Intracranial pressure- This is an indicator of the strength of the influence of cerebrospinal fluid, or cerebrospinal fluid, on brain tissue. Normally, its numbers range from 5 to 7 mmHg.
A condition in which it is significantly higher is called intracranial hypertension.
With increased intracranial pressure, symptoms and treatment in adult patients differ significantly from clinical picture and methods of therapy in children.
Since the bones of the skull lose flexibility with age, older patients are not at risk of developing hydrocephalus. However, constant compression of the brain can lead to no less serious consequences: episyndrome, loss of vision, stroke.
Is it possible to recognize the first signs of intracranial hypertension, and how to cope with this disease?
Increased intracranial pressure can be either chronic or acute.
It manifests itself with signs that may at first glance seem to have little connection with each other, and due to its polymorphism, this condition often goes unnoticed in the early stages.
The malaise is attributed to age problems, a consequence of overwork or stress, other somatic diseases.
The most important symptom of all the many signs, observed in almost everyone who suffers from increased intracranial pressure, is headache. It has a pressing character - the skull seems to be bursting from the inside, most often observed at night or in the morning, and becomes stronger with head movements and changes in body position.
Attacks of pain are often accompanied unpleasant sensations in the eyeballs, nausea and vomiting, which occurs due to compression of the nerves, are not relieved by analgesics and can be mistaken for a migraine attack. However, with migraine the pain is always one-sided, which is not the case with intracranial hypertension.
Another common symptom is deterioration and blurred vision, double vision. Compression and hypoxia of the optic nerves leads to their gradual death, which in advanced cases leads to blindness. Bruises form under the eyes that do not go away after rest.
Sometimes the pressure on the eyeballs is so strong that bulging eyes develop, which is characterized by the so-called setting sun symptom: the eyelids do not close completely, leaving a thin strip of the cornea exposed.
Less specific manifestations of intracranial hypertension include the following:
- increased fatigue and loss of strength;
- anxiety, depression;
- memory impairment;
- swelling of the face, especially the eyelids;
- dizziness when changing body position;
- hyperhidrosis of the feet and palms;
- changes in blood pressure, attacks of fever and sweating;
- paresthesia – increased sensitivity of the skin to temperature and touch;
- heart pain and bradycardia.
It is widely believed that intracranial hypertension goes away on its own over time and therefore does not require treatment. This is incorrect: only the idiopathic form of the disease is prone to spontaneous regression.
More often, this condition is a consequence of other disorders of the body, and without eliminating the immediate cause it only progresses.
Causes
 In some cases, the cause of increased intracranial pressure remains unclear.
In some cases, the cause of increased intracranial pressure remains unclear.
Idiopathic, or benign, hypertension usually occurs in children, adolescents, and obese women, and most often resolves within a few months. Treatment in this case can only be symptomatic.
More often, this condition, chronic or acute, is a consequence of other disorders of the body, and without eliminating the immediate cause it only progresses.
In order to identify the cause of increased ICP, a comprehensive examination is required: CT, MRI, EEG, lumbar puncture, which determines the amount of cerebrospinal fluid and the presence of pathogens in it, consultation with an endocrinologist, neurologist.

