Fainting is not a separate disease or diagnosis; it is a short-term loss of consciousness due to an acute decrease in blood supply to the brain, accompanied by a drop in cardiovascular activity.
Fainting or syncope, as it is called, occurs suddenly and usually does not last long - a few seconds. Absolutely healthy people are not immune from fainting, that is, one should not rush to interpret it as a sign of a serious illness; it is better to try to understand the classification and causes.
Classification of syncope
True fainting includes attacks of short-term loss of consciousness, which can be divided into the following types:
- Neurocardiogenic (neurotransmitter) form includes several clinical syndromes, therefore it is considered a collective term. The formation of neurotransmitter fainting is based on the reflex effect of the autonomic nervous system on vascular tone and heart rate, provoked by factors unfavorable for a given organism (temperature environment, psycho-emotional stress, fear, sight of blood). Fainting in children (in the absence of any significant pathological changes from the heart and blood vessels) or in adolescents during hormonal changes often have a neurocardiogenic origin. This type of syncope also includes vasovagal and reflex reactions that can occur during coughing, urination, swallowing, physical activity and other circumstances not related to cardiac pathology.
- or fainting occurs due to slow blood flow in the brain with a sharp transition of the body from a horizontal to a vertical position.
- Arrhythmogenic syncope. This option is the most dangerous. It is caused by the formation of morphological changes in the heart and blood vessels.
- Loss of consciousness, which is based on(changes in cerebral vessels).

Meanwhile, some conditions called fainting are not classified as syncope, although they look very similar to it. These include:
- Loss of consciousness associated with metabolic disorders (hypoglycemia - a drop in blood glucose, oxygen starvation, hyperventilation with a decrease in carbon dioxide concentration).
- Epilepsy attack.
Exists a group of disorders that resemble fainting, but occur without loss of consciousness:
- Short-term muscle relaxation (cataplexy), as a result of which a person cannot maintain balance and falls;
- Sudden onset of movement coordination disorder – acute ataxia;
- Syncopal states of psychogenic nature;
- TIA caused by impaired blood circulation in the carotid system, accompanied by loss of ability to move.
The most common case

A significant proportion of all fainting belongs to neurocardiogenic forms. Loss of consciousness provoked by ordinary everyday circumstances (transport, stuffy room, stress) or medical procedures (various copies, venipuncture, sometimes just visiting rooms that resemble operating rooms), as a rule, does not cause changes in the heart and blood vessels. Even arterial pressure, which decreases at the time of fainting, is at normal level. Therefore, all responsibility for the development of an attack is placed on the autonomic nervous system, namely, on its departments - the sympathetic and parasympathetic, which for some reason stop working in harmony.
Fainting of this kind in children and adolescents causes a lot of anxiety on the part of parents, who cannot be reassured only by the fact that such a condition is not a consequence of a serious pathology. Repeated fainting is accompanied by injury, which reduces quality of life and can be dangerous in general.
Why does consciousness disappear?
For a person far from medicine, classification, in general, does not play any role. Most people in an attack with loss of consciousness, pale skin and falling see fainting, but they cannot be blamed for a mistake. The main thing is to rush to help, and the doctors will figure out what kind of loss of consciousness, so we won’t particularly try to convince the readers.

However, based on the classification, but taking into account the fact that not everyone knows its subtleties, we will try to determine the causes of fainting, which can be both trivial and serious:
- Heat- the concept is different for everyone, one person feels tolerable at 40°C, another 25 - 28 - already a disaster, especially in a closed, unventilated room. Perhaps most often, such fainting occurs in crowded transport, where it is difficult to please everyone: some are windy, others feel ill. In addition, there are often other provoking factors (crush, odors).
- Prolonged absence of food or water. Fans of rapid weight loss or people forced to starve for other reasons beyond their control know something about hungry fainting. Syncope can be caused by diarrhea, persistent vomiting, or loss of fluid due to other circumstances ( frequent urination, increased sweating).
- Abrupt transition from a horizontal body position(got up - everything swam before my eyes).
- Sense of anxiety, accompanied by increased breathing.
- Pregnancy (redistribution of blood flow). Fainting during pregnancy is a common occurrence; moreover, sometimes loss of consciousness is one of the first signs interesting situation women. Emotional instability inherent in pregnancy against the background of hormonal changes, heat outside and in the house, fear of gaining extra kilos(hunger) provoke a decrease in blood pressure in a woman, which leads to loss of consciousness.
- Pain, shock, food poisoning.
- Jar of Hearts(why, before telling some terrible news, the person for whom it is intended will be asked to sit down first).
- Rapid blood loss for example, donors lose consciousness during blood donation not because some volume of precious fluid has been lost, but because it left the bloodstream too quickly and the body did not have time to turn on the defense mechanism.
- The sight of wounds and blood. By the way, men faint from blood more often than women, it turns out that the fair half is somehow more accustomed to it.
- Decrease in circulating blood volume(hypovolemia) with significant blood loss or due to taking diuretics and vasodilators.

- Reduced blood pressure, vascular crisis, the cause of which may be the uncoordinated work of the parasympathetic and sympathetic parts of the autonomic nervous system, its failure to perform its tasks. Fainting is not uncommon in adolescents suffering from or in children in puberty with diagnosable symptoms. In general, for hypotensive people, fainting is a common thing, so they themselves begin to avoid traveling on public transport, especially in the summer, visiting steam rooms in the bathhouse and any other places with which they have unpleasant memories.
- A fall(hypoglycemia) - by the way, not necessarily with an overdose of insulin in patients with diabetes. The “advanced” youth of our time know that this drug can be used for other purposes (increase height and weight, for example), which can be very dangerous (!).
- or what is popularly called anemia.
- Repeated fainting in children may be evidence serious illnesses, For example, syncope is often a sign of a disorder heart rate, which is quite difficult to recognize in a child early age because, unlike adults, cardiac output is more dependent on heart rate (HR) than stroke volume.
- The act of swallowing with pathology of the esophagus(a reflex reaction caused by irritation vagus nerve).
- Hypocapnia causing constriction of cerebral vessels, which is a decrease in carbon dioxide (CO 2) due to increased oxygen consumption with frequent breathing, characteristic of a state of fear, panic, and stress.
- Urination and cough(due to an increase in intrathoracic pressure, a decrease in venous return and, accordingly, a limitation of cardiac output and a decrease in blood pressure).
- Side effect of some medications or overdose of antihypertensive drugs.
- Reduced blood supply to certain areas of the brain(), although rare, can cause fainting in elderly patients.
- Serious cardiovascular pathology(myocardial infarction, etc.).
- Some endocrine diseases.
- in the brain obstructing blood flow.
Thus, most often, changes in the circulatory system caused by a drop in blood pressure lead to loss of consciousness. The body simply does not have time to adapt in a short time: the pressure has decreased, the heart has not had time to increase blood output, the blood has not brought enough oxygen to the brain.
