rental block
Small doses of radiation do not seem to have a noticeable effect on the immune system. When animals are irradiated with sublethal and lethal doses, a sharp decline resistance of the body to infection, which is due to a number of factors, among which the most important role is played by: a sharp increase in the permeability of biological barriers (skin, respiratory tract, gastrointestinal tract etc.), inhibition of the bactericidal properties of the skin, blood serum and tissues, a decrease in the concentration of lysozyme in saliva and blood, a sharp decrease in the number of leukocytes in the bloodstream, inhibition of the phagocytic system, adverse changes in the biological properties of microbes permanently living in the body - an increase in their biochemical activity, increased pathogenic properties, increased resistance, etc.
Irradiation of animals in sublethal and lethal doses leads to the fact that from large microbial reservoirs (intestines, Airways, skin) a huge amount of bacteria enters the blood and tissues.! At the same time, a period of sterility is conditionally distinguished (its duration is one day), during which microbes are practically not detected in tissues; the period of contamination of regional lymph nodes(usually coincides with the latent period); bacteremic period (its duration is 4-7 days), which is characterized by the appearance of microbes in the blood and tissues, and, finally, the period of decompensation defense mechanisms, during which there is a sharp increase in the number of microbes in organs, tissues and blood (this period occurs a few days before the death of animals).
Under the influence of large doses of radiation, causing partial or complete death of all irradiated animals, the body is unarmed both to endogenous (saprophytic) microflora and exogenous infections. It is believed that during the height of acute radiation sickness, both natural and artificial immunity are greatly weakened. However, there are data indicating a more favorable outcome of the course of acute radiation sickness in animals subjected to immunization prior to exposure to ionizing radiation. At the same time, it has been experimentally established that vaccination of irradiated animals aggravates the course of acute radiation sickness, and for this reason it is contraindicated until the disease resolves. On the contrary, several weeks after irradiation in sublethal doses, the production of antibodies is gradually restored, and therefore, already 1-2 months after radiation exposure, vaccination is quite acceptable.
We have the biggest information base in Runet, so you can always find similar requests
This topic belongs to:
Radioactive safety
Sampling of crop products. Effect of ionizing radiation on the immune system. The degree of change in the hematopoietic organs and blood vessels is directly dependent on the dose of radiation. Organization of radiological control in veterinary medicine
How to get a tax deduction
Who can return the money? What do we subtract from? What amount can you get? How many times can you get a deduction? When will the money be returned? Calculation example. Registration. What documents to collect?
Pharmacy training practice report
During the internship, I got acquainted with the pharmacy of Zdorovye LLC. She studied the formation of the company Zdorovye LLC. Completed safety training
Media typology
Typology is a classification of objects or phenomena according to the commonality of any signs. When studying journalism, it is important to professionally competently be able to give a typological description of each particular publication or broadcast program.
Child development at an early age. indicative figures
Indicators of child development at an early age. Indicators of child development in infancy. Approximate indicators of the neuropsychic development of children.
liferative activity (division rate) of these cells, the rate of division and maturation in the departments of morphologically recognizable precursors. It has been shown that after irradiation, the proliferation rate of stem cells increases, as a result of which the doubling time of their number is reduced from 5-6 days. up to 1 day.
The depth and duration of aplasia of the hematopoietic tissue is the greater, the higher the dose of radiation. However, there are exceptions to this rule. After irradiation at high doses (5.5 Gy in humans), the rate of recovery of the myeloid germ of hematopoiesis is significantly higher, and the number of cells in the bone marrow and blood is restored to the control level earlier than after exposure to doses of 2-3 Gy, despite the fact that that the degree of devastation in the first case was much greater. The reason for this phenomenon is not entirely clear.
In the case of uneven irradiation or complete shielding of individual parts of the body, damage to the organs of the hematopoietic system is modified due to the migration of cells from less irradiated parts. This mechanism ensures a faster repopulation of irradiated organs than with general uniform irradiation.
The stromal elements of the bone marrow are quite radioresistant. In the first weeks after irradiation at doses at which the development pathological process due mainly to damage to the hematopoietic system, resting stromal fibroblasts are little damaged. Their functional activity as producers of prostaglandin E and colony stimulating factors (CSF) is preserved and sometimes increases. Therefore, with total irradiation at doses at which the number of SCMs compatible with survival is maintained, damage to stromal elements is little pronounced, and their significance in the development of bone marrow aplasia is small. When irradiated at higher doses (of the order of 100 Gy), used, in particular, for radiotherapy tumors, some of the mature fibroblasts die, while their secretion of prostaglandin E and CSF increases.
As for the parent cells for fibroblasts (CFU-F), they are quite radiosensitive in humans: D0 = 1.3 Gy. In addition, in the period when bone marrow hematopoiesis is restored, CFU-F proliferate very sluggishly. These features may be important for the development of long-term changes in the hematopoietic system, such as aplastic anemia, etc.
In a morphological study after irradiation at high doses (about 10 Gy), after a few hours in the red bone marrow
observe damage to cell nuclei: pycnosis, karyorrhexis (apoptosis), karyolysis. Sometimes the cytoplasm is also destroyed (cytolysis). Bone marrow sinuses expand, erythrocytes go into the bone marrow parenchyma. A few hours later, the process of phagocytosis of damaged myelokaryocytes begins: nuclear fragments, and sometimes whole cells, are found in bone marrow macrophages. In rats, already 1-2 days after superlethal irradiation, the bone marrow is cleared of cellular decay products, leaving only stromal elements. The development of necrotic changes in the cells of the bone marrow is accompanied by vascular reactions, and the histological picture of the bone marrow can be characterized as inflammation with its characteristic phases of alteration, exudation, and, subsequently, the development of repair processes. In the devastated edematous stroma of the bone marrow, hemorrhages are observed. Bone marrow 3 days after irradiation at a superlethal dose looks like a "lake of blood". Shortly before death, bacteria are found in the bone marrow.
