1. Growth factors(macrophages, lymphocytes, fibroblasts, platelets, etc.) – stimulation of proliferation and limitation of apoptosis.
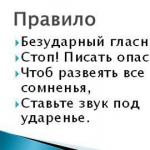
2. Keylons– glycoprotein tissue-specific growth inhibitors.
3. Fibronectin- fibroblast chemoattractant.
4. Laminin-the main adhesive protein of basement membranes.
5. Syndekan-integral proteoglycan cell membranes, binds collagen, fibronectin and thrombospondin.
6. Thrombospondin– glycoprotein, forms complexes with syndecan, collagen and heparin, plays a significant role in the assembly bone tissue.
The formation and implementation of the effects of biologically active substances (BAS) is one of the key links in inflammation. BAS ensure the natural development of inflammation, the formation of its general and local manifestations, as well as the outcome of inflammation. That is why biologically active substances are often referred to as "inflammatory mediators".
Inflammatory mediators- these are local chemical signals that are formed, released or activated at the site of inflammation, acting and destroyed also within the site. Inflammation mediators (mediators) are understood biologically active substances, responsible for the occurrence or maintenance of certain inflammatory phenomena, for example, increased vascular permeability, emigration, etc.
These are the same substances that, under conditions of normal functioning of the body, are formed in various organs and tissues in physiological concentrations and are responsible for the regulation of functions at the cellular and tissue level. During inflammation, being locally released (due to activation of cells and liquid media) in large quantities, they acquire a new quality - mediators of inflammation. Almost all mediators are also modulators of inflammation, i.e. they are capable of increasing or decreasing the severity of inflammatory phenomena. This is due to the complexity of their influence and their interaction both with the cells that produce these substances and with each other. Accordingly, the effect of a mediator can be additive (additive), potentiating (synergistic) and weakening (antagonistic), and the interaction of mediators is possible at the level of their synthesis, secretion or effects.
The mediator link is the main one in the pathogenesis of inflammation. It coordinates the interaction of many cells - effectors of inflammation, the change of cellular phases at the site of inflammation. Accordingly, the pathogenesis of inflammation can be imagined as a chain of multiple intercellular interactions regulated by mediators-modulators of inflammation.
Inflammatory mediators determine the development and regulation of alteration processes (including changes in metabolism, physicochemical parameters, structure and function), the development of vascular reactions, fluid exudation and emigration of blood cells, phagocytosis, proliferation and reparative processes at the site of inflammation.
Most mediators do their biological functions specifically affecting the receptors of target cells. However, some of them have direct enzymatic or toxic activity (eg, lysosomal hydrolases and reactive oxygen radicals). The functions of each mediator are regulated by corresponding inhibitors.
Blood plasma and inflammatory cells can serve as sources of inflammatory mediators. In accordance with this, 2 large groups of inflammatory mediators are distinguished: humoral and cellular. Humoral
mediators are mainly represented by polypeptides that constantly circulate in the blood in an inactive state and are synthesized mainly in the liver. These mediators make up the so-called "sentinel polysystem of blood plasma." Cellular mediators may be synthesized de novo (eg, arachidonic acid metabolites) or released from cellular stores (eg, histamine). The sources of cellular mediators at the site of inflammation are mainly macrophages, neutrophils and basophils.
Of the humoral mediators of inflammation, the most important are complement derivatives. Among the almost 20 different proteins formed during complement activation, its fragments C5a, C3a, C3b and the C5b-C9 complex are directly related to inflammation. At the same time, C5a and, to a lesser extent, C3a are mediators of acute inflammation. C3b opsonizes the pathogenic agent and accordingly promotes immune adhesion and phagocytosis. The C5b-C9 complex is responsible for the lysis of microorganisms and pathologically altered cells. The source of complement is blood plasma and, to a lesser extent, tissue fluid. Enhanced supply of plasma complement to the tissue is one of the important purposes of exudation. C5a, formed from it in plasma and tissue fluid under the influence of carboxypeptidase N, C5a des Arg and C3a increase the permeability of postcapillary venules. At the same time, C5a and C3a, being anaphylatoxins (i.e., liberators of histamine from mast cells), increase permeability both directly and indirectly through histamine. The effect of C5a des Arg is not associated with histamine, but is neutrophil-dependent, i.e., it is carried out due to permeability factors released from polymorphonuclear granulocytes - lysosomal enzymes and non-enzymatic cationic proteins, active oxygen metabolites. In addition, C5a and C5a des Arg attract neutrophils. In contrast, C3a has virtually no chemotactic properties. Active complement components release not only histamine and granulocyte products, but also interyaukin-1, prostaglandins, leukotrienes, platelet-activating factor, and interact synergistically with prostaglandins and substance P.