Video: causes of fainting - program “Live Healthy!”
The reason is the heart
Meanwhile, you should not relax too much if syncope becomes too frequent and the causes of fainting are not clear. Fainting in children, adolescents and adults is often a consequence of cardiovascular pathology , where not the last role belongs to various kinds ( and ):
- Associated with, high degree of, (often in older people);
- Caused by taking β-blockers, improper functioning of the valve prosthesis;
- Caused by drug intoxication (quinidine), electrolyte imbalance, lack of carbon dioxide in the blood.

Cardiac output can also be reduced by other factors that reduce cerebral blood flow, which are often present in combination: a drop in blood pressure, dilatation of peripheral vessels, decreased return venous blood to the heart, hypovolemia, vasoconstriction of the outflow tract.
Loss of consciousness in heart patients during physical exertion is a fairly serious indicator of ill health, since cause of fainting in this case can be:
- : stenosis of the tricuspid valve (TC) and valve pulmonary artery(LA);
Of course, such listed diseases rarely cause fainting in children; basically, they develop during life, and therefore are a sad advantage of advanced age.
What does fainting look like?
Fainting conditions are often accompanied. Hypoxia caused by the background does not give much time for reflection, although people for whom loss of consciousness is not something supernatural can sense the approach of an attack in advance and call this state prefainting. It is better to describe the symptoms indicating the approach of syncope and the fainting itself together, since the onset is felt by the person himself, and the fainting itself is seen by those around him. As a rule, upon regaining consciousness, a person feels normal, and only slight weakness reminds of loss of consciousness.

So, symptoms:
- “I feel sick” is how the patient defines his condition.
- Nausea sets in and an unpleasant sticky cold sweat breaks out.
- The whole body weakens, the legs give way.
- The skin turns pale.
- My ears are ringing and spots are flashing before my eyes.
- Loss of consciousness: the face is grayish, blood pressure is low, the pulse is weak, usually rapid (tachycardia), although bradycardia is not excluded, the pupils are dilated, but they react to light, albeit with some delay.
In most cases, the person comes to his senses within a few seconds. With a longer attack (5 minutes or more), involuntary urination is also possible. Such fainting can easily be confused by unknowing people with an attack of epilepsy.
Table: how to distinguish true fainting from hysteria or epilepsy

What to do?
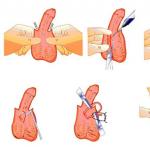
Having become an eyewitness to fainting, every person must know how to behave, although loss of consciousness often occurs without any first aid, if the patient quickly came to his senses, was not injured in a fall, and after syncope his state of health more or less returned to normal. First aid for fainting comes down to performing simple measures:

- Spray your face lightly with cold water
- Place the person in a horizontal position, place a bolster or pillow under their feet so that they are higher than their head.
- Unbutton the shirt collar, loosen the tie, provide access fresh air.
- Ammonia. If someone faints, everyone runs for this remedy, but sometimes they forget that they need to handle it carefully. Inhaling its vapors can lead to a reflex cessation of breathing, that is, you should not bring a cotton swab moistened with alcohol too close to the nose of a person who has lost consciousness.
Rendering emergency care with syncope is more related to its underlying cause(rhythm disturbance) or with consequences (bruises, cuts, traumatic brain injury). If, moreover, a person is in no hurry to return to consciousness, then one should be wary of other causes of fainting (drop in blood sugar, hysteria). By the way, as for hysteria, people prone to it are capable of fainting on purpose, the main thing is that there are spectators.
It is hardly worth arrogantly trying to find out the origin of prolonged fainting without having certain skills of the medical profession. The most reasonable thing would be to call an ambulance, which will provide emergency care and, if necessary, take the victim to the hospital.
Video: help with fainting - Dr. Komarovsky
How to fall into a frill on purpose / recognize an imitation
Some people manage to trigger an attack with the help of breathing (breathe frequently and deeply) or, after squatting for a while, rise sharply. But then it could be a real fainting?! It is quite difficult to simulate artificial fainting, healthy people It still doesn't work out well.
Syncope during hysteria can mislead those same spectators, but not the doctor: a person thinks in advance about how to fall so as not to get hurt, and this is noticeable, his skin remains normal (unless he smeared it with whitewash beforehand?), and if (suddenly?) it comes to the point to convulsions, but they are not caused by involuntary muscle contractions. By bending and taking various pretentious poses, the patient only imitates a convulsive syndrome.
Finding the reason
The conversation with the doctor promises to be long...

At the beginning of the diagnostic process, the patient should tune in to a detailed conversation with the doctor. He will ask a lot of different questions, the detailed answer to which is known to the patient himself or the parents, if it concerns a child:
- At what age did the first fainting appear?
- What circumstances preceded it?
- How often do attacks occur, are they the same in nature?
- What triggering factors usually lead to fainting (pain, heat, exercise, stress, hunger, cough, etc.)?
- What does the patient do when a “feeling of faintness” sets in (lies down, turns his head, drinks water, eats food, tries to go out into the fresh air)?
- What is the period before the attack?
- Features of the nature of the pre-fainting state (ringing in the ears, darkening of the eyes, nausea, pain in the chest, head, stomach, heart beating rapidly or “freezing, stopping, sometimes knocking, sometimes not knocking...”, lack of air)?
- The duration and clinical picture of the syncope itself, that is, what does fainting look like according to eyewitnesses (the position of the patient’s body, skin color, pulse and breathing pattern, blood pressure level, presence of convulsions, involuntary urination, tongue bite, pupil reaction)?
- Condition after fainting, the patient’s well-being (pulse, breathing, blood pressure, want to sleep, headache and dizziness, general weakness)?
- How does the person being examined feel outside of syncope?
- Which transferred or chronic diseases Is he celebrating it (or what did his parents say)?
- What pharmaceuticals did you have to use during your life?
- Does the patient or his relatives indicate that childhood Were there any paraepileptic phenomena (walking or talking in your sleep, screaming at night, waking up in fear, etc.)?
- Family history (similar attacks in relatives, vegetative-vascular dystonia, epilepsy, heart problems, etc.).
Obviously, what at first glance seems like a mere trifle can play a leading role in the formation of syncope, which is why the doctor pays such close attention to various little things. By the way, the patient, when going for an appointment, must also dig deep into his life in order to help the doctor discover the cause of his fainting.
Inspection, consultation, equipment assistance
Examination of the patient, in addition to determining constitutional features, measuring (on both hands), listening to heart sounds, involves identifying pathological neurological reflexes, studying the functioning of the autonomic nervous system, which, of course, cannot be done without consulting a neurologist.
Laboratory diagnostics include traditional blood and urine tests (general), a sugar curve, as well as a number of biochemical tests, depending on the expected diagnosis. At the first stage of the search, the patient must undergo and use R-graphic methods, if necessary.