At lower radiation doses, the changes are less pronounced. In cases ending in recovery, separate foci of hematopoiesis first appear, and over time they merge. In humans, 2 days after irradiation at doses of 2-6 Gy histological examination sections of the bone marrow can detect a decrease in the number of cells of erythroid and granulocytic germs by 1.5-2 times compared to the norm, areas with exposed stroma, swelling of the underlying substance, small hemorrhages.
Later, a progressive increase in the content of stromal elements is observed in the bone marrow: fibroblasts, reticular cells, macrophages. After irradiation in doses of 2-4 Gy at the beginning of the second week, during the period corresponding to the previously described abortive rise, an increase in the mitotic activity of bone marrow cells is noted, and the number of undifferentiated cells increases. By the end of the third week, an increase in the number of cells of granulocytic and erythroid germs is detected. At higher radiation doses, the manifestations of abortive rise are much less pronounced.
From the end of the third week after irradiation at doses of more than 2-3 Gy, aplasia progresses in the bone marrow, manifested by fatty atrophy. The area of adipose tissue on sections of the bone marrow can reach 80%. At the same time, signs of regeneration are also detected: microfoci of undifferentiated cells and cells of early generations of erythroid and myeloid germs, as well as increased proliferation of stromal cells. Subsequently, foci of hematopoietic tissue grow
3.5. The effect of ionizing radiation on critical body systems
quickly enough, ensuring the restoration of hematopoietic function.
Even a year after irradiation at doses of 2-4 Gy, the structure of the bone marrow is not completely restored. Large foci of fatty degeneration persist, the number of stromal cells is increased compared to the norm, hematopoietic tissue in the bone marrow parenchyma is represented not diffusely, but by separate large foci. After exposure to radiation in doses of 5 Gy and above, widespread foci of hypoplasia are observed in the bone marrow during these periods.
Morphological changes in bone marrow cells associated with their direct damage (pycnosis of the nucleus, karyorrhexis, destruction or swelling of the nucleus) can usually be registered in the first hours after irradiation. Destroyed cells are quickly removed. Later, cells with anomalies associated with mitotic disorders begin to be detected: giant cells, cells with a hypersegmented nucleus, with abnormal mitotic figures (bridges in anal or telophase), chromosome fragments in interphase cells. The maximum yield of these cells falls on 12-24 hours after irradiation. By the third day, most of these cells also disappear.
3.5.3. Post-radiation changes in the morphological composition of peripheral blood
The decrease in the number of functional cells begins when the last cells that have entered the maturing section by the time of irradiation enter the peripheral blood, that is, after a period corresponding to the time the cells pass through this section in the norm. The content of neutrophilic granulocytes in the blood, the passage of which through the maturation department is 5-6 days, begins to decrease from this time.
The rate of decrease in the number of cells in the blood is the higher, the shorter the duration of their circulation after being released from the bone marrow. The rather long period between irradiation and the development of maximum neutropenia (this occurs by the end of the third week) is explained by the fact that from the middle of the second week after irradiation, an abortive rise in the content of granulocytes develops in the peripheral blood.
The reasons for the release of a significant number of mature neutrophilic cells into the blood at this time are associated with the effect of extramedullary factors on the bone marrow, in particular, with an increase in the blood at early stages.

their terms after exposure to the content of catecholamines and other biologically active substances.
In the dynamics of changes in the number of blood neutrophils after irradiation, several phases can be distinguished:
− initial or primary neutrophilia;
- lag phase (at this time, the natural release of blood neutrophils into the tissues is compensated by the entry of these cells from the maturation pool);
− primary devastation;
− abortive rise;
− secondary devastation;
− restoration.
Lymphocytes die in early dates after irradiation; accordingly, their level in the peripheral blood rapidly decreases.
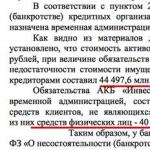
Rice. 11. Dynamics of changes in the number of granulocytes in the blood after total irradiation (according to S. Killman, 1974):
1 - primary neutrophilia; 2 - lag phase; 3 - primary devastation; 4 - abortive rise; 5 - secondary devastation; 6 - recovery
With a sharp decrease after irradiation total number leukocytes in the blood, one can speak of an equally profound decrease in the absolute number of monocytes.
The content of tissue macrophages during the first week after irradiation does not change significantly. The functional activity of these cells also does not change or even appears to be increased. At the same time, the workload of these cells with tissue decay products reduces the effectiveness of their participation in the antimicrobial defense system. In the period of expressed clinical manifestations radiation injury, the number of cells of the system of mononuclear phagocytes is reduced.
3.5. The effect of ionizing radiation on critical body systems
The dynamics of platelet count after irradiation is similar to changes in the number of neutrophils. An abortive rise is expressed only after irradiation in relatively low (up to about 3.5 Gy) doses. In the phase of secondary devastation, deep thrombocytopenia is observed: by the end of the 3-4th week after irradiation at average lethal doses, the platelet count reaches 5-8% of the normal level.
The content of erythrocytes after irradiation decreases slowly and moderately, since mature erythrocytes are sufficiently radioresistant, and the life span of these cells is about 100 days. Even with the complete cessation of their formation, the number of red blood cells in the blood due to natural death decreases by about 1% per day (if there are no bleeding complicating the situation).
The depth of cytopenia directly depends on the radiation dose. At doses of the order of 5-6 Gy, neutrophils and platelets may not be detected at all in peripheral blood smears. The time interval required to restore the number of these cells to the initial level after irradiation at high doses may turn out, as already mentioned when characterizing changes in the hematopoietic organs, to be shorter than when exposed to lower doses.
In addition to quantitative changes in blood cells after irradiation, morphological changes are also detected: homogenization of lymphocyte nuclei, the appearance of lymphocytes with micronuclei, giant hypersegmented neutrophils, and giant platelets.
3.5.4. Effect of irradiation on immune system
The main function of the immune system is to protect the body from exposure to foreign antigens and to control the maintenance of the genetic constancy of the internal environment of the body. The immune system performs this function with the help of natural and adaptive (acquired) mechanisms. At the core natural immunity lies the action of non-specific mechanisms associated with the functioning of cellular (neutrophils, macrophages, NK cells (natural killers), etc.) and humoral (complement, lysozyme, interferons, etc.) factors. Factors of natural immunity are relatively radioresistant and are affected only at very high doses of radiation. Specific immunity based on properties
T- and B-lymphocytes respond selectively to foreign substances, on the contrary, they are highly sensitive to the action of radiation.