Kinins- vasoactive peptides formed from kininogens (alpha2-globulins) under the influence of kallikreins in plasma (nonapeptide bradykinin) and in tissue fluid (decapeptide lysylbradykinin, or kallidin). The triggering factor for the activation of the kallikrein-kinin system is the activation of Hageman factor (blood coagulation factor XII) during tissue damage, which converts prekallikreins into kallikreins.
Kinins mediate arteriolar dilation and increased venular permeability by contracting endothelial cells. They contract the smooth muscle of the veins and increase intracapillary and venous pressure. Kinins inhibit the emigration of neutrophils, modulate the distribution of macrophages, stimulate the migration and mitogenesis of T lymphocytes and the secretion of lymphokines. They also enhance fibroblast proliferation and collagen synthesis and, therefore, may be important in reparative phenomena and in the pathogenesis of chronic inflammation.
One of the most significant effects of kinins is the activation of reflexes by irritating the endings sensory nerves and thus mediating inflammatory pain. Kinins cause or enhance the release of histamine from mast cells and the synthesis of prostaglandins by many cell types, so some of their main effects - vasodilation, smooth muscle contraction, pain - are associated with the release of other mediators, especially prostaglandins.
Activation of the Hageman factor triggers not only the process of kinin formation, but also blood coagulation and fibrinolysis. In this case, mediators such as fibrinopeptides and fibrin degradation products are formed, which are powerful hemattractants. In addition, fibrinolysis and the formation of blood clots in the vessels of the lesion are essential in both the pathological and protective phenomena of inflammation.
Of the cellular mediators, the primary interest is eicosanoids since most likely they are the central mediator of the inflammatory reaction. This is supported by the long-term maintenance of eicosanoid production in the lesion, their close connection with key event inflammatory process- leukocyte infiltration, powerful anti-inflammatory effect of inhibitors of their synthesis.
The main role in the production of eicosanoids at the site of inflammation is played by leukocytes, especially monocytes and macrophages, although they are formed by almost all types of nuclear cells upon stimulation of the latter. The predominant eicosanoids at the site of inflammation are almost always prostaglandin (PG) E2, leukotriene (LT) B4 and 5-hydroxyeicosatetraenoic acid (5-HETE). Thromboxane (Tx) A2, PGF2alpha, PGD2, prostacyclin (PG12), LTC4, LTD4, LTE4, and other GETE are also formed, although in smaller quantities.
The main effects of eicosanoids on inflammation are their effects on leukocytes. PG, Tx and especially LT are powerful hemattractants and thus play an important role in the mechanisms of self-maintenance of leukocyte infiltration. PGs themselves do not increase vascular permeability, but, being strong vasodilators, they increase hyperemia and, consequently, exudation. LTS4, JITD4, LTE4 increase vascular permeability by direct contraction of endothelial cells, and LTV4 acts as a neutrophil-dependent mediator. PG and LT are important in the genesis of inflammatory pain. At the same time, PGE2, without having direct pain activity, increases the sensitivity of the receptors of afferent pain nerve endings to bradykinin and histamine. PGE2 is a potent antipyretic agent, and fever during inflammation may be due in part to its release. PGs play a key role in modulating the inflammatory process, carrying out bidirectional regulation of exudation, emigration and degranulation of leukocytes, and phagocytosis. For example, PGE can potentiate the development of edema caused by histamine or bradykinin, and PGF2alpha, on the contrary, can weaken it. A similar relationship between PGE and PGF2alpha also applies to leukocyte emigration.
Especially wide range interactions with other inflammatory mediators are characteristic of RT. They interact synergistically in relation to bronchospasm with histamine, acetylcholine, PG and Tx, and stimulate the release of PG and Tx. The modulatory function of eicosanoids is carried out through changes in the ratio of cyclic nucleotides in cells.