Brain image - intracranial pressure, hydrocephalus
The prognosis for the patient and the possibility of recovery from intracranial hypertension without serious consequences depends on the severity of his condition and the pathology that caused it. In some cases, physical therapy is sufficient, in others, surgery is required.
Constant compression of the optic nerves gives a very specific picture when examining the fundus, so often mild forms of chronic intracranial hypertension are detected during a routine examination by an ophthalmologist.
 Cerebral aneurysm is a dilatation of blood vessels in the brain, which can be congenital or acquired. - the most dangerous consequence of the disease.
Cerebral aneurysm is a dilatation of blood vessels in the brain, which can be congenital or acquired. - the most dangerous consequence of the disease.
Let's look at the symptoms of concussion in children.
Incorrectly prescribed procedures and herbal remedies often not only do not improve, but even worsen the patient’s condition. Therefore, self-medication and use without medical indications is not recommended.
Usually, the right therapy quickly helps you return to a healthy state. But even in cases where the disease has passed without a trace at first glance, it is recommended to undergo a preventive examination at least twice a year in order to avoid relapses.
Video on the topic
Increased intracranial pressure (ICP) – dangerous condition which many people face. It can occur in both childhood and adulthood. Women suffer from the disease somewhat more often than men. Unfortunately, sometimes the symptoms of increased intracranial pressure are not paid attention to, which leads to dire consequences. Therefore, it is necessary to know well what it is, the symptoms and principles of treatment of the disease in adults and children.
Causes of high ICP
Why does the pressure inside the skull increase? This phenomenon may be due to various factors. But in most cases, high intracranial pressure is associated with a violation of the outflow of cerebrospinal fluid from the cavity inside the skull.
First, it is useful to understand what intracranial pressure is. You should not think that inside the skull there is only a huge number of nerve cells and nothing more. A significant volume of the brain (more than a tenth) is occupied by cerebrospinal fluid, which is also called cerebrospinal fluid. It is mainly located in the area of the ventricles, located inside the skull, in its center. Also, part of the cerebrospinal fluid circulates in the space between the soft and arachnoid membranes of the brain. There is also cerebrospinal fluid in the spinal canal.
The functions performed by cerebrospinal fluid are varied. This includes protecting brain tissue from impacts on the skull bones, ensuring water and electrolyte balance and drainage from the brain. harmful substances and toxins. Another thing is important - the amount of cerebrospinal fluid determines the pressure inside the skull. Part of the cerebrospinal fluid (more than two thirds) is formed directly in the ventricles, and part is converted from blood circulating in the brain area. The liquor is completely renewed within a week.
Intracranial pressure is usually indicated in millimeters of mercury or millimeters of water. For adults, the normal value ranges from 3-15 mm Hg. Art. From a physics point of view, this parameter shows how many millimeters the cerebrospinal fluid pressure exceeds atmospheric pressure. In children, the pressure inside the skull is usually slightly lower than in adults. If the volume of cerebrospinal fluid circulating in the brain area becomes more than normal, this usually leads to increased intracranial pressure.
Increase in ICP above 30 mm. rt. Art. often leads to irreversible damage to brain tissue and death.
This is why it is important for people to know about ICP levels. But how to determine it, because, unlike blood pressure, ICP cannot be measured at home? To determine the pressure inside the skull, special instrumental methods which are carried out only in a hospital setting. Therefore, characteristic symptoms are often the reason for suspecting the diagnosis of “increased intracranial pressure”.
Symptoms of increased intracranial pressure
When intracranial pressure increases, symptoms typically include a number of commonly observed signs:
- visual disturbances,
- dizziness,
- absent-mindedness,
- memory impairment,
- instability of blood pressure (hypertension or hypotension),
- nausea,
- vomit,
- lethargy,
- fast fatiguability,
- sweating,
- chills,
- irritability,
- mood swings,
- increased skin sensitivity,
- pain in the spine,
- breathing disorders,
- dyspnea,
- muscle paresis.
If you experience any of these signs from time to time, then, naturally, this is not evidence of increased intracranial pressure. Symptoms of increased pressure inside the skull may be similar to symptoms of other ailments.
The most common symptom indicating the disease is headache. Unlike migraine, it affects the entire head at once and is not concentrated on one side of the head. Most often, pain with high ICP is observed in the morning and night hours. Pain with increased intracranial pressure can intensify when turning the head, coughing, sneezing. Taking analgesics does not help relieve pain.
The second most common symptom of increased intracranial pressure is problems with visual perception - double vision, blurred objects, decreased peripheral vision, attacks of blindness, fog before the eyes, decreased reaction to light. These signs of increased intracranial pressure are associated with compression of the optic nerves.
Also, under the influence of increased ICP, the patient’s shape may change. eyeball. It may bulge so much that the patient is unable to close the eyelids completely. In addition, blue circles made up of congested small veins may appear under the eyes.
Nausea and vomiting are also common symptoms of increased intracranial pressure. As a rule, vomiting does not bring relief to the patient.
It should be borne in mind that intracranial pressure may increase for a short time (2-3 times) and in healthy people– for example, when coughing, sneezing, bending, physical activity, stress, etc. However, the ICP should quickly return to normal. If this does not happen, then this is evidence of a chronic increase in intracranial pressure.
Signs of increased intracranial pressure in young children
How does the disease manifest in young children? Unfortunately, infants cannot tell their parents about their feelings, so they have to rely on indirect symptoms of intracranial pressure. These include:
- lethargy;
- cry;
- poor sleep;
- vomit;
- seizures;
- involuntary eye movements;
- swelling and pulsation of the fontanelle;
- increase in head size (hydrocephalus);
- uneven muscle tone – some muscles are tense and some are relaxed;
- protrusion of a network of blood vessels under the scalp.
On the other hand, symptoms such as nosebleeds, stuttering, occasional shuddering during sleep, and increased excitability, as a rule, do not indicate increased pressure inside the child’s skull.
Diagnosis of increased intracranial pressure
To directly measure pressure inside the skull, complex instrumental methods that require highly qualified physicians, sterility and appropriate equipment are used, which are often unsafe. The essence of these methods is puncture of the ventricles and insertion of catheters into the areas where cerebrospinal fluid circulates.
A method such as puncture of cerebrospinal fluid from the area is also used. lumbar region spine. In this case, both pressure measurements and a study of the composition of the cerebrospinal fluid can be carried out. This method is necessary if there is reason to suspect the infectious nature of the disease.
Safer diagnostic methods have become more widespread:
- ultrasonography,
- CT scan.
As a result of these studies, it is possible to identify changes in the structure of the brain and surrounding tissues, indicating increased intracranial pressure.
These changes include:
- increase or decrease in the volume of the ventricles of the brain,
- swelling,
- increasing the space between the shells,
- tumors or hemorrhages,
- displacement of brain structures,
- dehiscence of the sutures of the skull.
Important diagnostic method also is encephalography. It allows you to determine disturbances in the activity of various parts of the brain characteristic of increased ICP. Doppler ultrasound of blood vessels helps to detect blood flow disturbances in the main arteries and veins of the brain, congestion and thrombosis.
An important diagnostic method is fundus examination. In most cases, it can also detect increased intracranial pressure. At this syndrome Symptoms such as enlargement of the vessels of the eyeball, swelling of the place where the optic nerve approaches the retina, and small hemorrhages on the retina appear. After determining the degree of development of the disease, the doctor must inform the patient about how best to treat it.
Causes of increased intracranial pressure.
What causes increased ICP in an adult? Here we must take into account that increased intracranial pressure is usually secondary symptom, and not an independent disease.
Factors that can lead to increased intracranial pressure include:
- inflammatory processes of the brain and meninges (encephalitis, meningitis);
- obesity;
- hypertension;
- hyperthyroidism;
- dysfunction of the adrenal glands;
- liver pathologies causing encephalopathy;
- osteochondrosis cervical spine spine;
- tumors in the head area;
- abscess;
- cysts;
- helminthiasis;
Also, increased intracranial pressure can appear as a result of infectious diseases, such as:
- bronchitis,
- mastoiditis,
- malaria.
Another one possible reason occurrence of the syndrome - taking certain medications.
These include:
- corticosteroids,
- antibiotics (primarily tetracyclines),
- hormonal contraceptives.
Factors leading to high intracranial pressure can either provoke increased generation of cerebrospinal fluid, disrupt its circulation, or interfere with its absorption. Three mechanisms for the occurrence of the syndrome may occur at once.
Hereditary predisposition should also be taken into account this disease. In infants, the main factors contributing to the onset of the disease are birth injuries, fetal hypoxia, toxicosis during pregnancy and prematurity. Lack of oxygen during an unfavorable pregnancy can lead to a compensatory increase in cerebrospinal fluid production and, ultimately, to hydrocephalus.