Lymphocytes are among the most radiosensitive cells in the body, and their death is noted already after exposure to radiation in tenths of a gray. In this case, not only young dividing cells die, but also (an exception to the rule of Bergonier and Tribondo) mature lymphocytes, which in normal conditions(without antigenic stimulation) do not divide. Among the radiosensitive cells susceptible to interphase death at doses close to or even lower than those that cause reproductive death of hematopoietic stem cells, T-lymphocytes (T-helpers and T-suppressors), B-lymphocytes and thymocytes are isolated. thymus. The radiosensitivity of B-lymphocytes is higher than that of T-lymphocytes, and the radiation resistance of T-suppressors is somewhat greater than that of T-helpers. Thymocytes also differ in their radiosensitivity: the maximum radiosusceptibility is observed in cambial cells, and the greatest radioresistance is in epithelial cells. In addition, there is a relatively small population of radioresistant cells among T-lymphocytes, which retain their functional activity after irradiation at very high doses (6–10 Gy, and according to some data, up to 20 Gy). These cells are both cortisone-resistant. Their content is about 3-8% of all T-lymphocytes, and, possibly, they are memory T-cells.
The high radiosensitivity of mature populations of blood lymphocytes and their interphase death on the first day after exposure to ionizing radiation is also associated with the rapid development of lymphopenia after exposure. Interphase death of lymphocytes is not associated with the moment of cell mitosis, it begins after 6 hours and ends 3 days after exposure to radiation. The destruction of lymphocytes after irradiation occurs both in the lymphoid organs (thymus, lymph nodes, spleen, lymphoid formations in the intestine), and in the peripheral blood and lymph. As a result, it is possible to detect a decrease in the number of lymphocytes in the blood already tens of minutes after irradiation, and by the 3rd day the number of lymphocytes decreases to a minimum. The depth of the decrease in the level of lymphocytes, as well as other peripheral blood cells, directly depends on the radiation dose. It should be emphasized that the post-radiation drop in the number of lymphocytes, along with granulocytopenia, is the main cause of the development of the syndrome. infectious complications during the height of acute radiation sickness.
3.5. The effect of ionizing radiation on critical body systems
Table 37 - Radiosensitivity of some cells of the human immune system
(according to A.A. Yarilin, 1989, 1997; T. Szepesi, T.M. Fliedner, 1989)
Type of cells |
D0 , Gr |
pluripotent hematopoietic stem cells |
|
Granulocyte precursor cells |
|
Blood neutrophils |
|
Monocyte precursor cells |
|
blood monocytes |
|
NK cells (natural killer cells) |
|
Lymphocyte precursor cells: early stages |
|
late stages |
|
Blood lymphocytes: T-lymphocytes |
|
B-lymphocytes |
|
Thymocyte progenitor cells - cambial thymus cells |
|
Thymus epithelial cells |
|
thymus dendritic cells |
|
The impact of radiation on lymphoid tissue leads not only to the death of lymphocytes, but also causes significant changes in their functional activity. This, in turn, can lead to a distortion of the immune response both in the short term and (which is especially important) in the long-term period after radiation exposure.
Thus, in the next few minutes or hours after irradiation, both B-lymphocytes and especially T-lymphocytes are characterized by the loss of cell receptors present on their surface for various antigens, which is associated with the interference of ionizing radiation in the rearrangement of TCR genes (antigen-recognizing receptor of T-lymphocytes). A post-radiation change in the expression of adhesion molecules leads to disruption of the distribution of lymphocytes in the blood and lymphoid organs and actually distorts the spatial organization of the immune system.
Already in the early stages after irradiation, the ability of B-lymphocytes to produce specific immunoglobulins in response to antigenic stimulation is significantly reduced. This inhibition directly correlates with the dynamics of depopulation of lymphoid organs, and is most pronounced in the case of antigen administration after 1-2 days. after irradiation. With the introduction of the antigen shortly before irradiation, the production of antibodies may even increase. In the case of pre-immunization before
The “secondary response” to the re-introduction of the antigen after irradiation is not significantly disturbed by the action of radiation.
Another immediate result of radiation exposure is a decrease in the proliferative activity of T-lymphocytes, their migratory properties, and the ability to inactivate non-syngeneic CFUs. The death of T-lymphocytes as a result of irradiation is accompanied by a decrease in their cytotoxic functions in the body, which is manifested by the suppression of some delayed-type hypersensitivity reactions, graft-versus-host reactions, etc. The severity of the inhibition of these reactions depends to a large extent on the level of functional activity of T-lymphocytes , which is suppressed already after irradiation in doses of 0.15-0.20 Gy.
Exposure to ionizing radiation leads to an imbalance of T-helpers of the Th1 and Th2 classes, which determine the ratio of the cellular mediated and humoral components of the immune response, as well as a number of manifestations of immunopathology. Recall that Th2 products - interleukin-2, γ-interferon, β-tumor necrotic factor - provide the development cellular immunity, and Th2 products - interleukin-4, -5, -10 - serve as mediators of the humoral response. These cells are in the ratio of antagonism, implemented with the participation of γ-interferon and interleukin-10.
Thl differentiation is maintained by macrophages through the production of interleukin-12, and Th2 development is regulated by interleukin-4. In turn, the product Thl γ-interferon stimulates the activity of macrophages.
3.5. The effect of ionizing radiation on critical body systems
It has been established that the higher the dependence of the immune response on the thymus, the stronger the effect of radiation. The effect of ionizing radiation on the thymus-dependent link of the immune system consists of a direct effect on T-cells and an indirect effect through the thymus stroma. The activity of the thymus stroma in the early periods after irradiation may increase, and in later periods, as a rule, it is suppressed, which is accompanied by an accelerated transfer of thymus powers to the peripheral part of the immune system and the development of manifestations of immunological aging.