In case of suspicion the arrhythmogenic nature of syncope, the main emphasis in diagnosis falls on the study of the heart:
- R – cardiac imaging and contrasting of the esophagus;
- bicycle ergometry;
- special methods for diagnosing cardiac pathology (in a hospital setting).
If the doctor suspects that syncope causes organic brain diseases or the cause of fainting appears vaguely, the range of diagnostic measures expands noticeably:
- R-graphy of the skull, sella turcica (location of the pituitary gland), cervical spine spine;
- Consultation with an ophthalmologist (visual fields, fundus);
- (electroencephalogram), including a monitor one, if there is a suspicion of an attack of epileptic origin;
- EchoES (echoencephaloscopy);
- (vascular pathology);
- CT, MRI (space-occupying lesions, ).
Sometimes, even the methods listed do not fully answer questions, so you should not be surprised if the patient is asked to take a urine test for 17-ketosteroids or a blood test for hormones ( thyroid gland, genitals, adrenal glands), since it is sometimes difficult to find the cause of fainting.
How to treat?
The tactics for treating and preventing syncope depend on the cause of fainting. And it's not always medications. For example, with vasovagal and orthostatic reactions The patient is first of all taught to avoid situations that provoke syncope. To do this, it is recommended to train vascular tone, carry out hardening procedures, avoid stuffy rooms, sudden changes in body position, men are advised to switch to urination while sitting. Usually, individual points are discussed with the attending physician, who takes into account the origin of the attacks.

Fainting caused by a drop in blood pressure is treated by increasing blood pressure also depending on the reason for its decrease. Most often, this cause is neurocirculatory dystonia, so drugs that affect the autonomic nervous system are used.
Recurrent fainting, which may be of arrhythmogenic nature, deserves special attention. It should be borne in mind that they increase the likelihood sudden death, therefore, in such cases, arrhythmia and the diseases that cause it are treated in the most serious way.
It is impossible to say unambiguously about fainting states: they are harmless or dangerous. Until the cause is clarified, and attacks continue to bother the patient every now and then, the prognosis can be very different (even extremely unfavorable), because it completely depends on the nature of this condition. How high the risk is will be determined by a thorough history and a comprehensive physical examination, which can be the first step towards forever forgetting about this unpleasant “surprise” that can make a person lose consciousness at the most inopportune moment.
One of the presenters will answer your question.
Currently answering questions: A. Olesya Valerievna, Ph.D., teacher at a medical university
Unconsciousness can be caused by the most for various reasons and, accordingly, can manifest itself in different forms - from simple fainting to a life-threatening deep coma.
An unconscious state similar to deep sleep: a person does not perceive anything and does not react to stimuli. Note that this condition can be characterized by varying degrees of severity - from short-term loss of senses to long-term coma. Whatever the cause of loss of consciousness, the initial cause is always changes in the brain.
Loss of consciousness and regulatory mechanism
Maintaining consciousness is determined by the functioning of a number of important areas of the brain, in particular: the cerebral cortex, the base of the brain, the visual thalamus, and especially a group of cells called the reticular formation.
Even when a person loses consciousness, the base of the brain still supports the functioning of the body's major systems. Therefore, in an unconscious state, as a rule, only auxiliary areas of the brain are affected.
Electroencephalography
Brain activity can be measured using an electrical encephalograph. On an electroencephalogram, brain impulses are indicated as wavy lines; The configuration of the waves changes depending on the type of activity or mode of functioning of the brain. For example, if the patient is unconscious, then the device slowly demonstrates large waves (three per second); if a person comes to his senses or wakes up, then the device already draws 6-8 waves per second, and also records faster and sharper fluctuations, which indicates increased electrical activity.
Electroencephalography helps doctors find out how much the brain is damaged; after all, the absence of an electrical signal is a sign of a complete cessation of brain activity.
What is coma or coma?
Coma is dangerous form unconscious state. In some cases, comatose states last for a very long time. During comas, unlike sleep, brain activity is suppressed, and the person cannot respond to stimuli (coughing, sneezing, etc. are absent), and he also lacks tendon, corneal and other reflexes. In a very deep coma, the patient cannot even respond to painful stimuli.
The causes of coma are, as a rule, brain damage (as a result of bleeding or tumors), as well as sudden shock or blood intoxication (in particular, urea). An extended coma can also be caused by damage to the thalamus.
Diabetes mellitus and hypoglycemia can lead to coma, but in such cases medicine can help effective assistance to the patient.
Previously, any coma that lasted more than 24 hours led to irreversible brain damage, however modern methods treatment and patient care have significantly changed the situation. However, the longer a person is in a coma, the less likely he is to make a final and complete recovery.
In all cases of unconsciousness, treatment will be determined by the reasons that caused it: for some it will be enough to simply rest, while for others surgical intervention will be required. A comatose patient requires long-term treatment.
Remember that if a person loses consciousness, it is necessary to provide first aid and
Review
Fainting is a sudden temporary loss of consciousness, usually accompanied by a fall.
Doctors often refer to fainting as syncope to distinguish it from other conditions involving temporary loss of consciousness, such as a seizure or concussion.
Fainting is very common, with up to 40% of people losing consciousness at least once in their lives. The first fainting episode usually occurs before the age of 40. If the first episode of loss of consciousness occurs after age 40, this may indicate severe chronic illness. The most common neurogenic syncope is most often observed during adolescence in girls.
The immediate cause of syncope is a disruption in the flow of oxygen-rich blood to the brain. Its functions are temporarily impaired, and the person loses consciousness. This usually happens in a stuffy room, on an empty stomach, with fear, severe emotional shock, and in some people, with the sight of blood or a sudden change in body position. A person may faint from coughing, sneezing, or even while emptying the bladder.
First aid for fainting should be to prevent the person from falling and protect him from injury. If someone feels bad, support them and gently lay them down, raising their legs up, or sit them down. Provide fresh air by opening windows and unbuttoning your collar. Try not to create panic in order to avoid large crowds of people, crowding and stuffiness. When fainting, consciousness usually returns within a few seconds, less often - 1-2 minutes, but some types of fainting require immediate attention. medical care.
If the person does not regain consciousness within 2 minutes, call ambulance by calling 03 from a landline, 112 or 911 from a mobile phone.
Symptoms of fainting
Fainting is usually preceded by sudden weakness and dizziness, followed by a brief loss of consciousness, usually lasting a few seconds. This can happen when a person is sitting, standing, or standing up too quickly.
Sometimes loss of consciousness may be preceded by other short-term symptoms:
- yawn;
- sudden sticky sweat;
- nausea;
- frequent deep breathing;
- disorientation in space and time;
- blurred vision or spots before the eyes;
- tinnitus.
After a fall, the head and heart are at the same level, so blood reaches the brain more easily. Consciousness should return in about 20 seconds; less often, fainting lasts for 1-2 minutes. A longer absence of consciousness is an alarming signal. In this case, you need to call an ambulance.