Photo: Roman Samborskyi/Shutterstock.com
Complications
Chronic increased intracranial pressure, contrary to popular belief, tends to progress. Without proper treatment, the disease can lead to serious consequences leading to disability.
Such complications include:
- stroke;
- impaired coordination of movements as a result of damage to the cerebellum;
- impaired reflexes, arrhythmias as a result of compression of the brain stem;
- paralysis;
- speech disorders;
- psychical deviations;
- blindness;
A common result of the development of the disease is death.
However, a benign form of the disease is also quite rare, in which the symptoms of increased ICP go away on their own, without any treatment. Associated with the presence of this form of the disease is the misconception that the disease goes away on its own. But that's not true. The fact is that, as a rule, the benign form of the disease is typical only for young women, who are often overweight. So you shouldn’t rely on the fact that you have a benign form of the disease. It is best to consult a doctor.
Treatment of increased intracranial pressure
What to do if this diagnosis is established? If the increase in intracranial pressure is a secondary process, then first of all it is necessary to eradicate the primary disease - atherosclerosis, hypertension, osteochondrosis, hormonal imbalances. However symptomatic therapy increased intracranial pressure is also extremely important.
Once high intracranial pressure is detected, treatment should be prescribed by a doctor. There are several ways to treat increased intracranial pressure. They are divided into conservative and surgical.
Conservative methods of treating increased intracranial pressure include, first of all, taking medications. The goal of therapy is in this case is a decrease in cerebrospinal fluid pressure, increasing the outflow of blood from the brain.
The main group of drugs that are indicated for increased intracranial pressure are diuretics, for example, Furasemide, Diacarb. If tumors are present or meningitis is detected, steroidal anti-inflammatory drugs are prescribed to reduce swelling. Also taken are drugs that improve venous blood flow, potassium supplements (Asparkam). Studies have shown that nootropic drugs are ineffective in increasing intracranial pressure.
If increased intracranial pressure is caused by some other disease, then drugs are used to treat the underlying disease.
Also, when treating high ICP in adults, physiotherapy can be used (in particular, magnetic influence on the collar area, electrophoresis with medicinal substances), massage of the cervical-collar area and spine, physical therapy, acupuncture, and a circular shower. These methods are used mainly in mild cases of increased ICP, when there is no direct threat to life. Also, for the purpose of prevention, the patient can carry out a daily massage of the areas of the back of the head, neck, and base of the skull.
In severe cases of the disease, surgical operations. Currently, the most common type of surgery is bypass surgery. This is the name given to the insertion of a tube through which excess cerebrospinal fluid is pumped out of the cerebral ventricles into the abdominal cavity. This method, however, also has disadvantages, such as the fact that the catheter can become clogged and fail. In addition, this method has a high risk of complications. Children will need to lengthen the tube several times as they grow. Also, the cerebrospinal fluid can be drained into a special sterile container. A method may also be used to drain cerebrospinal fluid from the ventricles into the space between the membranes at the base of the brain. In this case, the risk of complications is minimal.
As aid with high pressure in the head, methods can also be used traditional therapy, in particular, tinctures of herbs - hawthorn, motherwort, eucalyptus, mint, valerian. They provide a calming effect and relieve vascular spasms.

Photo: Oxana Denezhkina/Shutterstock.com
Diet is of great importance. First of all, when ICP increases, it is necessary to reduce the volume of daily fluid intake to 1.5 liters. You should also take more foods containing potassium and magnesium salts - seaweed, buckwheat, beans, dried apricots, kiwi. At the same time, consumption should be reduced sodium salt, meat products, especially animal fats, confectionery products. You should monitor your weight, since excess weight is also one of the factors that provokes the onset of the disease.
During the absence of exacerbations, the patient is recommended to exercise physical culture. A good preventive measure is jogging and swimming. With this diagnosis, overheating of the body, baths, smoking and alcohol are contraindicated. An increase in temperature above +38 ºС poses a danger for those suffering from increased ICP, therefore in such cases it is necessary to take antipyretic drugs. It is necessary to maintain a daily routine, ensure sufficient time for sleep and rest, and minimize brain strain when watching television.
Intracranial pressure is a very significant indicator in the diagnosis of pathology of the nervous system, in the nature of the course of diseases not only of the brain, but also of the spinal cord. This type of hypertension reflects the level of pressure of the fluid located in the ventricles of the brain circulating through the spinal canal.
It is possible to measure intracranial pressure quantitatively only by puncture of the canal or ventricles of the brain. Not every doctor is able to perform the procedure correctly. It is not performed on an outpatient basis, only in a hospital setting. There are situations when specialists from neurosurgical clinics or departments have to be called for consultation and spinal puncture.
Difficulties arise at the stage of assessing the indicator. The interpretation of increased intracranial pressure is complicated by the large “swings” of the indicator: in mm of water column – 60–200, in mm of mercury – 3–15. It is impossible to replace the measurement with computed tomography or magnetic resonance imaging. These techniques reveal only indirect signs of hypertension inside the skull.
What anatomical structures are responsible for maintaining normal intracranial pressure?
To protect brain tissue, humans have three membranes:
- soft,
- arachnoid (arachnoid),
- hard.
About 1/10 of the volume of the adult skull (150 ml) is filled with cerebrospinal fluid (CSF). Its main purpose:
- maintain the necessary balance of water and electrolytes in nerve cells;
- provide food;
- protect immobile structures of the spinal cord.
70% of the fluid is formed in the glandular cells of the cerebral ventricles, the so-called internal cavities of the brain (2 lateral, third and fourth). Up to 30% of the volume is replenished due to the release of the liquid part of the blood from the vessels into the cavity of the ventricles. A complete update occurs every 7 days.
The common collector is the fourth ventricle. In it, the fluid collects and passes through a special hole into the space between the soft and arachnoid membranes (subarachnoid).
In the deep grooves and crevices of the brain substance, in the base area there are 6 liquor cisterns. Fluid drains here from the fourth ventricle and is absorbed by the cells. Unnecessary residues return to the venous vessels of the brain.
What happens when the circulation mechanism is disrupted?
Circulation failure is possible due to violations at any stage:
- change in production by glandular cells;
- increased output from the arteries;
- mechanical obstacle to free flow in the ventricles;
- reverse suction.
As a result, an excess volume of fluid is retained inside the skull, which stretches the meninges and compresses the soft tissue structures. This is manifested by pathological symptoms such as increased intracranial pressure.
In the clinic, it is important to distinguish a physiological increase in intracranial pressure from the manifestation of diseases. An increase in the indicator is detected when:
- stress;
- tilting the head forward;
- screaming, crying (in a child);
- after straining against the background of lifting weights.
Hypertension in the skull normally increases almost three times without any symptoms of pathology. The decrease occurs spontaneously, and is therefore called benign intracranial pressure. It is believed that similar normal indicator present in 70% of newborns.
It is impossible to perform a puncture on a frightened baby
Intracranial pressure in adults responds to alcohol intake and increased workload during pregnancy. To distinguish physiological reasons from possible pathology, it is necessary to exclude diseases with damage to brain structures.
What pathological causes cause increased intracranial pressure?
It is impossible to treat a patient without knowing why the symptoms that bother him arise. Let's consider how intracranial pressure is affected by disrupted fluid circulation mechanisms.
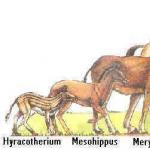
One of the reasons is congenital anomalies. This applies to altered venous sinuses and hydrocephalus. Due to the reduction in the absorption of cerebrospinal fluid, it accumulates in the ventricles, compressing adjacent tissues and structures. IN childhood the size of the skull increases, the sutures between the bone components diverge.
Pathology of pregnancy and labor activity:
- severe toxicosis;
- fetal asphyxia due to umbilical cord entanglement;
- protracted labor with weakened uterine tone.
The fetus experiences an acute lack of oxygen. In this case, increased production of cerebrospinal fluid is a reflex defense mechanism.