In the early post-radiation period, the likelihood of developing autoimmune reactions also increases, the severity of which increases with increasing radiation dose. However, autoimmune processes are also manifested in late dates after radiation exposure, as well as under the action of low doses of radiation. A number of researchers believe that for low doses and intensities of ionizing radiation, the development of autoimmune processes is even more characteristic than for the consequences of exposure to high doses.
Under the action of high doses of ionizing radiation that kill most lymphocytes, the formation of the antigen-recognizing mechanism is disrupted. The cells that determine the selection of thymocytes differ greatly in their radiosensitivity: epithelial cells are resistant to radiation at doses up to 8–10 Gy, while dendritic cells die already at doses of 2–4 Gy. In this regard, the process of positive selection is relatively radioresistant, and low-dose irradiation can even increase its effectiveness. On the contrary, the process of negative selection is disturbed even under the action of relatively low doses of radiation, as a result of which a part of autoreactive clones can be preserved and subsequently become a source of autoaggression. In late periods after irradiation, not only dendritic, but also thymic epithelial cells can suffer. This is due to the death of their relatively radiosensitive precursors - dividing cambial cells (D0 for them is 2.5-3.7 Gy). As a result, the number of differentiated T-lymphocytes decreases, the total number of thymocytes decreases (a similar process is observed with aging), and, as a result, the likelihood of developing autoimmune and tumor processes increases.
Another factor leading to the progression of autoimmune processes in an irradiated organism is the early postradiation death of a special population of suppressor cells that inhibit the formation of natural autoantibodies to B1 cells.
endogenous substances. The elimination of these cells by irradiation, and they die already at doses of 4-6 Gy, leads to an increase in the production of natural autoantibodies and, as a result, the development of organ-specific autoimmune processes.
An important aspect of the effect of ionizing radiation on immunity is also their effect on the system of cytokines, products of activated cells of the immune system that play a key role in the regulation of hematopoiesis and intercellular interaction during the development of inflammation and the immune response. The effect of radiation on this system strongly depends on the nature of cytokine-producing cells. Thus, the formation of lymphokines in vivo is suppressed due to the massive death of the lymphocytes producing them, although the process of cytokine production itself can be stimulated by radiation (as is the case with interleukin-2). At the same time, exposure to ionizing radiation leads to an increase in the production of interleukin-1, -6 and tumor necrosis factor by macrophages, stromal and epithelial cells of the thymus. Stimulation of the production of these cytokines by irradiation is of particular interest, because interleukin-1 and tumor necrosis factor themselves have a radioprotective effect, realized with the participation of interleukin-6, and in combination with interleukin-1, radioprotective activity is also manifested in granulocytic and granulocyte-macrophage factors . These facts probably indicate that some of the effects of radiation are aimed at weakening or eliminating the consequences caused by it.
Thus, ionizing radiation significantly affects the immune system, causing a wide range of its reactions - from changes in the regulation of the immune response to the death of immunocompetent cells. Thus, a change in the expression of adhesion molecules, leading to disturbances in the distribution of lymphocytes, distorts the spatial organization of the immune system. Its temporal organization is disturbed due to the interference of radiation in the process of rearrangement of TCR genes, damage to the thymus epithelium and the associated “transfer of the immunological clock” towards aging.
3.5.5. The effect of ionizing radiation on gastrointestinal tract
In the gastrointestinal tract, the most radiosensitive is the small intestine, D0 for epithelial stem cells small intestine is about 1 Gy, while in the large intestine this figure is up to
Sources of ionizing radiation (radionuclides) can be outside the body and (or) inside it. If animals are exposed to radiation from the outside, then they talk about external exposure, and the effect of ionizing radiation on organs and tissues from incorporated radionuclides is called internal irradiation. In real conditions, it is most often possible various options both external and internal exposure. Such options are called combined radiation injuries.
The dose of external exposure is formed mainly due to the impact of g-radiation; b- and c-radiation do not make a significant contribution to the total external exposure of animals, since they are mainly absorbed by the air or the epidermis of the skin. radiation injury skin p-particles is possible mainly when keeping livestock in open areas at the time of the fallout of radioactive products of a nuclear explosion or other radioactive fallout.
The nature of external exposure of animals over time can be different. Various options are possible single exposure when animals are exposed to radiation for a short period of time. In radiobiology, it is customary to consider a single exposure to radiation exposure for no more than 4 days. In all cases where animals are exposed to external irradiation intermittently (they may vary in duration), there is fractionated (intermittent) irradiation. With continuous long-term exposure to ionizing radiation on the body of animals, they speak of prolonged irradiation.
Allocate common (total) exposure in which the entire body is exposed to radiation. This type of exposure occurs, for example, when animals live in areas contaminated with radioactive substances. In addition, under the conditions of special radiobiological studies, local irradiation, when one or another part of the body is exposed to radiation! With the same dose of radiation, the most severe effects are observed with total exposure. For example, when irradiating the whole body of animals at a dose of 1500 R, almost 100% of their death is noted, while irradiation of a limited area of the body (head, limbs, thyroid gland etc.) does not cause any serious consequences. In the following, the consequences of only general external exposure of animals are considered.
Effect of ionizing radiation on immunity
Small doses of radiation do not seem to have a noticeable effect on the immune system. When animals are irradiated with sublethal and lethal doses, a sharp decrease in the body's resistance to infection occurs, which is due to a number of factors, among which the most important role is played by: a sharp increase in the permeability of biological barriers (skin, respiratory tract, gastrointestinal tract, etc.), inhibition of the bactericidal properties of the skin , blood serum and tissues, a decrease in the concentration of lysozyme in saliva and blood, a sharp decrease in the number of leukocytes in the bloodstream, inhibition of the phagocytic system, adverse changes in the biological properties of microbes permanently residing in the body - an increase in their biochemical activity, an increase in pathogenic properties, an increase in resistance and etc.