After fainting, you may feel weak and confused for 20 to 30 minutes. The person may also feel tired, drowsy, nauseated, and have abdominal discomfort, and may not remember what happened just before the fall.
Fainting or stroke?
Loss of consciousness can occur with a stroke - a disorder cerebral circulation. A stroke, unlike fainting, always requires emergency medical attention and is life-threatening. A stroke can be suspected if a person does not regain consciousness for more than 2 minutes or if after fainting the victim has the following symptoms:
- the face is skewed to one side, the person cannot smile, his lip has drooped or his eyelid has drooped;
- the person is unable to lift one or both arms and keep them upright due to weakness or numbness;
- speech becomes unintelligible.
Causes of fainting (loss of consciousness)
Loss of consciousness during syncope is associated with a temporary reduction in blood flow to the brain. The causes of this type of circulatory disorder are very diverse.
Disruption of the nervous system as a cause of loss of consciousness
Most often, loss of consciousness is associated with a temporary malfunction of the autonomic nervous system. This type of fainting is called neurogenic or vegetative syncope.
The autonomic nervous system is responsible for unconscious body functions, including heartbeat and blood pressure regulation. Various external stimuli, for example, fear, the sight of blood, heat, pain and others, can temporarily disrupt the functioning of the autonomic nervous system, which leads to a drop in blood pressure and fainting.
The work of the autonomic nervous system is also associated with a slowdown of the heart, which leads to a short-term decrease in blood pressure and impaired blood supply to the brain. This is called vasovagal syncope.
Sometimes the autonomic nervous system becomes overloaded during coughing, sneezing or laughing and loss of consciousness occurs. This kind of fainting is called situational.
In addition, fainting may be associated with prolonged standing in an upright position. Typically, when a person stands or sits, gravity causes some of the blood to flow downward and pool in the arms and legs. To maintain normal blood circulation, the heart begins to work a little harder, the blood vessels narrow slightly, maintaining sufficient blood pressure in the body.
In some people, this mechanism is disrupted, and the blood supply to the heart and brain is temporarily interrupted. In response, the heart begins to beat too fast, and the body produces norepinephrine, a stress hormone. This phenomenon is called postural tachycardia and can cause symptoms such as dizziness, nausea, sweating, rapid heartbeat and fainting.
Carotid sinus syndrome
The carotid sinus is a symmetrical area on the lateral surface of the middle part of the neck. This is an important area, rich in sensitive cells - receptors, which is necessary to maintain normal blood pressure, heart function and blood gas composition. In some people, syncope (fainting) can occur when there is an accidental mechanical impact on the carotid sinus - this is called carotid sinus syndrome.
Orthostatic hypotension is a cause of fainting in the elderly
The second most common cause of fainting can be a drop in blood pressure when a person stands up suddenly - orthostatic hypotension. This phenomenon is more common in older people, especially after 65 years of age.
A sudden change in body position from horizontal to vertical leads to the outflow of blood to the lower parts of the body under the influence of gravity, causing blood pressure in the central vessels to drop. Typically the nervous system regulates this by increasing the heart rate, constricting blood vessels and thus stabilizing blood pressure.
At orthostatic hypotension the regulatory mechanism is disrupted. Therefore, rapid pressure restoration does not occur, and blood circulation in the brain is disrupted for some period. This is enough to cause fainting.
Possible causes of orthostatic hypotension:
- dehydration is a condition in which the body's fluid content decreases and blood pressure decreases, making it harder for the heart to stabilize, increasing the risk of fainting;
- diabetes mellitus - accompanied by frequent urination, which can lead to dehydration; in addition, high blood sugar levels damage the nerves responsible for regulating blood pressure;
- medications - any medications for hypertension, as well as any antidepressants, can cause orthostatic hypotension;
- Neurological diseases - diseases affecting the nervous system (for example, Parkinson's disease) can cause orthostatic hypotension.
Heart disease - the cause of cardiac syncope
Heart disease can also cause disruption of the blood supply to the brain and lead to temporary loss of consciousness. This type of fainting is called cardiac syncope. Its risk increases with age. Other risk factors:
- pain in the heart cell (angina);
- suffered a heart attack;
- pathology of the structure of the heart muscle (cardiomyopathy);
- abnormalities on the electrocardiogram (ECG);
- repeated sudden fainting without warning symptoms.
If you suspect that fainting is caused by heart disease, you should consult a physician as soon as possible.
Reflex anoxic spasms
Reflex anoxic convulsions are a type of fainting that develops after a short-term cardiac arrest due to overload of the vagus nerve. It is one of 12 cranial nerves that runs down from the head into the neck, chest and abdomen. Reflex anoxic seizures are more common in young children, especially when the child is upset.
Diagnosis of the causes of fainting
Most often, fainting is not dangerous and does not require treatment. But in some cases, after fainting, you should consult a doctor to find out whether the loss of consciousness was caused by any disease. Contact a neurologist if:
- fainting occurred for the first time;
- you regularly lose consciousness;
- injury due to loss of consciousness;
- you have diabetes or heart disease (such as angina);
- fainting occurred during pregnancy;
- before fainting, you felt chest pain, irregular, rapid or strong heartbeat;
- during blackout, urination or defecation occurred involuntarily;
- you were unconscious for several minutes.
During the diagnosis, the doctor will ask about the circumstances of the fainting and recent illnesses, and may also measure your blood pressure and listen to your heartbeat with a stethoscope. In addition, additional research will be required to diagnose the causes of loss of consciousness.
Electrocardiogram (ECG) is prescribed when it is suspected that fainting was caused by heart disease. An electrocardiogram (ECG) records the heart rhythms and electrical activity of the heart. Electrodes (small sticky discs) are attached to the arms, legs and chest and are connected to the ECG machine using wires. Each heartbeat creates an electrical signal. The ECG notes these signals on paper, recording any abnormalities. The procedure is painless and takes about five minutes.
Carotid sinus massage performed by a doctor to rule out carotid sinus syndrome as a cause of fainting. If the massage causes dizziness, heart rhythm disturbances or other symptoms, the test is considered positive.
Blood tests allow you to exclude diseases such as diabetes and anemia (anemia).
Blood pressure measurement in the supine and standing positions to detect orthostatic hypotension. In orthostatic hypotension, blood pressure drops sharply when a person stands up. If the test results reveal a medical condition, such as heart disease or orthostatic hypotension, your doctor may prescribe treatment.
First aid for fainting
There are certain measures that should be taken when someone is fainting. It is necessary to position the person in such a way as to increase blood flow to the head. To do this, just put something under your feet, bend them at the knees or lift them up. If you have nowhere to lie down, you need to sit down and put your head between your knees. Doing this will usually help prevent fainting.