Inflammation of the meninges is caused by infectious pathogens
Infectious diseases with brain damage:
- meningoencephalitis (the source may be ticks, bacterial and viral infection);
- neurosyphilis (one of the forms of the chronic syphilitic process).
Any inflammation is accompanied by edema and swelling of brain tissue. Plasma is discharged through the wall of blood vessels into the cerebrospinal fluid. Its volume increases significantly. In addition, the usual infectious diseases interfere with absorption, which further increases the already elevated intracranial pressure. This mechanism is observed when:
- flu,
- bronchitis,
- inflammation of the middle ear,
- malaria,
- enteritis,
- mastoiditis.
High arterial hypertension of any kind causes an increased discharge of the liquid part of the blood from the vascular bed of the brain into the cerebrospinal fluid.

With increased blood pressure, intracranial hypertension simultaneously increases
Impaired venous tone with chronic failure helps reduce blood outflow and fluid stagnation in brain tissue. Changes cerebral circulation do not pass without leaving a trace for structures affecting intracranial pressure.
In this case, the internal cavities of the ventricles stretch, compressing the surrounding tissues. The nutrition of neurons is disrupted.
Increased intracranial pressure occurs as a result of the negative effects of certain medications. These include:
- group of corticosteroids (Hydrocortisone, Prednisolone);
- antibiotics (Tetracycline and its analogues);
- Biseptol;
- nitrofuran derivatives (Furazolidone, Furadonin);
- hormonal contraceptives.
The action of the drugs can cause the effect of a false tumor with cerebral edema and typical consequences.
Endocrine diseases are often accompanied by increased blood pressure, followed by intracranial hypertension. The process is especially characteristic of pathologies associated with growth thyroid-stimulating hormone and estrogens. Detected when:
- hyperthyroidism,
- obesity,
- adrenal insufficiency;
- encephalopathy with liver damage.
Among the causes, one cannot miss brain damage due to:
- skull injuries (open and closed type);
- suffered a stroke;
- surgical interventions.
Blood entering the subarachnoid space damages the villi that absorb fluid into the veins of the skull. Thrombosis occurs with venous stagnation.
What are the causes of low intracranial pressure?
The main reason for the decrease in cerebrospinal fluid pressure is skull trauma, damage to the meninges with fluid leaking out. This mechanism is equally typical for adults and children. Similar action specifically achieved during therapeutic drainage of the ventricles of the brain or during lumbar puncture during brain surgery.
Other reasons are:
- prolonged spasm of cerebral vessels;
- chronic fatigue syndrome;
- avitaminosis;
- uncontrolled use of diuretics with subsequent dehydration;
- chronic intoxication with alcohol, drugs, medications;
- manifestation of severe allergic reaction;
- infectious diseases;
- osteochondrosis of the spine in the cervicothoracic and thoracic regions;
- heart and vascular diseases accompanied by hypotension;
- endocrine disorders, causing disturbance normal hormonal balance (during pregnancy, during menstruation, before menopause).
As you can see, the list of reasons for increased and decreased intracranial pressure partially coincides. This confirms the individual reaction of each person.
Symptoms of increased intracranial pressure
Most common symptom, indicating cerebral hypertension are headaches. They are caused by high sensitivity arachnoid to stretching.