Irradiation of animals in sublethal and lethal doses leads to the fact that from large microbial reservoirs (intestines, respiratory tract, skin) a huge amount of bacteria enters the blood and tissues.! At the same time, a period of sterility is conditionally distinguished (its duration is one day), during which microbes are practically not detected in tissues; the period of contamination of regional lymph nodes (usually coincides with the latent period); the bacteremic period (its duration is 4--7 days), which is characterized by the appearance of microbes in the blood and tissues, and, finally, the period of decompensation of protective mechanisms, during which there is a sharp increase in the number of microbes in organs, tissues and blood (this period occurs a few days before death).
Under the influence of large doses of radiation, causing partial or complete death of all irradiated animals, the body is unarmed both to endogenous (saprophytic) microflora and exogenous infections. It is believed that during the height of acute radiation sickness, both natural and artificial immunity are greatly weakened. However, there are data indicating a more favorable outcome of the course of acute radiation sickness in animals subjected to immunization prior to exposure to ionizing radiation. At the same time, it has been experimentally established that vaccination of irradiated animals aggravates the course of acute radiation sickness, and for this reason it is contraindicated until the disease resolves. On the contrary, a few weeks after irradiation in sublethal doses, the production of antibodies is gradually restored, and therefore, already 1-2 months after exposure to radiation, vaccination is quite acceptable.
The functioning of the human body to a certain extent is provided by relationships with environmental factors. Of particular importance is its effect on immune activity. These factors can be divided into 3 main groups.
Abiotic - temperature, humidity, daylight hours, barometric pressure, magnetic field disturbance, chemical composition air, soil, water.
Biotic - microflora, flora and fauna.
Anthroponotic - physical ( electromagnetic waves, ionizing radiation, noise, vibration, ultrasound, ultraviolet radiation); chemical (emissions from industrial enterprises and transport, contact with chemicals in production, in agriculture); biological (waste of factories for the production of biological products, food industry); socio-ecological (demographic shifts, urbanization, population migration, changes in diet, living conditions, psychophysical stress, medical measures).
As already mentioned, the immune system is highly sensitive to environmental changes. Therefore, studies of immune reactivity should be carried out at the stage when inducing factors have not yet led to the development of diseases, but have already caused immune damage. It is clear that the resistance of the immune system to negative influences on the body depends on the genotype, health status and much more. Nevertheless, general patterns of response exist under these conditions as well.
The sensitivity of individual parts of the immune system to any factors is different, but in any case, it is a critical target for a large number of eubiotics and other influences. This circumstance causes the formation of prenosological changes in immune reactivity in the body, which, on the one hand, are markers of unfavorable living conditions, and on the other hand, provide the basis for the subsequent development of pathology, chronicity or aggravation of existing diseases.
11.1. IMMUNE REACTIVITY AND THE MICROBIAL ENVIRONMENT
The concept of "microbial environment" includes not only normal automicroflora, but also those microorganisms that a person encounters in everyday life, at work, and in a medical institution.
Certain changes in the composition of the microflora of the body occur under the influence of various factors. This is observed as a result of prolonged use of large doses of antibacterial drugs and in a number of other cases. The human microflora is composed of several compartments. First - own, constant, capable of self-sustaining, includes a limited number of species. Second - this is a true microflora, limitedly capable of self-sustaining, consists of essentially more types. It is inconsistent in composition. The third - passing, random microflora. Its representatives in the body die, and if they multiply, they are very limited, and are quickly eliminated.
Simplification of the microflora creates favorable conditions for the colonization of the macroorganism by new species or varieties, and these processes occur with the formation of secondary immune deficiency in patients.
AT modern conditions the number of so-called nosocomial, hospital infections - infectious processes caused by pathogens circulating in medical institutions is increasing. This pathology is 2-30%, with mortality from 3.5 to 60% of all infectious diseases. AT surgical clinics the frequency of nosocomial infections is 46.7 cases per 1000, in therapeutic - 36.3, in gynecology - 28.1, in maternity wards- 15.3, in pediatrics - 13.9.
Hospital infections occur for a number of reasons.
First of all, because patients develop secondary immune disorders, most often immune deficiency as a result of the underlying disease.
Secondly, many medicines(antibiotics, sulfonamides, etc.) cause simplification of automicroflora.
Thirdly, in large hospitals, the risk of infection of patients with hospital strains of microorganisms increases. Indeed, on an area of more than 15-16 km 2 there are 3 million 300 thousand beds, on which 64 million patients and 6 million medical workers are accommodated during the year with a density of 200 thousand people / km 2.
The cause of nosocomial infections can be more than 2000 types of pathogenic, opportunistic microorganisms, sometimes multi-resistant to 4-5 antibacterial drugs simultaneously, circulating in hospitals for decades. These include staphylococci, pseudomonas, respiratory entero- and rotaviruses, hepatitis A viruses, anaerobic bacteria, molds and yeasts, legionella.
Fourth, invasive aggression characteristic of modern medicine, including more than 3000 types of manipulation interventions - catheterization, bronchoscopy, plasmapheresis, probing, etc., complex medical devices (anesthesia, cardiopulmonary bypass, the internal contour of which is difficult to disinfect, optical equipment).
To this we must add a twofold increase in the number of the elderly population with weakened immune reactivity due to age, frequent use of drugs, X-ray exposure and other reasons that violated the natural biocenosis.
11.2. IMMUNE REACTIVITY AND CHEMICALS
Chemical substances, the number of which reaches 4 billion (63 thousand are used in everyday life), can enter the body and cause various disorders. These include general toxic and local irritant effects, desquamation of the epithelium, bronchospasm, increased penetration of microorganisms through mechanical barriers. With chronic exposure, activation of CD8-lymphocytes is observed, which causes the development of immune tolerance, suppression of antibody production, and inhibition of nonspecific anti-infective resistance factors.
The formation of conjugated antigens and the induction of reactions that deplete the immune system are possible. All these actions, except for the formation of immune deficiency, are also dangerous due to the mutagenic effect.
Immunotropic chemical compounds can be divided into the following groups.
1. Products of complete or partial combustion of fossil fuels - fly ash, toxic radicals, nitrogen peroxides, sulphur dioxide, polycyclic aromatic hydrocarbons, benzpyrenes, cholanthrenes.