If a person does not regain consciousness within 1-2 minutes, you need to do the following:
- lay it on its side, supported by one leg and one arm;
- tilt your head back and lift your chin to open
Airways; - Continuously monitor your breathing and pulse.
Then you should call an ambulance by calling 03 from a landline phone, 112 or 911 from a mobile phone and stay with the person until doctors arrive.
Treatment after fainting
Most fainting spells do not require treatment, but it is important for your doctor to rule out possible diseases which could cause loss of consciousness. If the latter are detected during examination, you will need treatment. For example, if you are diagnosed with diabetes, diet, exercise, and medications can help lower your blood sugar levels. Treatment cardiovascular diseases associated with fluctuations in blood pressure, rhythm disturbances or atherosclerosis also minimizes the likelihood of recurrent syncope.
If fainting is of a neurogenic nature or is situational, then you need to avoid those causes that usually lead to loss of consciousness: stuffy and hot rooms, excitement, fear. Try to spend less time standing on your feet. If you faint at the sight of blood or medical procedures, tell your doctor or nurse so they can do the procedure while you lie down. When it is difficult to determine what situations cause you to faint, your doctor may recommend keeping a symptom diary to record the circumstances surrounding your fainting spells.
To prevent fainting caused by carotid sinus syndrome, you should avoid putting pressure on the neck area - for example, not wearing shirts with a high, tight collar. Sometimes a pacemaker is inserted under the skin to treat carotid sinus syndrome - a small electronic device, which helps maintain a regular heart rhythm.
To avoid orthostatic hypotension, try not to change your body position suddenly. Before getting out of bed, sit up, stretch, and take a few calm, deep breaths. In summer, you should increase your water consumption. The doctor may also recommend eating smaller meals in small portions and increasing salt intake. Some medications may lower blood pressure, but you should stop taking prescribed medications only with your doctor's approval.
To stop the drop in blood pressure and prevent fainting, there are special movements:
- crossing legs;
- muscle tension in the lower body;
- clenching your hands into fists;
- arm muscle tension.
The technique of correctly performing these movements needs to be learned. In the future, these movements can be performed after noticing symptoms of impending fainting, for example, dizziness.
Sometimes medications are used to treat after fainting. However, drug therapy must be prescribed by a doctor.
In addition, syncope can create dangerous situation at work. For example, when handling heavy equipment or dangerous mechanisms, when working at height, etc. Issues of work ability are resolved on a case-by-case basis with the attending physician after completion of the diagnosis.
Which doctor should I contact after fainting?
With the help of the NaPopravku service, you can diagnose possible causes of fainting and offer treatment, if necessary.
If your episodes of loss of consciousness are accompanied by other symptoms not described in this article, use the “Who Treats It” section to choose the right specialist.
Localization and translation prepared by site. NHS Choices provided the original content for free. It is available from www.nhs.uk. NHS Choices has not reviewed, and takes no responsibility for, the localization or translation of its original content
Copyright notice: “Department of Health original content 2019”
All site materials have been checked by doctors. However, even the most reliable article does not allow us to take into account all the features of the disease in specific person. Therefore, the information posted on our website cannot replace a visit to the doctor, but only complements it. The articles have been prepared for informational purposes and are advisory in nature.
Definition of coma, collapse, fainting. Basic clinical characteristics of assessing the state of consciousness. Sudden and short-term loss of consciousness due to narrowing or occlusion of the arteries supplying the brain. Pathogenesis.
ABOUTfainting. Collapse. Coma.
The ability to provide emergency care is an absolute requirement for any medical worker, regardless of his specialty. The most common cases of depression of consciousness, in which urgent medical benefit, relate FAINTING And COMA. Collapse may be a harbinger of fainting and also deserves the closest attention.
Opdefinition of coma, collapse, fainting.
1. Faintingcharacterized by generalized muscle weakness, decreased postural tone, inability to stand upright, and loss of consciousness (Raymond D., Adams et al., 1993).
2. Coma(from the Greek cat - deep sleep) - complete shutdown of consciousness with a total loss of perception of the environment and oneself and with more or less pronounced neurological and autonomic disorders. Coma severity depends on the duration of neurological and autonomic disorders. Coma of any etiology (ketoacidotic, uremic, hepatic, etc.) have common symptoms and are manifested by loss of consciousness, decrease or disappearance of sensitivity, reflexes, skeletal muscle tone and disorder of the body’s autonomic functions (VFO). Along with this, symptoms characteristic of the underlying disease are observed (focal neurological symptoms, jaundice, azotemia, etc.).
3. Collapse(from Latin collabor, collapsus - weakened, fallen) - acutely developing vascular insufficiency, characterized by a drop in vascular tone and a relative decrease in circulating blood volume (CBV). Loss of consciousness at collapse can occur only with a critical decrease in blood supply to the brain, but this is not a mandatory sign. The fundamental difference collapse from shock is the absence of pathophysiological signs characteristic of the latter: sympathoadrenal reaction, microcirculation disorders and tissue perfusion, acid-base condition, generalized dysfunction of cells. This condition can occur against the background of intoxication, infection, hypo- or hyperglycemia, pneumonia, adrenal insufficiency, and physical and mental fatigue. Clinically collapse manifested by a sharp deterioration in condition, the appearance of dizziness or loss of consciousness (in this case we will talk about fainting), the skin becomes pale, cold sweat appears, mild acrocyanosis, shallow, rapid breathing is noted, sinus tachycardia. The degree of blood pressure reduction reflects the severity of the condition. Emergency care is the same as treatment for fainting.
4. Acute vascular insufficiency— violation of venous return due to an increase in the capacity of the vascular bed. Presence of acute vascular insufficiency the victim does not have to be accompanied by fainting; the latter occurs only when the blood supply to the brain drops below critical. Fainting And coma refer to quantitative syndromes of disturbance (depression) of consciousness. Our country has adopted a working classification of depression of consciousness, proposed by A.I. Konovalov et al., (1982), according to which there are 7 degrees of consciousness assessment: clear; moderate stun; the stun is deep; sopor; moderate coma; deep coma; extreme coma. Qualitative syndromes of disturbance (stupidity) of consciousness (delirium, oneiric syndrome, amentia and twilight disorders of consciousness) are presented in the topic “ Emergency conditions in psychiatry."
TO classification of oppression of consciousness (A. I. Konovalova). Assessment of the state of consciousness. Degrees of depression of consciousness. Glasgow scale.
ABOUTmain clinical characteristics of assessing the state of consciousness (A. I. Konovalov et al., 1982)
Clear consciousness- its complete safety, adequate reaction to the environment, complete orientation, wakefulness.
Moderate stun- moderate drowsiness, partial disorientation, delay in answering questions(often requires repetition), slow execution of commands.
Deep Stun- deep drowsiness, disorientation, almost complete sleepiness, limited and difficult speech contact, monosyllabic answers to repeated questions, following only simple commands.