Patients note that the headache is much worse when turning and bending, in cases of coughing and sneezing
This is explained by adding physiological mechanism aggravating the patient's condition. Important Feature- increased pain in the morning. The symptom is caused by prolonged horizontal position of the body at night. At the same time, the production of cerebrospinal fluid increases, and the outflow becomes more difficult.
To less permanent clinical manifestations relate:
- nausea, independent of food, may result in gushing vomiting, which does not bring relief, since it is associated with irritation of the center in the medulla oblongata;
- sweating - has a paroxysmal nature, accompanied by chills (a consequence of damage to the autonomic nodes of the nervous system);
- under the patient's eyes there are persistent dark circles, they are not associated with pigmentation, but are caused by overflow and stagnation of the venous network of the skin of the lower eyelid;
- visual impairment in the form of double vision and narrowing of fields is transient.
Focal neurological manifestations and changes mental status often come to the fore after headaches.
The patient notes:
- increased irritability;
- increased fatigue;
- apathy;
- unstable mood.
These manifestations depend on the force of compression of the cortical centers and medulla oblongata, the area of the hypothalamus responsible for the formation of emotions.
Sometimes the patient is bothered by back pain. They indicate increased pressure in the spinal canal. If the damage concerns specific motor centers and cell nuclei, then the patient is found to have weakening (paresis) of muscles in one or two limbs, in half of the body, and loss of sensitivity.
Sometimes patients note a feeling of suffocation, lack of air, not associated with physical activity. The symptom may indicate compression of the medulla oblongata.
Doctors of various specialties take part in the diagnosis. The identification of focal symptoms and their localization is determined by a neurologist. An ophthalmologist examines the fundus of the eye using an ophthalmoscope. In favor high blood pressure says detected disc edema optic nerve, a picture of venous stagnation.
Benign intracranial hypertension
Benign or pseudotumor hypertension inside the skull - rare pathology. It most often affects people aged 30 to 40 years. It is known that women suffer from it 8 times more often than men. Overweight is observed in most young patients.
The reasons are not exactly known. Among the provoking factors:
- obesity;
- pregnancy with eclampsia;
- violation menstrual cycle;
- endocrine diseases(reduced parathyroid function, Addison's disease, diabetic ketoacidosis);
- poisoning with salts of heavy metals (lead, arsenic);
- scurvy;
- medications (except for those already listed, vitamin A, psychotropic drugs);
- chronic renal failure;
- blood diseases (leukemia, anemia, hemophilia, thrombocytopenic purpura);
Intracranial hypertension is regarded as secondary, associated with the listed factors. A significant proportion of cases are considered idiopathic (of unclear origin).
Headache (90%) of varying intensity is the main clinical symptom, it was noted in 90% of patients.
Up to 75% of patients have vision changes; they usually precede a headache.
Distinctive feature pathology is self-normalization of pressure; no treatment is required. However, relapses occur in 40% of cases.
Diagnostics
Only the attending physician can decide which diagnostic method to give preference to.

Spinal tap is considered the most informative method diagnostics
To identify increased intracranial pressure, a comprehensive examination is necessary. Applicable:
- puncture of the spinal canal with measurement of the indicator;
- magnetic resonance imaging;
- CT scan;
- electroencephalography.
Electroencephalography and ultrasound methods allow us to indirectly judge possible disorders associated with increased pressure inside the skull. Not all methods are used in clinics. The local therapist should determine their feasibility and refer them to the right institution.
Treatment
Treatment of increased intracranial pressure should first of all be aimed at eliminating the causes that caused and maintained the pathology.
If there is no threat of compression of brain tissue, then a course of drug therapy, physical therapy, massage, and physiotherapy is quite sufficient.
Three classes of medications are considered effective:
- Anti-inflammatory drugs (antibiotics, corticosteroid hormones) - have a targeted effect on microorganisms, reduce allergic mood, eliminate tissue swelling and intoxication.
- Diuretics (Lasix, Diacarb) - reduce the production of cerebrospinal fluid by reducing chlorine-containing salts in the blood.
- Potassium preparations (Panangin, Asparkam) - affect cellular metabolism, especially indicated for cerebral hypertension caused by stroke, impaired venous circulation.
- Notta and Neurohel (advertised homeopathic remedies);
- Piracetam, Picamilon, Nootropil, Encephabol (nootropics);
- Cavinton, Vinpocetine, Cinnarizine and Sermion (from the group of venotonics).
Their use in cerebral hypertension has shown a lack of effectiveness.
Physiotherapeutic methods
Reliable ways to reduce cerebral hypertension for many years are:
- Electrophoresis with Eufillin solution - injected into the vessels through the electrodes of the collar zone medicinal substance, which improves the nutrition of brain cells, relieving hypoxia and its consequences.
- Magnetotherapy, also through the collar zone, relieves cerebral edema and restores blood supply.
- The massage is performed in the spine and cervical region. It is recommended to first complete a course of 15–20 procedures, then perform self-massage in a circular motion twice a day for 10 minutes.
- Exercise therapy exercises are aimed at relieving tension in the neck muscles. Eliminating their spastic contraction helps reduce pressure on the vessels responsible for the outflow of blood from the brain. Acupuncture sessions are conducted for the same purpose.