Sources histamine are basophils and mast cells. Serotonin(neurotransmitter) in humans, in addition to a small amount in mast cells, it is also found in platelets and enterochromaffin cells. Due to rapid release during mast cell degranulation , the ability to change the lumen of microvessels and cause direct contraction of endothelial cells of venules, histamine and serotonin are considered the main mediators of initial microcirculatory disorders in the focus of acute inflammation and the immediate phase of increased vascular permeability. Histamine plays a dual role in both blood vessels and cells. Through H2 receptors it dilates arterioles, and through H1 receptors it constricts venules and thus increases intracapillary pressure. Through Hi receptors, histamine stimulates, and through Hg receptors, it inhibits the emigration and degranulation of leukocytes. In the normal course of inflammation, histamine acts predominantly through Hg receptors on neutrophils, limiting their functional activity, and through Hi receptors on monocytes, stimulating them. Thus, in addition to pro-inflammatory vascular effects, it has anti-inflammatory cellular effects. Serotonin also stimulates monocytes at the site of inflammation. Histamine carries out bidirectional regulation of proliferation, differentiation and functional activity of fibroblasts and, therefore, may be important in reparative phenomena. The modulatory effects of histamine are also mediated by cyclic nucleotides.
As for the interactions of biogenic amines at the site of inflammation, it is known that histamine, through Hi receptors, can trigger or enhance the synthesis of prostaglandins, and through Na receptors, inhibit it. Biogenic amines interact both with each other and with bradykinin, nucleotides and nucleosides, and substance P to increase vascular permeability. The vasodilating effect of histamine is enhanced in combination with acetylcholine, serotonin, and bradykinin.
Main source lysosomal enzymes in the focus of inflammation are phagocytes - granulocytes and monocytes-macrophages. Despite the enormous importance of phagocytosis in the pathogenesis of inflammation, phagocytes are primarily mobile carriers of mediators-modulators secreted extracellularly. The release of lysosomal contents occurs during their chemotactic stimulation, migration, phagocytosis, damage, and death. The main components of lysosomes in humans are neutral proteinases - elastase, cathepsin G and collagenases contained in the primary, azurophilic, granules of neutrophils. In the processes of antimicrobial protection, including inflammation, proteinases are considered “second-order” factors after oxygen-dependent (myeloperoxidase - hydrogen peroxide) and oxygen-independent mechanisms such as lactoferrin and lysozyme. They provide mainly lysis of already killed microorganisms. The main effects of proteinases are mediation and modulation of inflammatory phenomena, including damage to one’s own tissues. The mediator and modulatory effects of proteinases occur in relation to vascular permeability, emigration, and phagocytosis.
An increase in vascular permeability under the influence of lysosomal enzymes occurs due to lysis of the subendothelial matrix, thinning and fragmentation of endothelial cells and is accompanied by hemorrhage and thrombosis. By forming or breaking down the most important chemotactic substances, lysosomal enzymes are modulators of leukocyte infiltration. First of all, this concerns the components of the complement system and kallikrein-kinin.
Lysosomal enzymes, depending on their concentration, can themselves enhance or inhibit neutrophil migration. In relation to phagocytosis, neutral proteinases also have a number of effects. In particular, elastase can form opsonin C3b; C3b is also important for particle adhesion to the neutrophil surface. Consequently, the neutrophil itself provides a mechanism for enhancing phagocytosis. Both cathepsin G and elastase increase the affinity of the neutrophil membrane Fc receptor for immunoglobulin complexes and, accordingly, enhance the efficiency of particle uptake.
Thanks also to the ability of lysosomal enzymes to activate the complement system, kallikrein-kinin, coagulation and fibrinolysis, and release cytokines and lymphokines, inflammation develops and is self-sustaining for a long time.
The most important property non-enzymatic cationic proteins, contained in both azurophilic and specific granules of neutrophils, is their high microbicidal properties. In this regard, they are in synergistic interaction with the myeloperoxidase - hydrogen peroxide system. Cationic proteins are adsorbed onto the negatively charged bacterial cell membrane through electrostatic interaction. As a result, the permeability and structure of the membrane are disrupted and the death of the microorganism occurs, which is a prerequisite for subsequent effective lysis by lysosomal proteinases. Extracellularly released cationic proteins mediate increased vascular permeability (mainly by inducing mast cell degranulation and histamine release), adhesion and emigration of leukocytes.