2. Products chemical industry: benzene, phenols, xylene, ammonia, formaldehyde, products of plastics, rubber, paint industry, oil products.
3. Household and agricultural chemicals, pesticides, insecticides, herbicides, fertilizers, detergents, cosmetics, drugs, flavors, detergents etc.
4. Metals: lead, mercury, cobalt, molybdenum, etc.
5. Inorganic dust, quartz dioxide, asbestos, carbon, talc, polymetallic aerosols, welding fumes, etc.
Different chemicals trigger different mechanisms of damage to the immune system. For example, chlorinated cyclic dilexins, brominated biphenyls, methylmercury are the cause of impaired maturation of CD3 cells, thymus atrophy, lymph node hypoplasia; alkylating compounds, benzene, ozone, heavy metals - immunosuppression due to DNA damage, and aromatic amines, hydrazine - the formation of cytotoxic antibodies and cell clones against autolymphocytes. The use of halogen aromatic, ozone is accompanied by a decrease in the production of interleukins and interferons; chlorinated cyclic dilexins - functions of CD19 cells and the formation of antibodies; heavy metals, acridine dyes, hexachlorobenzene, aromatic amines - complement defects with a risk of developing SLE. Toxic nitrogen radicals, sulfur oxides, sulfur dioxide, quartz, coal, asbestos cause insufficiency of local immunity, phagocytosis, gastrointestinal tract, lungs, eyes; methylmercury, brominated biphings - suppression of the suppressor function of T-cells with hyperreactivity of CD3- and CD19-lymphocytes; aromatic amines, thiol poisons, mercury, heavy metals, methane - changes in the genotype of lymphocytes, solubilization of membrane HLA antigens, epitopes, CD and other receptors.
11.3. IMMUNE REACTIVITY AND OTHER FACTORS
Electromagnetic waves and microwave fields under chronic exposure cause phase fluctuations in the phagocytic activity of neutrophils, disruption of AT synthesis, which leads to immunopathological and immunosuppressive conditions.
Noise with an intensity of 60-90 dB for 2 months or more contributes to the inhibition of bactericidal and complementary activity.
blood serum, decrease in titers of normal and specific antibodies.
Various metals have a significant effect on the immune system. Beryllium, vanadium and iron induce, respectively, sensitization and modulation, stimulation of lymphoproliferation and modulation, inhibition of phagocytosis and antibody formation; gold, cadmium, potassium and cobalt - inhibition of chemotaxis and release of enzymes from phagocytes; suppression of the humoral immune response; CD3 lymphopenia, decreased DTH and NK cell activity; induction of HNT, HRT. Lithium, copper, nickel, mercury can cause suppression of leukocyte activity; decreased function of CD3 and CD19 cells; thymus involution and allergies; induction of autoimmune reactions and thymus atrophy, respectively. Finally, there are reports that selenium and zinc can cause modulation and, accordingly, thymus hypoplasia and the development of immunodeficiencies.
11.4. IMMUNE REACTIVITY AND REGIONAL
PECULIARITIES
Exist certain connection meteorological factors with indicators of non-specific anti-infective resistance. The increase in the complementary activity of blood serum turned out to be closely associated with an increase in atmospheric pressure, and the production of lysozyme throughout the year - with changes in air temperature and its relative humidity. The level of β-lysines in the blood turned out to be associated with all weather factors, but air temperature had the highest degree of correlation with these indicators.
It is known that each individual is adapted to the usual conditions of life and when changing the place of residence long time adjusting to the new environment. So, immigrants from areas with a hot or temperate climate to the north or northerners to the south experience suppression of immune reactivity during the year, which causes them to have an increased incidence of upper respiratory tract, acute intestinal disorders with a sluggish course and an increase in protracted and chronic forms.
On the other hand, in areas with a cold climate, there is a decrease in the severity of allergic diseases, which is associated with fewer allergens in the environment. At the same time, in persons with a predisposition to allergies, cold air, windy weather cause attacks of asthmatic bronchitis, bronchitis.
al asthma, the occurrence of dermatoses, urticaria. In part, pathological reactions are due to the release into the blood of cold agglutinins, complete and incomplete autoantibodies against skin tissues and internal organs. The change in the immune reactivity of persons who arrived to live in the Arctic and Antarctic regions is determined not only by the effect of low temperature, but also by the lack ultraviolet irradiation, malnutrition, etc.
On examination immune status about 120,000 healthy individuals from 56 cities and 19 territorial regions of the CIS have been diagnosed with several types of immune status. So, immune status with suppression of T-cell immunity found in residents of Norilsk, regions of the Far North, Krasnoyarsk Territory, the city of Kurchatov, Semipalatinsk Region, Novokuznetsk, Tbilisi, suppressive type of immune status - in the city of Serzhal, Semipalatinsk region and Vitebsk, immune status with suppression of humoral immunity - residents of some cities and settlements Central Asian region, as well as - Moscow, St. Petersburg, Chelyabinsk. A uniformly activated type of immune status with some stimulation of the cellular and humoral link was established in the cities of Kirishi and Odessa. An activated profile due to humoral mechanisms with normal or slightly reduced cellular reactions was registered in residents of Rostov-on-Don, Tashkent region, Nizhny Novgorod, Karaganda, Yerevan. mixed type immune status with suppression of cellular and activation of humoral immunity - in Kyiv, Armavir, Karakalpakstan.
11.5. IMMUNE REACTIVITY AND NUTRITION
Moderate manifestations of malnutrition do not cause profound damage to immune reactivity. However, in chronic protein-calorie deficiency, there is a decrease in the activity of phagocytosis, the properdino-complementary system, the formation of interferon, lysozyme, γ-globulins of various classes, a decrease in the content of CD3- and CD19-lymphocytes, their subpopulations, and an increase in the number of immature null cells.
Deficiency of retinol, riboflavin, folic acid, pyridoxine, ascorbic acid, iron, reduces the resistance of tissue barriers, and, in combination with a lack of protein, inhibits the activity of cellular and humoral immunity. In individuals with hypo-
vitamins infectious diseases occur more often, flow harder, prone to chronicity and complications.