A pair of electrodes is located in the collar area, this helps to normalize the functioning of blood vessels, wall tone, and ensures the necessary circulation of cerebrospinal fluid
Balneotherapy is actively used with the appointment oxygen baths, circular shower. These techniques affect reflex zones using temperature and massage with oxygen bubbles, which allows you to restore sensitivity and mental abnormalities.
When is surgery necessary?
Surgical intervention required to treat the threat of compression of vital centers in brain tissue. Neurosurgical operations to remove space-occupying formations (cysts, tumors) are carried out in specialized institutions under the control of magnetic resonance equipment. They consist in the formation of a complex system for draining cerebrospinal fluid from the cranial cavity into blood vessels, into the heart cavity, peritoneum.
Therapeutic spinal punctures also belong to surgical methods. They help in an emergency to relieve high blood pressure by pumping out some of the fluid.
Modern endoscopic operations are performed with a rigid apparatus through the created hole using craniotomy. The essence of the operation is to insert an endoscope into the third ventricle of the brain, “drilling” its bottom and forming an additional path for the outflow of cerebrospinal fluid through the venous cistern located underneath.
Treatment with folk remedies
Doctors consider it possible to use folk remedies if a clear connection has been established between increased cerebrospinal fluid pressure and osteochondrosis, obesity, venous insufficiency, frequent stressful situations. Herbal decoctions and tinctures are recommended that improve blood circulation and reduce the production of cerebrospinal fluid.
In the summer, young mulberry branches are collected, chopped into small pieces and dried. The decoction is prepared by boiling two tablespoons of the raw material in a liter of water for a quarter of an hour. Then you should leave it for another hour. The product contains a large amount of vitamins, antioxidants, and microelements. It is recommended to take a glass three times a day. Healers promise a reduction in headaches after a week of treatment.
- hawthorn tinctures,
- motherwort,
- valerian,
- peppermint,
- eucalyptus.
They are mixed and stored in a dark glass bottle. You can add a few sticks of cloves and let it brew for another 2 weeks. Take 20 drops on a piece of sugar before meals or dilute with water. It is recommended to be treated in monthly courses with breaks.
A decoction of black poplar buds has a diuretic and calming effect. You need to brew 2 tablespoons per 0.5 liters of water in a thermos. Take half a glass before meals during the day.
In cases of mechanical obstruction caused by a tumor, folk recipes may not only be useless, but also have a harmful effect on the cause of the disease. Therefore their use is not indicated.
What is the risk of increased intracranial pressure for a patient?
It has been proven that a single excess of cerebrospinal fluid pressure over the limit of 400 mm of water column compresses blood vessels and tissue so much that all metabolic processes stop, and a variety of ischemic stroke with the death of neurons.
Chronic long-term elevation most often “disables” the cerebellar structures. This manifests itself in vestibular disorders, paresis, and changes a person’s behavior and emotions.

Vestibular disorders include unsteady gait, sudden dizziness
When the structures of the brain stem are damaged, the ventricles, pons, and wedging occur upper sections in the hemispheres, infringement of the lower zones in the foramen magnum. Typical manifestations develop:
- bradycardia;
- muscle tone decreases;
- decreased body temperature;
- pupils dilate in the absence of reaction to light;
- reflexes change.
Compression of the optic nerve can cause complete visual impairment, including irreversible blindness. Attentive attention to the signs in the fundus allows you to anticipate complications in advance and eliminate them.
Epileptiform seizures occur when certain areas of the brain are activated. Seizures, unlike true epilepsy, proceed more favorably.
Any signs of increased intracranial pressure require timely adoption of therapeutic measures and identification of the causes. To do this, you should not endure headaches; you should contact your therapist. If consultations with other specialists are necessary, they should be planned in the examination plan.
People quite often do not pay attention to headaches. In a sense, this is facilitated by modern medicines, allowing you to drown out unpleasant sensations.
But everyone should understand that its appearance is a signal from the body, indicating that not everything is okay with you. Quite often in such patients, the main cause of discomfort is increased intracranial pressure. Symptoms in adults, treatment methods - read about all this in our review.
What is intracranial pressure
Liquor is cerebrospinal fluid, the excess of which can put pressure on the human brain. It is formed in clusters of small vessels called the “sacs” of the human brain.
And it is the pressure of this fluid that has become commonly called intracranial. If there is little cerebrospinal fluid, then the pressure inevitably decreases, but if there is too much of it, then this is exactly the case when doctors diagnose increased intracranial pressure. Symptoms in adults are extremely unpleasant. And this is a dangerous disease.
A healthy person is characterized by a stable level of fluid in the body, without obvious predominance in one direction or another.

Increased intracranial pressure: symptoms in adults
In addition to high blood pressure itself, this problem has a number of associated symptoms. How does the increased manifestation in adults manifest as follows:
- headache noticeably worsens in the evening and at night;
- constant feeling of nausea, but no vomiting;
- a person feels weak and lethargic, he becomes irritable much faster;
- the pupil of the eye does not react to light, and the patient himself has “floaters” flashing in his eyes;
- one side of the body suddenly loses muscle strength, which strongly resembles paralysis.
Intracranial pressure headaches often become more severe with sneezing and coughing. The same should be expected from bends.
In such cases, if the pain area is unclear, you can expect the pain to intensify not in the evening, but in the morning.
Pressure has a significant effect on the optic nerve. The consequences of this can be temporary blindness, fog before the eyes and other manifestations that prevent a person from leading a full life.
Even mentally stable people experience discomfort during attacks of high blood pressure. They may experience nervous breakdowns and long periods of depression. The person becomes lethargic, leads a passive lifestyle and quickly gets irritated.
Frequent lower back pain can also be one of the manifestations of the disease.

How to be treated
If you have increased intracranial pressure, treatment should not be delayed until long box. You need to urgently seek help from a specialist. Methods of therapy depend quite strongly on the reasons for the appearance of such high pressure. Much also depends on the age of the patient who consults the doctor.
The main methods of treatment are taking drugs that affect blood vessels, as well as sedatives and diuretics.
In addition, manual therapy and gymnastics are prescribed.
The patient is put on a specific diet, the essence of which is to consume foods rich in vitamins. Should be avoided large quantity liquids and salts.
In especially severe cases, drainage and insertion of shunts are indicated - this is necessary to reduce the amount of cerebrospinal fluid.
How to reduce intracranial pressure yourself
If an illness catches you at the wrong time, you can always cope with it at home. You shouldn’t count on a complete cure, but you can alleviate most symptoms are quite real. So,
Diuretics play an important role in self-medication, such as tincture of hawthorn, rose hips, lavender, etc. They provoke a decrease in intracranial pressure.
It is worth noting that before taking herbal tinctures, you must consult your doctor.
Also, massage of two points on the back of the head is quite effective. To use it, you need to clasp your head with your hands so that thumbs ended up exactly on the back of the head. After this, you need to make circular movements for several minutes.