WITHsupports(unconsciousness, deep sleep) - almost complete absence of consciousness, preservation of purposeful, coordinated defensive movements, opening of the eyes to painful and sound stimuli, occasional monosyllabic answers to multiple repetitions of a question, immobility or automated stereotypical movements, loss of control over pelvic functions.
Moderate coma(I) - inability to wake up, chaotic uncoordinated defensive movements to painful stimuli, lack of opening the eyes to stimuli and control of pelvic functions, mild respiratory and cardiovascular problems are possible.
Deep coma(II) - inability to wake up, lack of protective movements, impaired muscle tone, inhibition of tendon reflexes, severe respiratory impairment, cardiovascular decompensation. Transcendental (terminal) coma(III) - atonal state, atony, areflexia, vital functions are supported by respiratory devices and cardiovascular drugs.
Otsenthe depth of the disturbance of consciousness in emergency situations in an adult, without resorting to special methods studies can be carried out using the Glasgow scale, where each answer corresponds to a certain score (see Table 14), and in newborns - using the Apgar scale.
Table 14. Glasgow scale.
I. Opening the eyes:
Missing 1
For pain 2
For speech 3
Spontaneous 4
II. Response to painful stimulus:
Missing 1
Flexion reaction 2
Extensor reaction 3
Withdrawal 4
Localization of irritation 5
Executing command 6
III. Verbal answer:
Missing 1
Inarticulate sounds 2
Incomprehensible words 3
Confused Speech 4
Complete orientation 5
Otsenka states of consciousness is made by totaling points from each subgroup. 15 points correspond to a state of clear consciousness, 13-14 - stunned, 9-12 - stupor, 4-8. - coma, 3 points - brain death.
Note. Correlation between indicatorsGlasgow scaleand mortality in coma is highly reliable. The number of points from 3 to 8 corresponds to a mortality rate of 60%, from 9 to 12 - 2%, from 13 to 15 about 0 (D. R. Shtulman, N. N. Yakhno, 1995).
ABOUT general condition of the patient. Assessment of the patient's general condition. Severity of general SOS the patient's languor.
In addition to assessing the impairment of consciousness and determining the etiological factor, it is important to evaluate general state sick.
The clinic differentiates 5 degrees of severity of the patient’s general condition: satisfactory, moderate, severe, extremely severe and terminal.
Satisfactory condition- consciousness is clear. Vital important functions not violated.
WITHmoderate condition- consciousness is clear or there is moderate stupor. Vital functions are slightly impaired.
TIyellow state- consciousness is impaired to the point of deep stupor or stupor. There are severe disorders of the respiratory or cardiovascular systems.
WITHthe condition is extremely serious- moderate or deep coma, fubo severe symptoms damage to the respiratory and/or cardiovascular systems.
Tterminal state- extreme coma with gross signs of damage to the trunk and disturbances of vital functions.
TO omatous states. Causes (etiology) of coma. Classification of comatose states. The vast majority comatose states, depending on the etiological factor, can be reduced into the following three groups (D. R. Shtulman, N. N. Yakhno, 1995):
1. Diseases not accompanied by focal neurological signs.
Normal cellular composition cerebrospinal fluid. Normal CT scan(CT) and magnetic resonance imaging (MRI). This group includes:
Intoxication (alcohol, barbiturates, opiates, anticonvulsants, benzolyazepines, tricyclic antidepressants, phenothiazines, ethylene glycol, etc.);
Metabolic disorders (hypoxia, diabetic acidosis, uremia, hepatic coma, hypoglycemia, adrenal insufficiency);
Severe general infections (pneumonia, typhus, malaria, sepsis);
Vascular collapse (shock) of any etiology and cardiac decompensation in old age;
Epilepsy;
Hypertensive encephalopathy and eclampsia;
Hyperthermia and hypothermia.
2. Diseases that cause irritation of the meninges with an admixture of blood or cytosis in the cerebrospinal fluid, usually without focal cerebral and brainstem signs. CT and MRI scans may be normal or abnormal. Diseases in this group include;
Subarachnoid bleeding due to aneurysm rupture;
Acute bacterial meningitis;
Some forms of viral encephalitis.
3. Diseases accompanied by focal brainstem or lateralized brain signs with or without changes in the cerebrospinal fluid. CT and MRI detect pathological changes. This group includes:
Brain hemorrhages;
Cerebral infarction due to thrombosis or embolism;
Brain abscesses and subdural empyemas;
Epidural and subdural hematomas;
Brain contusion;
Brain tumors.
According to simplified classification comatose state divided into omu destructive (anatomical) And to whom metabolic (dismetabolic)(D.R. Shtulman, N.N. Yakhno, 1995).
Loss of consciousness. Types of loss of consciousness. Systematization of types of loss of consciousness. General recommendations for emergency care. Scheme of interviewing an eyewitness.
WITHAndStematization of types of loss of consciousness
For a systematic approach to diagnostics and emergency care, all accidents with loss of consciousness it is most convenient to look at the following types(Colin Ogilvie, 1981):
1. Sudden and short-term loss of consciousness.
2. Sudden and prolonged loss of consciousness.
3. Prolonged loss of consciousness with a gradual onset.
4. Loss of consciousness of unknown onset and duration.
The concept " sudden and short-lived» assumes duration loss of consciousness from a few seconds to several minutes, and the term “ Pgradual and long lasting” implies hours or days. General recommendations when providing emergency care
Issues of providing emergency care to unconscious victims have their own specifics: limited time when life-threatening condition, the lack of anamnesis and medical history forces the doctor to be extremely collected and accurately follow the general recommendations below.
1. If possible, an eyewitness should be interviewed according to the scheme given in table. 15. Correct interpretation of the data obtained can be a good help in establishing a clinical diagnosis.
Table 15. Eyewitness Interview Design (Colin Ogilvie, 1987).
Time of day
Provoking factor: heat, excitement, pain, change in body position, physical activity, etc.
Initial body position: standing, sitting, lying down
Skin color: pallor, hyperemia, cyanosis
Pulse: frequency, rhythm, filling
Movements: jerky or involuntary; local or general
Fall injury, involuntary urination
Seizure duration
Recovery symptoms: headache, confusion, speech disorders, paresis, etc.
2. Any variety loss of consciousness can be both a consequence and a cause of traumatic brain injury (TBI), therefore, at the initial stages of diagnosis and treatment, it must be excluded or confirmed. We should not forget that when sudden loss consciousness, it is possible to hit your head on hard objects, which in itself can cause a TBI.
3. Quite often cause of coma Alcohol intoxication can occur, but even in the presence of its very characteristic signs, alcohol cannot be considered the root cause of coma until a “drunken” injury has been ruled out and laboratory confirmation of a high concentration of alcohol in the blood has been obtained.
4. When examination of the patient, unconscious, it is necessary to determine the degree of impairment of consciousness, its etiology and assess the general condition of the patient.