Main source cytokines(monokines) during inflammation are stimulated monocytes and macrophages. In addition, these polypeptides are produced by neutrophils, lymphocytes, endothelial and other cells. The most studied cytokines are interleukin-1 (IL-1) and tumor necrosis factor (TNF). Cytokines increase vascular permeability (in a neutrophil-dependent manner), adhesion and emigration of leukocytes. Along with pro-inflammatory properties, cytokines can also be important in the direct defense of the body, stimulating neutrophils and monocytes to kill, absorb and digest invading microorganisms, as well as enhancing phagocytosis by opsonizing the pathogenic agent.
By stimulating wound cleansing, cell proliferation and differentiation, cytokines enhance reparative processes. Along with this, they can mediate tissue destruction (degradation of the cartilage matrix and bone resorption) and thus play a role in the pathogenesis of diseases connective tissue, in particular rheumatoid arthritis.
The action of cytokines also causes a number of metabolic effects that underlie the general manifestations of inflammation - fever, drowsiness, anorexia, metabolic changes, stimulation of hepatocytes to increased protein synthesis acute phase, activation of the blood system, etc.
Cytokines interact with each other, with prostaglandins, neuropeptides and other mediators.
Inflammatory mediators also include a number lymphokines- polypeptides produced by stimulated lymphocytes. The most studied of the lymphokines that modulate the inflammatory response are macrophage inhibitory factor, macrophage-activating factor, and interleukin-2. Lymphokines coordinate the interaction of neutrophils, macrophages and lymphocytes, thus regulating the inflammatory response as a whole.
Active oxygen metabolites, First of all, free radicals - superoxide anion radical, hydroxyl radical HO, perhydroxyl, due to the presence of one or more unpaired electrons in their outer orbit, have increased reactivity with other molecules and, therefore, significant destructive potential, which is important in the pathogenesis of inflammation. The source of free radicals, as well as other oxygen-derived mediators and modulators of inflammation - hydrogen peroxide (H 2 0 2), singlet oxygen (f0 2), hypochloride (HOC1) are: the respiratory explosion of phagocytes during their stimulation, the arachidonic acid cascade in the process of eicosanoid formation, enzymatic processes in the endoplasmic reticulum and peroxysomes, mitochondria, cytosol, as well as autoxidation of small molecules such as hydroquinones, leukoflavins, catecholamines, etc.
The role of active oxygen metabolites in inflammation is, on the one hand, to increase the bactericidal ability of phagocytes and, on the other hand, in their mediator and modulatory functions. The mediator role of active oxygen metabolites is due to their ability to cause lipid peroxidation, oxidation of proteins, carbohydrates, and damage to nucleic acids. These molecular changes underlie the phenomena caused by active oxygen metabolites that are characteristic of inflammation - increased vascular permeability (due to damage to endothelial cells), stimulation of phagocytes.
Modulatory role , active oxygen metabolites may consist of both enhancing inflammatory phenomena (by inducing the release of enzymes and interacting with them in tissue damage; not only initiating, but also modulating the arachidonic acid cascade), and in anti-inflammatory effects (due to inactivation of lysosomal hydrolases and other inflammatory mediators ).
Reactive oxygen metabolites are important in maintaining chronic inflammation.
Mediators and modulators of inflammation also include neuropeptides- substances released by C-fibers as a result of activation by an inflammatory agent of multimodal nociceptors, which play an important role in the occurrence of axon reflexes in the terminal branches of primary afferent (sensitive) neurons. The most studied are substance P, calcitonin gene-related peptide, neurokinin A. Neuropeptides increase vascular permeability, and this ability is largely mediated by mediators derived from mast cells. Between unmyelinated nerves and mast cells there are membrane contacts that provide communication to the central nervous system with a focus of inflammation.
Neuropeptides interact synergistically to increase vascular permeability both among themselves and with histamine, bradykinin, C5a, platelet-activating factor, leukotriene B4; antagonistically - with ATP and adenosine. They also have a potentiating effect on the recruitment and cytotoxic function of neutrophils and enhance the adhesion of neutrophils to the endothelium of venules. In addition, neuropeptides increase the sensitivity of nociceptors to the action of various mediators, in particular prostaglandin E2 and prostacyclin, thus participating in the recreation of inflammatory pain.
In addition to the above substances, inflammatory mediators also include acetylcholiv and catecholamines, released upon stimulation of choline and adrenergic structures. Acetylcholine causes vasodilation and plays a role in the axon-reflex mechanism of arterial hyperemia during inflammation. Norepinephrine and adrenaline inhibit the growth of vascular permeability, acting mainly as modulators of inflammation.
. Chapter II
Cell reproduction. Problems cell proliferation in medicine.