Tablets for intracranial pressure
Of course, drug therapy is also used in the treatment of intracranial pressure. It is necessary to pay attention to the fact that drug treatment must be carried out under the supervision of a doctor. Otherwise, you should expect negative and even fatal consequences.
The usual practice in such cases is to prescribe diuretics like Furosemide or Veroshpiron. If the condition has a negative impact on the patient’s optic nerve, then he is prescribed corticosteroid tablets for intracranial pressure, for example Prednisolone or Dexamethasone.
Traditional treatment
Is it possible to traditional treatment intracranial pressure? Alternative medicine is quite effective, but its main disadvantage is that it only weakens the symptoms that appear. Actually cure intracranial pressure with folk remedies almost impossible. They should be used in cases where it is not possible to get an appointment with your doctor.
The main weapon against all ailments is herbal infusions and decoctions. Mainly used are valerian, sage and St. John's wort.
Having selected medicinal herbs, they should be filled with boiling water. It is necessary to make sure that no more than one tablespoon of herbs was taken. You need to drink the infusion for one month, drinking a quarter glass three times a day. After a course of herbs, you should take a break from them for a significant period of time.
There are other options. Alcohol tincture is very popular remedy among the people. You need to take dried clover flowers as a base, fill exactly half the jar with them, and fill them to the very top with alcohol or vodka. After this, the tincture should be placed in a dark and cool place for two weeks.
When it is ready, you can take it two times a day, one teaspoon, after diluting it with water.
And finally, garlic tincture is a good remedy for headaches. To make it, you need to take three lemons and pass them through a meat grinder along with the skin. Add three chopped heads of garlic to the resulting mixture.
After this, the drug should be allowed to settle, and only then you can start taking the medicine in small doses and several times a day.

Intracranial pressure. Which doctor should I contact?
What kind of doctor treats this unpleasant and potentially dangerous illness? First you have to go to a therapist to eliminate all possible options. After this, they must issue a referral to a neurologist, but he already knows very well what to do with the disease.
You should not expect that the doctor will be able to cure intracranial pressure instantly. First, you will need to undergo many examinations, including an MRI and an encephalogram. After making sure that you do not have other brain pathologies, the doctor can begin standard treatment procedures.
The need for examination by a therapist is high, since he needs to cut off many other possible diseases. This is very important, because the faster you can start proper treatment, the easier it will be to overcome the disease.

Medicines for increased intracranial pressure
Some drugs fight the manifestations of intracranial pressure, while others are aimed at the root cause of the disease.
Medicines for increased intracranial pressure in adults are primarily diuretics. Their main purpose is to help the body get rid of excess liquid. The less it is, the faster the pressure will drop.
For example, the drug "Gritserol" effectively copes with this task.
In addition, drugs that expand vascular system person. For example, one of the most widespread options is magnesia. It also has an antiarrhythmic effect.
Among some doctors, it is common practice to treat internal cranial pressure according to a certain scheme, which includes nootropics and tablets that help stabilize the blood circulation in the brain.
The most common choice of doctors is “Nootropil”, “Pirocetam” and “Phenotropil”. Their main goal is to normalize the patient’s thought process and at the same time help him cope with intellectual stress.
"Sermion" and "Cavinton" are already drugs that affect blood circulation. It is worth recalling once again that only a doctor can choose the right pills and determine the dosage. Self-medication in such a delicate area of medicine can lead to consequences that no doctor can reverse.

When to see a doctor
Measuring normal pressure is not the slightest difficulty, but when it comes to intracranial pressure, many people fall into a stupor. And there is a reason.
Most effective method Finding out if there is a problem is a puncture. The doctor takes a needle connected to a pressure gauge and then inserts it into the spinal canal. All this requires careful preparation of the patient, which is only available in a hospital setting.
These are not all options. More expensive - MRI. It costs a lot of money, but is no less accurate, and there is no need to insert any needles or anything else that could frighten the patient. And yet, most often, doctors make do with electroencephalography. With its help, you can identify changes in the pattern of brain activity, which is also evidence higher level pressure in the brain.
If you once find yourself with an unreasonable headache and nausea, do not delay, consult a doctor. It may be possible to prevent the disease before it progresses to more serious phases.
Causes of the disease
Intracranial pressure, the symptoms and treatment of which we have examined, can be caused by many factors, but most often such a condition is observed in cases congenital pathologies and for a variety of inflammations, for example, meningitis and encephalitis.
People who are overweight are at risk. So healthy vitamin At the same time, it is a substance that can significantly increase your blood pressure, but this is only possible if there is an excess of retinol in the body.
Intoxication is another reason for the occurrence of the disease. Impact toxic substances has a detrimental effect on normal work brain. As a result, serious organic damage can occur.
Intracranial pressure in children
Children are just as likely as adults to get it. unpleasant disease, which ultimately can have a very negative impact on their level of development and future success in life. Apathy, drowsiness, excessive sensitivity, in in some cases even squint. All this does not contribute to the learning process and prevents the child from being active and inquisitive.