Exclusion from the diet of animal proteins leads to inhibition of humoral defense mechanisms. On the other hand, the lack of nucleic acids, even with sufficient caloric intake, leads to the suppression of cellular immunity. It should be emphasized that fasting, including therapeutic, to a certain extent reproduces the above effects.
11.6. IMMUNE REACTIVITY DURING EXPOSURE TO IONIZING RADIATION
The widespread use of nuclear technology entails an expansion of the circle of people exposed to the adverse effects of radiation factors, to which should be added the contingent living in areas contaminated with radionuclides after the Chernobyl accident.
Irradiation of the body causes an increase in the permeability of the skin, subcutaneous fat, pulmonary, blood-brain and hemato-ophthalmic barriers, intestinal vessels in relation to various microorganisms, decay products of autologous tissues, etc. These processes contribute to the development of complications. Violation of permeability begins in the first hours after radiation injury at a dose of 100 roentgens or more, reaches a maximum after 1-2 days. All this contributes to the formation of autoinfections.
A common characteristic feature of the irradiated organism is the prolongation of the period of purification from pathogens, the tendency to generalized infections, and resistance to opportunistic microorganisms (Escherichia coli, Proteus, sarcins, etc.) is especially strongly reduced. Reduced resistance to bacterial toxins Cl. perfringens, Cl. tetani, Cl. botulinum, diphtheria, staphylococcus, shigella. This is based on a decrease in the ability of blood serum to neutralize toxins, as well as damage to the function of the pituitary gland, adrenal glands, and thyroid gland.
Representatives of normal automicroflora living in natural cavities (intestines, respiratory tract), as well as pathogens located in various foci of infection, if any, migrate into the blood, spread to organs. At the same time, the composition of normal microflora changes dramatically,
Species immunity is highly stable to the influence of ionizing radiation.
In a relationship specific immunity irradiation with lethal and sublethal doses before immunization causes a sharp suppression of the formation of antibodies during the first two days, which lasts up to 7 days or more. Inhibition of antibody production is combined with a significant prolongation of the inductive phase of antibody genesis from 2–3 days in the norm to 11–18 days. As a result, the maximum production of antibodies is registered only 40-50 days after irradiation. However, complete inhibition of the synthesis of specific immune globulins does not occur.
If irradiation is carried out after immunization, then the synthesis of antibodies either does not change or slows down slightly. Installed two phases of antibody production under the influence of ionizing radiation. First - radiosensitive, lasting 1-3 days, second - radioresistant, making up the rest of the time period.
Revaccination is quite effective with primary immunization carried out before exposure.
Irradiation of an immunized organism, produced at the height of antibody production, can short-term (several times) reduce the number of circulating antibodies, but after a day (less often two), it is restored to its original values.
Chronic exposure in the same dose as acute exposure before vaccination damages the immune system to a much lesser extent. In some cases, to obtain the same effect, its total dose may exceed a single "acute" dose by more than 4 times.
Ionizing radiation also causes suppression of transplantation immunity. The closer the irradiation is applied to the time of transplantation, the more damage to transplant immunity occurs. With the lengthening of this interval, the inhibitory effect decreases. The normalization of the transplantation reaction of the organism occurs, as a rule, 30 days after exposure.
To a lesser extent, the formation of a secondary transplantation response suffers. As a result, secondary grafts in irradiated contingents are rejected much faster than primary ones.
Ionizing radiation, suppressing the immune system of the recipient
that significantly lengthens the period of immune inertness or tolerance. For example, when bone marrow is transplanted to irradiated persons, the transplanted cells proliferate intensively during the period of immune tolerance caused by irradiation and replace the destroyed hematopoietic tissue of the recipient. There is a chimera organism, because. the hematopoietic tissue in such an organism is the tissue of the donor. All this leads to a prolongation of the engraftment of the donor tissue and the possibility of transplanting other tissues of the donor. On the other hand, radiation can break the formed tolerance. Most often, incomplete non-response suffers, while complete non-response is more radioresistant.
Passive immunity is more resistant to radiation. The timing of the withdrawal of passively administered immune globulins from the irradiated organism, as a rule, does not change. However, their therapeutic activity drops sharply. This makes it necessary to administer 1.5-8 times higher doses of serum or γ-globulins to the corresponding contingents in order to achieve the proper preventive or therapeutic effect.
Irradiation also changes the antigenic composition of tissues. This causes the disappearance of some normal antigens, i.e. simplification of the antigenic structure and the emergence of new antigens. Species antigenic specificity does not suffer from irradiation, organ and organoid specificity changes. The appearance of autoantigens is nonspecific in relation to the radiation factor. Tissue destruction and the appearance of autoantigens are observed within a few hours after irradiation. In some cases, their circulation persists for 4-5 years.
Most of the lymphocytes are highly sensitive to radiation, and this manifests itself already when exposed to external radiation at a dose of 0.5 to 10.0 Gy (in principle, internal radiation has the same effect). Cortical thymocytes, splenic T-cells and B-lymphocytes are the most sensitive to exposure. More resistant are CD4 cells and T-killers. These data substantiate the high risk of autoimmune complications after external and incorporated irradiation.
One of the manifestations of the functional inferiority of irradiated lymphocytes is the violation of their cooperative capabilities. For example, in the first days (1-15 days) after the Chernobyl accident, there was a decrease in the number of cells with the CD2DR+ phenotype. At the same time, there was a decrease in thymic serum titer
factor and indicator RTML with Con-A. All this is evidence of inhibition of the functional activity of the T-system of immunity. Changes in the humoral link were less pronounced.
Small doses of radiation, as a rule, do not cause severe morphological changes in the immune system. Their effect is realized mainly at the level of functional disorders, the recovery of which occurs very slowly and is cyclical. For example, in irradiated contingents, there is a decrease in the amount of CD2DR+, which is eliminated only after 1-12 months, depending on the dose received. In some cases, even after 2 years, there was a persistence of a secondary immunodeficiency state.