IN n sudden and short-term loss of consciousness. Causes of sudden and short-term loss of consciousness. Simple fainting (postural syncope). Causes (etiology) of simple fainting. Most common cause of sudden and short-term loss of consciousness May be:
1. Simple fainting.
2. Transient narrowing or occlusion of the arteries supplying the brain.
Diagnosis simple syncope(Postural syncope) can be exposed to the victim only in that
in the event that loss of consciousness occurred in a vertical position, and its recovery occurred several tens of seconds (up to 5 minutes) after the body was in a horizontal position.
Etiology. Provoking factors Psevere fainting can be:
1. Standing suddenly or standing for a long time, especially in the heat ( orthostatic type of fainting).
2. Factors that activate vasovagal reflexes - pain, the sight of blood, fear, psycho-emotional overload, urination, defecation, coughing (vasodepressor (vasovagal) type of fainting).
3. Compression of the carotid sinus area ( fainting due to carotid sinus hypersensitivity syndrome).
4. Autonomic neuropathy.
5. Uncontrolled use of antihypertensive, sedatives, antihistamines and other drugs.
Pathogenesis of simple fainting. Clinic for simple fainting. Differential diagnosis simple fainting (postural syncope).
Pathogenesis of simple fainting is associated with a short-term decrease in the venous tone of the vessels of the lower extremities and the abdominal cavity, i.e., the volume of circulating blood (CBV) becomes relatively small for the vascular bed and blood is deposited in the periphery. This causes a decrease in venous return and a drop in cardiac output and, as a consequence, a disruption of the blood supply to the brain occurs. The basis of the vasodepressor type of fainting (during defecation, urination) is a sharp increase in intrathoracic pressure during straining, which causes a decrease in venous inflow and a drop in cardiac output.
Clinic.
ABOUTfainting may occur suddenly or with warning signs. Precursors of the development of simple fainting is the appearance in the victim of a feeling of weakness, dizziness, nausea, darkening of the eyes. Objectively, at this time one can note pallor of the skin, beads of sweat on the face, bradycardia and hypotension. With loss of consciousness, decreased muscle tone and weakened tendon reflexes are noted. Characteristic a sign of simple fainting is the appearance of sinus bradycardia. The rapid restoration of consciousness in a horizontal position confirms the correctness diagnosis of syncope. At deep faint urinary incontinence is possible, however this syndrome more common in epilepsy.
DiffErential diagnosis of simple fainting (postural syncope).
1. Internal bleeding. If it is present, especially with a slow flow with the absence pain syndrome and visible bleeding, the patient may experience fainting with a fairly rapid restoration of consciousness in a horizontal position of the body, but the persistence of tachycardia, instead of typical bradycardia, shortness of breath and pallor of the skin, will be indirect signs of existing anemia. The study of red blood parameters has a decisive role in this situation.
2. Painless forms of acute myocardial infarction or pulmonary embolism may be accompanied by a short-term loss of consciousness. When the victim’s body is in a horizontal position after the restoration of consciousness, signs of respiratory and circulatory failure remain with signs of overload of the pulmonary circulation, cardiac arrhythmias, etc. In typical cases, short-term loss of consciousness for the above reasons occurs when the body is in a vertical position (standing or sitting) . If loss of consciousness occurs in the victim lying down, one should think about a disturbance in the rhythm of cardiac activity (primarily a Morgagni-Edams-Stokes attack, or cerebrovascular accident.
IN n sudden and short-term loss of consciousness due to narrowing or occlusion of the arteries, supplying brain. Pathogenesis.
This variant of pathology is predominantly found in elderly people against the background of atherosclerotic damage to the arteries supplying blood to the brain.
At the core pathogenesis May be:
2. Embolism of individual areas of the brain with small emboli formed at the site of narrowing of the arteries.
3. Mechanical strengthening of the existing occlusion.
4. “Subclavian steal syndrome.”
5. Aortic stenosis.
1. Spasm of the cerebral arteries, as the cause of cerebrovascular accident, can be assumed if fainting occurs against the background of a migraine attack or a hypertensive crisis.
2. Site of vertebral stenosis or carotid arteries , supplying blood to the brain, can be a source of microemboli formation. When a patient recovers from a fainting state of this etiology, a characteristic sign is the appearance of specific neurological symptoms:
Loss of vision in one eye ( transient amaurosis) or hemiparesis that developed immediately after fainting indicates an acute circulatory disorder in the carotid artery system;
The appearance of dizziness, hemianopia, diplopia and imbalance indicates an acute circulatory disorder in the vertebrobasilar artery system.
3. Fainting, which occurs against the background of mechanical strengthening of the existing stenosis of the vertebral arteries, is called “Sistine Chapel syndrome”. This condition was first described in elderly tourists in Rome while viewing Michelangelo's frescoes on the dome of the Sistine Chapel. Loss of consciousness is associated with prolonged hyperextension of the neck and compression or kinking of the vertebral arteries.
4. " Subclavian steal syndrome“occurs against the background of initial stenosis of the subclavian arteries proximal to the origin of the thyrocervical trunk. When working intensively with your hands, blood flow in vertebral arteries becomes retrograde and acute cerebral ischemia occurs.
5. Brief loss of consciousness possible against the background of aortic stenosis, if performed quickly physical activity; a harbinger of fainting may be the appearance of ischemic pain in the heart area.
In children, less often in adults, one of the reasons for short-term loss of consciousness may be “ epilepsy minortic seizure» ( absence seizure). During such an attack, it is sometimes possible to notice instantaneous movements of the muscles of the face, eyes or limbs. These seizures are so short in duration that the victim does not have time to fall and can only drop what was in his hands.
If within a few minutes the patient, despite emergency assistance, consciousness is not restored, one should think about the development of a coma.
Comatose states may also present with sudden and prolonged loss of consciousness and gradual and prolonged loss of consciousness.
IN n sudden and prolonged loss of consciousness. Scheme of examination of a patient in a comatose state.
INnsudden and prolonged loss of consciousnessmay be a manifestation acute disorder cerebrovascular accident (CVA), hypoglycemia, epilepsy and hysteria. If, after emergency care is provided, the patient does not regain consciousness within a few minutes, additional information The contents of the victim’s pockets and wallet can serve as evidence: prescriptions for specific medications or the medications themselves can suggest the correct path for diagnosis and treatment. Having a home phone number will allow you to quickly contact relatives and obtain information on issues of interest; a diabetic or epileptic card will indicate the probable cause of the coma. To prevent possible undesirable legal complications, checking the contents of pockets should be carried out in the presence of witnesses, followed by drawing up an inventory of everything found. This is followed bystart clinical examination in accordance with table. 16.
Table 16. Scheme of examination of a patient in a comatose state (according to Colin Ogilvie,
1987).