Consequences of intracranial pressure for a child
The child runs the risk of becoming depressed, he inevitably falls behind in his studies, does not want to go out with his peers, avoids new acquaintances, and even locks himself in his room because he does not want to participate in any of the activities.
Increased intracranial pressure (symptoms and treatment of the disease depend on the presence concomitant diseases) can be found even in infants. Because of it, children learn to hold their heads up, walk and even talk late. Therefore, it is not recommended to skip or ignore a routine examination by specialists, including a neurologist.
To prevent such a misfortune from happening to your child, you should listen carefully to their complaints (we are, of course, talking about older children, not babies) and, if necessary, take them to the doctor in a timely manner.
Symptoms of intracranial pressure in children
In children, the disease manifests itself in its own way, but there are also general symptoms. Anxiety and fatigue, severe headaches, nausea and vomiting, squint - all this is what you should pay attention to during the period of child growth.
In very small babies, the shape of the head may become deformed and the volume of the head may increase; regurgitation is observed too frequently, and this does not even depend on meals. The child generally behaves more restlessly than other children. And finally, the monotonous scream is another evidence that small organism suffers from increased intracranial pressure.
Intracranial pressure is an accumulation or lack of cerebrospinal fluid in a certain part of the skull, caused by a violation of its circulation.
The name of the liquid is liquor. It is located in the ventricles of the brain, in the spinal cavity, as well as in the space between the bones of the skull, bone marrow and brain. Liquor protects the “gray matter” from severe overloads and mechanical damage.
The liquid is always under a certain pressure. It is constantly updated, circulating from one area to another. The process usually takes about seven days. But sometimes it is disrupted and cerebrospinal fluid accumulates in one place. Increased intracranial pressure occurs. If there is a decrease in cerebrospinal fluid, then decreased intracranial pressure occurs.
A decrease often occurs after a head injury, with brain tumors, with prolonged vasoconstriction, and also due to long-term use of diuretics.
Causes
The main causes of ICP are:
- Violation of metabolic processes in which liquid is poorly absorbed into the blood;
- Spasmodic vessels through which cerebrospinal fluid cannot circulate normally;
- Excess fluid in the body, causing the amount of cerebrospinal fluid to increase;
- Brain hypoxia;
- Meningitis;
- Encephalitis;
- Tumors;
- Excess weight;
- Severe poisoning;
- Excess vitamin A.
Symptoms of intracranial pressure:

When is surgery necessary?
- If a skull injury has occurred. Due to the impact, a hematoma may occur, which will provoke an increase in intracranial pressure;
- Severe headache and fainting. In this case, most likely, a vascular aneurysm ruptured.
You should always treat intracranial pressure rather than wait until an accident occurs.
Symptoms
“speaks” an increased head size, strabismus. In school children and preschool age fatigue, irritability, and increased sensitivity appear.
Diagnostics
Doctors determine the presence of a problem using many data, including:
- Stagnation of the optic nerve head;
- Impaired outflow of venous blood.
In addition, adults and older children undergo computed tomography and magnetic resonance imaging, and infants are examined using ultrasound of the skull through the fontanel.
Another method is to insert a special needle with a pressure gauge into the spinal canal or fluid cavities. This procedure is far from safe and should only be performed by highly qualified doctors.
To establish an accurate diagnosis, it is advisable to use all of the diagnostic methods listed above. The main ones remain MRI and X-ray computed tomography.
Treatment
 Increased intracranial pressure is a serious threat to the patient's life. Regular pressure on the brain disrupts its activity, as a result of which intellectual abilities may decrease and the nervous regulation of the functioning of internal organs may be disrupted.
Increased intracranial pressure is a serious threat to the patient's life. Regular pressure on the brain disrupts its activity, as a result of which intellectual abilities may decrease and the nervous regulation of the functioning of internal organs may be disrupted.
If the diagnosis reveals serious abnormalities, treatment should take place in a hospital setting.
If a tumor occurs, it is removed. If present, operations are performed to drain the fluid; in case of neuroinfections, antibacterial therapy is prescribed.
The main thing is not to self-medicate. As soon as you feel unwell, immediately visit a doctor and get competent recommendations.
If there is no high threat to the patient's life, symptomatic treatment is prescribed. drug treatment, aimed at normalizing intracranial pressure.
Diuretics
The most commonly used are diuretics, which speed up the process of excretion of cerebrospinal fluid and improve its absorption. Treatment with such drugs is carried out in courses. If the disease recurs frequently, they are taken constantly, but at least once every seven days.
Sedatives and vascular drugs
If prescribed by a doctor, you can inject nootropic drugs that improve nutrition and blood circulation in the brain. To normalize blood pressure, massage sessions are often performed; patients go swimming and improve their health.
If there are no serious complications, you can do without medications. Instead it does:
- Manual therapy;
- Osteopathy;
- Gymnastic exercises.
It is also worth thinking about normalizing your drinking regime.
How to measure intracranial pressure?
Intracranial pressure can be measured by inserting a special catheter into the lateral ventricle of the brain, where the cerebrospinal fluid is located. This method is considered to be the most accurate.
If the pressure is high, it can be reduced by pumping out some of the cerebrospinal fluid.
Another method is to use a subdural screw. It is inserted into a hole in the skull. This device allows you to measure pressure in the subdural space.
Epidural sensor
The sensor is inserted between the dural tissue and the skull. To do this, the hair is shaved off the head and the skin is treated with an antiseptic. After this, an incision is made and the skin is pulled back so that the “skull box” becomes visible. The final stage is entering the sensor. It is necessary to measure pressure only in extreme cases.
Consequences
If measures are not taken to normalize blood pressure, the disease will take a chronic form. This is fraught with the occurrence of many diseases, the most dangerous of which is stroke. Therefore, it is better to take the problem seriously and treat it immediately after the diagnosis is confirmed.
Treatment with folk remedies
- Alternative treatment should be used only for chronic disease or as an addition to already prescribed therapy.
Lemon juice with honey
Take one lemon. Cut it. Squeeze out the juice thoroughly. Add 2 tablespoons of honey and one hundred milliliters of water. Mix all ingredients thoroughly and drink. The treatment period is twenty days. After ten days there is a break.
Pollen with honey
Used for head massage. Take 2 parts of flower pollen, add honey. Mix the ingredients and leave for 72 hours in a place where sunlight does not penetrate. Then rub the mixture in small portions into the back of your head, the back of your neck and the bridge of your nose. Then wrap your head with a towel. Carry out the procedure every day for a month.
Plantain
Take three spoons of dry plantain, pour half a liter of boiling water over them and leave for thirty minutes. Drink fifty grams of decoction three times a day.
Video on the topic