In addition to the negative effect of the radiation factor on lymphocytes, the auxiliary cells of the immune system are damaged. In particular, the stroma, thymic epithelial cells are affected, which leads to a decrease in the production of thymosin and other thymic factors. As a result, sometimes even after 5 years, there is a decrease in the cellularity of the thymus cortex, a disorder in the synthesis of T-cells, the function of the peripheral organs of the lymphoid system is weakened, and the number of circulating lymphocytes is reduced. At the same time, antibodies are formed against thymus tissue, which leads to "radiation aging" of the immune system. There is also an increase in IgE synthesis, which increases the risk of developing allergic and autoimmune processes in the irradiated organism.
Evidence of the negative effect on the immune system of exposure is the change in the incidence of the inhabitants of Kyiv after the accident at the Chernobyl nuclear power plant. So, from 1985 to 1990, the incidence increased per 10,000 population: bronchial asthma- by 33.9%, bronchitis - by 44.2%, contact dermatitis- by 18.3%.
Characteristic was the formation of the following clinical syndromes.
1. Increasing susceptibility to respiratory infections, especially in patients with bronchial asthma and bronchitis, with an allergic component. The presence of inflammatory processes of an infiltrative nature in the lungs, subfebrile conditions, skin allergic reactions.
2. Hemorrhagic systemic vasculitis, lymphadenopathy, polymyalgia, polyarthralgia, fever of unknown origin, severe general weakness, mainly in young people.
3. "Syndrome of mucous membranes." This is a burning sensation, itching of the mucous membranes different localization(eyes, pharynx, oral cavity, genitals) in combination with an astheno-neurotic condition. At the same time, there are no visible changes in the mucous membranes. Microbiological examination of the mucous membranes reveals conditionally pathogenic microflora, more often staphylococcal and fungi.
4. Multiple intolerance syndrome a wide range substances of various nature (food, drugs, chemicals, etc.). This is most often observed in young women in combination with pronounced signs of autonomic dysregulation and asthenic syndrome.
2.2 Effect of ionizing radiation on immunity
Small doses of radiation do not seem to have a noticeable effect on the immune system. When animals are irradiated with sublethal and lethal doses, a sharp decrease in the body's resistance to infection occurs, which is due to a number of factors, among which the most important role is played by: a sharp increase in the permeability of biological barriers (skin, respiratory tract, gastrointestinal tract, etc.), inhibition of the bactericidal properties of the skin , blood serum and tissues, a decrease in the concentration of lysozyme in saliva and blood, a sharp decrease in the number of leukocytes in the bloodstream, inhibition of the phagocytic system, adverse changes in the biological properties of microbes permanently residing in the body - an increase in their biochemical activity, an increase in pathogenic properties, an increase in resistance and etc.
Irradiation of animals in sublethal and lethal doses leads to the fact that from large microbial reservoirs (intestines, respiratory tract, skin) a huge amount of bacteria enters the blood and tissues.! At the same time, a period of sterility is conditionally distinguished (its duration is one day), during which microbes are practically not detected in tissues; the period of contamination of regional lymph nodes (usually coincides with the latent period); the bacteremic period (its duration is 4--7 days), which is characterized by the appearance of microbes in the blood and tissues, and, finally, the period of decompensation of protective mechanisms, during which there is a sharp increase in the number of microbes in organs, tissues and blood (this period occurs a few days before death).
Under the influence of large doses of radiation, causing partial or complete death of all irradiated animals, the body is unarmed both to endogenous (saprophytic) microflora and exogenous infections. It is believed that during the height of acute radiation sickness, both natural and artificial immunity are greatly weakened. However, there are data indicating a more favorable outcome of the course of acute radiation sickness in animals subjected to immunization prior to exposure to ionizing radiation. At the same time, it has been experimentally established that vaccination of irradiated animals aggravates the course of acute radiation sickness, and for this reason it is contraindicated until the disease resolves. On the contrary, a few weeks after irradiation in sublethal doses, the production of antibodies is gradually restored, and therefore, already 1-2 months after exposure to radiation, vaccination is quite acceptable.
Radiobiologists have a very solid store of knowledge about the effect of high doses of ionizing radiation on biomacromolecules, cells, organisms, but they do not have sufficient data ...
Exposure to low doses of radiation
A huge number of new facts regarding the effects of radiation gave the tragic consequences of two grandiose radiation disasters: the South Urals in 1957 and Chernobyl in 1986 ...
Exposure to low doses of radiation
The outstanding Swedish radiobiologist R.M. Sievert came to the conclusion as early as 1950 that there is no threshold level for the action of radiation on living organisms. The threshold level is...
Effects of radiation on humans and the environment
It is believed that radiation in any dose is very dangerous. Its influence on a living organism can be both positive: use in medicine, and negative: radiation sickness. Interesting results were obtained by scientists ...
The effect of ionizing radiation on animals
In principle, all farm animals exposed to ionizing radiation can be divided into two categories. The first category includes animals that have received lethal doses of radiation ...
Natural radiation background
Features of the effects of radiation on living matter
The bulk of the radiation exposure of the world's population comes from natural sources radiation. Most of them are such that it is absolutely impossible to avoid radiation from them ...
Features of the impact of radiation on living matter
On average, approximately 2/3 of the effective equivalent dose of radiation that a person receives from natural sources of radiation comes from radioactive substances that enter the body with food, water and air ...
Features of the impact of radiation on living matter
In its latest report, UNSCEAR published for the first time in 20 years detailed overview information relating to acute damage to the human body, which occurs at high doses of radiation. Generally speaking, radiation has a similar effect...
Fission fragment environmental hazard assessment
The effect of radiation on the human body is called irradiation. During this process, the radiation energy is transferred to the cells, thereby destroying them. Irradiation can cause all sorts of diseases: infectious complications...
Ultimately allowable concentration harmful substances
The maximum permissible level (MPL) is the maximum level of exposure to radiation, noise, vibration, magnetic fields and other harmful physical influences, which does not pose a danger to human health, the condition of animals, plants ...
Solar radiation and its impact on natural and economic processes
Cytology and environmental protection
The impact of radiation on the body can be different, but almost always it is negative. In small doses, radiation can become a catalyst for processes leading to cancer or genetic disorders ...