2.1. Life cycle of a cell.
The cellular theory states that cells arise from cells by dividing the original. This position excludes the formation of cells from non-cellular matter. Cell division is preceded by reduplication of their chromosomal apparatus, DNA synthesis in both eukaryotic and prokaryotic organisms.
The time a cell exists from division to division is called the cell or life cycle. Its magnitude varies significantly: for bacteria it is 20-30 minutes, for a shoe 1-2 times a day, for an amoeba about 1.5 days. Multicellular cells also have different abilities to division. In early embryogenesis they divide frequently, and in the adult organism for the most part lose this ability as they become specialized. But even in an organism that has reached full development, many cells must divide to replace worn-out cells that are constantly sloughed off and, finally, new cells are needed to heal wounds.
Therefore, in some populations of cells, divisions must occur throughout life. Taking this into account, all cells can be divided into three categories:
1. By the time a child is born, nerve cells reach a highly specialized state, losing the ability to reproduce. During ontogenesis, their number continuously decreases. This circumstance also has one good side; if nerve cells divided, then higher nerve functions(memory, thinking) would be impaired.
2. Another category of cells is also highly specialized, but due to their constant exfoliation, they are replaced by new ones and this function is performed by cells of the same line, but not yet specialized and have not lost the ability to divide. These cells are called renewing cells. An example is the constantly renewed cells of the intestinal epithelium, hematopoietic cells. Even bone tissue cells can be formed from unspecialized ones (this can be observed during the reparative regeneration of bone fractures). Populations of unspecialized cells that retain the ability to divide are usually called stem cells.
3. The third category of cells is an exception, when highly specialized cells under certain conditions can enter the mitotic cycle. We are talking about cells that have a long lifespan and where, after complete growth, cell division occurs rarely. An example is hepatocytes. But if 2/3 of the liver is removed from an experimental animal, then in less than two weeks it is restored to its previous size. The same are the cells of the glands that produce hormones: under normal conditions, only a few of them are able to reproduce, and under altered conditions, most of them can begin to divide.
The cell cycle means the repeated repetition of sequential events over a certain period of time. Typically, cyclic processes are graphically depicted as circles.
The cell cycle is divided into two parts: mitosis and the interval between the end of one mitosis and the beginning of the next - interphase. The autoradiography method made it possible to establish that in interphase the cell not only performs its specialized functions, but also synthesizes DNA. This period of interphase is called synthetic (S). It begins approximately 8 hours after mitosis and ends after 7-8 hours. The interval between the S-period and mitosis was called presynthetic (G1 - 4 hours) after the synthetic period, before mitosis itself - postsynthetic (G2). happening over the course of about an hour.
Thus, there are four stages in the steel cell cycle; mitosis, G1 period, S period, G2 period.
Establishing the fact of DNA doubling in interphase means that during it the cell cannot perform specialized functions; it is busy building cellular structures, synthesis of building materials that ensure the growth of daughter cells, accumulation of energy expended during mitosis itself, synthesis of specific enzymes for DNA replication. Therefore, interphase cells, in order to fulfill their functions prescribed by the genetic program (become highly specialized), must temporarily or permanently leave the cycle during the G0 period, or remain in an extended G1 (no significant differences in the state of cells of the G0 and G1 periods were noted, since it is possible to return from G0 cells in a cycle). It should be especially noted that in multicellular mature organisms, the majority of cells are in the G0 period.
As already mentioned, the increase in the number of cells occurs only due to the division of the original cell, which is preceded by a phase of accurate reproduction of genetic material, DNA molecules, chromosomes.
Mitotic division includes new cell states: interphase, decondensed and already reduplicated chromosomes pass into the compact form of mitotic chromosomes, an achromatic mitotic apparatus is formed, which is involved in chromosome transfer, chromosomes diverge to opposite poles and cytokinesis occurs. The process of indirect division is usually divided into the following main phases: prophase, metaphase, anaphase and telophase. The division is conditional, since mitosis is a continuous process and the change of phases occurs gradually. The only phase that has a real beginning is anaphase, in which
chromosomes begin to separate. The duration of individual phases is different (on average, prophase and telophase - 30-40", anaphase and metaphase - 7-15"). At the beginning of mitosis, a human cell contains 46 chromosomes, each of which consists of 2 identical halves - chromatids (a chromatid is also called the S-chromosome, and a chromosome consisting of 2 chromatids is called the d-chromosome).