1. Skin: moist, dry, hyperemic, cyanotic, icteric
2. Head and face: presence of injuries
3. Eyes: conjunctiva (hemorrhage, jaundice); reaction of pupils to light; fundus (disc edema, hypertensive or diabetic retinopathy)
4. Nose and ears: discharge of pus, blood; liquorrhea; acrocyanosis
5. Tongue: dry; bite marks or scars
6. Breath: smell of urine, acetone, alcohol
7. Neck: stiff neck, pulsation of the carotid arteries
8. Rib cage: frequency, depth, rhythm of breathing
9. Heart: rhythm disturbance (bradycardia); sources of cerebral embolism (mitral stenosis)
10. Belly: Enlarged liver, spleen or kidneys
11. Hands: blood pressure, hemiplegia, injection marks
12. Hands: frequency, rhythm and filling of the pulse, tremor
13. Legs: hemiplegia, plantar reflexes
14. Urine: incontinence or retention, protein, sugar, acetone
First of all, when examining a patient, you should exclude TBI. At the slightest suspicion, an X-ray examination of the skull should be done in 2 projections.
ABOUThagony neurological symptoms allows us to suggest the presence of an acute cerebrovascular accident.
WITHVhedgehog tongue bites or old scars it will most likely indicate epilepsy.
Diagnosis of hysterical coma should be set only after complete exclusion of organic pathology. It should be emphasized that this complication of hysteria, despite popular opinion, is quite rare.
Npresence of multiple traces of subcutaneous injections in typical places will talk about diabetes mellitus, and multiple traces of intravenous injections, often in the most unexpected places, suggests drug addiction.
At the slightest suspected hypoglycemic condition, without waiting for laboratory confirmation, you should urgently administer 40-60 ml of 40% glucose solution intravenously. If the patient subsequently develops even a ketoacidotic coma, his condition will not worsen, and in case of hypoglycemia, this simple method of treatment will save the life of the victim.
Prolonged loss of consciousness with a gradual onset. Causes (etiology) and diagnosis h clear signs of comatose states with a gradual onset and prolonged loss of consciousness.
Comatose states that develop gradually in a hospital setting, as a rule, do not present difficulties in diagnosis. So, if a patient has acute liver failure that cannot be treated, then he may subsequently develop hepatic coma. The main causes of gradual and prolonged loss of consciousness are given in table. 17. Issues of diagnosis and treatment of comatose states given in this table are discussed in the corresponding chapters of the textbook.
Table 17. The most common causes and diagnostic signs of comatose states with a gradual onset and prolonged loss of consciousness (according to Colin Ogilvie, 1987).
| 2. Vascular disorders | Hemiplegia (hemiparesis), hypertension, stiff neck muscles (with subarachnoid hemorrhage) |
| 3. Tumor | Focal symptoms of the central nervous system, swelling of the optic nerve disc on the affected side |
| 4. Infection | Drainage of pus from the nose or ears, stiff neck, fever |
| 5. Epilepsy | Seizures on examination or history, scars or fresh bite marks on the tongue |
| II. Metabolic pathology | |
| 1. Uremia | Uremic breath, dehydration, muscle twitching, retinopathy, proteinuria |
| 2. Diabetes | Acetone breath, dehydration, retinopathy (microaneurysms), sugar and ketone bodies in urine |
| 3. Hypoglycemia | Sweating, trembling, Babinski's sign may be present |
| 4. Hepatic coma | Jaundice, splemomegaly, hematemesis, “popping” tremor |
| III. Intoxication | |
| 1. Alcohol | Smell of alcohol on the breath, facial flushing (look carefully for a head injury) |
| 2. Psychotropic drugs | Breathing disorders, moderate hypersalivation |
| 3. Carbon monoxide | Breathing disorders, characteristic hyperemia |
When a person finds himself in an unconscious state, it is very frightening to those around him. In most cases, they do not know what happened to the victim - fainting or loss of consciousness. What is the difference between these conditions? Or are these terms synonymous, as many believe? In order not to get lost in guesswork, you will have to deepen your medical knowledge.
Fainting is a loss of response to external stimuli and a lack of awareness of the surrounding reality, which occurs unexpectedly and does not last long. IN medical dictionary fainting is referred to as "syncope". Syncope develops if blood flow to the head becomes poor, which provokes oxygen starvation of the brain.
Loss of consciousness is a broader and deeper concept. This is the name for a fairly long-term depression of the autonomic nervous system and the absence of reflexes, which can be the result of many serious pathologies.
Signs of unconsciousness
When a person is close to fainting, he:
- the ability to reason deteriorates;
- noise in the ears;
- dizzy;
- frequent yawning and a feeling of stuffiness appear;
- limbs become cold;
- the skin becomes too pale or acquires a bluish tint (if it is hot in the room or outside, skin may, on the contrary, blush);
- nails turn blue;
- sweat secretion increases;
- nausea and an unpleasant taste in the mouth occur;
- muscles relax sharply;
- blood pressure drops;
- heartbeat quickens or slows down;
- pupils dilate.
Then those around them see that the person is “settling down.”

Blackout in case of fainting lasts from a few seconds to 2 minutes. The eyeballs roll back, the pressure remains low, the pulse is weak, beads of sweat are visible on the skin, and convulsions are possible. The victim does not move, does not react to sounds, light or pain. All the muscles of the body are absolutely weak-willed, so involuntary emptying of the bladder or intestines often occurs. After 20-30 seconds consciousness returns, and no negative consequences in the long term this condition does not entail.
If you are not dealing with fainting, but with loss of consciousness, then the difference in their clinical picture can be understood by the fact that the person:
- loses mobility and the ability to think very quickly;
- his condition does not improve within 5 minutes.
The return of reactions - as well as the subsequent recovery of the patient - occurs slowly, and memory loss is possible.
Why does consciousness “go away”?
A person may faint due to:
- excessive fatigue;
- severe pain;
- dehydration of the body;
- stressful situation;
- emotional shock;
- nervous tension;
- freezing or, conversely, overheating;
- lack of oxygen;
- coughing attack;
- physical activity;
- gestation;
- menstrual bleeding;
- immediate reduction in blood pressure;
- exceeding the dose of a certain medication;
- alcohol intoxication;

- fasting or poor nutrition;
- sudden change in body position;
- arrhythmias and heart diseases.
As you can see, most of The problems listed above are temporary, transient in nature, and it is relatively easy to cope with them. Unlike fainting, loss of consciousness is a symptom of some serious illness. It, as already mentioned, lasts longer than simple fainting, and sometimes it is followed by coma. The list of causes of loss of consciousness includes the following ailments and conditions:
- ischemic attack;
- cerebral hemorrhage and other types of stroke;
- epilepsy attack;
- state of shock;
- hypoglycemia;
- severe circulatory disorders;
- significant damage to the skull and brain;
- damage to the lungs and nervous system;
- intoxication due to poisoning.