One of the most remarkable phenomena observed in mitosis is the formation of the spindle. It ensures the alignment of d-chromosomes in one plane, in the middle of the cell, and the movement of S-chromosomes to the poles. The spindle is formed by the centrioles of the cell center. Microtubules are formed in the cytoplasm from the protein tubulin.
In the G1 period, each cell contains two centrioles; by the time of the transition to the G2 period, a daughter centriole is formed near each centriole and a total of two pairs are formed.
In prophase, one pair of centrioles begins to move to one pole, the other to the other.
Between pairs of centrioles, a set of interpolar and chromosomal microtubules begins to form towards each other.
At the end of prophase, the nuclear membrane disintegrates, the nucleolus ceases to exist, chromosomes (d) spiral, the spindle moves to the middle of the cell and d-chromosomes find themselves in the spaces between the microtubules of the spindle.
During prophase, D chromosomes undergo a path of condensation from thread-like structures to rod-shaped ones. The shortening and thickening of (d-chromosomes continues for some time in metaphase, as a result of which metaphase d-chromosomes have sufficient density. A centromere is clearly visible in the chromosomes, separating them into equal or unequal shoulders, consisting of 2 S-chromosomes adjacent to each other (chromatids). At the beginning of anaphase, S chromosomes (chromatids) begin to move from the equatorial plane to the poles. Anaphase begins with the splitting of the centromeric region of each chromosome, as a result of which the two S chromosomes of each d chromosome are completely separated from one another. Thanks to this, each daughter cell receives an identical set of 46 S chromosomes. After centromere separation, one half of the 92 S chromosomes begins to move towards one pole, the other half towards the other.
To this day, it has not been established precisely under what forces the movement of chromosomes to the poles occurs. There are several versions:
1. The spindle contains actin-containing filaments (as well as other muscle proteins), it is possible that this force is generated in the same way as in muscle cells.
2. The movement of chromosomes is caused by the sliding of chromosomal microtubules along continuous (interpolar) microtubules with opposite polarity (McItosh, 1969, Margolis, 1978).
3. The speed of chromosome movement is regulated by kinetochore microtubules to ensure orderly segregation of chromatids. Most likely, all of the listed mechanisms for achieving a mathematically precise distribution of hereditary substance to daughter cells cooperate.
Towards the end of anaphase and the beginning of telophase, a constriction begins to form in the middle of the elongated cell; it forms the so-called cleavage furrow, which, going deeper, divides the cell into two daughter cells. Actin filaments take part in the formation of the furrow. But as the furrow deepens, the cells are connected to each other by a bundle of microtubules called the median body, the remainder of which is present for some time in interphase. Parallel to cytokinesis, chromosome decoiling occurs at each pole in the reverse order from the chromosomal to the nucleosomal level. Finally, the hereditary substance takes the form of clumps of chromatin, either tightly packed or decondensed. The nucleolus, nuclear envelope, surrounding chromatin and karyoplasm are formed again. Thus, as a result of mitotic cell division, the newly formed daughter cells are identical to each other and are a copy of the mother cell, which is important for the subsequent growth, development and differentiation of cells and tissues.
2.2. Mechanism of regulation of mitotic activity
Maintaining the number of cells at a certain, constant level ensures overall homeostasis. For example, the number of red blood cells and white blood cells in healthy body relatively stable, despite the fact that these cells die off, they are constantly replenished. Therefore, the rate at which new cells are formed must be regulated to match the rate at which they die.
To maintain homeostasis, it is necessary that the number of different specialized cells in the body and the functions they must perform be under the control of various regulatory mechanisms that maintain all this in a stable state.
In many cases, the cells are given a signal that they need to increase their functional activity, and this may require an increase in the number of cells. For example, if the Ca content in the blood drops, then the cells of the parathyroid gland increase the secretion of the hormone, and the calcium level reaches normal. But if the animal’s diet lacks calcium, then additional production of the hormone will not increase the content of this element in the blood. In this case, the cells thyroid gland begin to divide intensively, so that an increase in their number leads to a further increase in hormone synthesis. Thus, a decrease in a particular function can lead to an increase in the population of cells providing these functions.
In people who find themselves in high mountains, the number of red blood cells sharply increases (at an altitude of less than 02) in order to provide the body with the necessary amount of oxygen. Kidney cells react to a decrease in oxygen and increase the secretion of erythropoietin, which enhances hematopoiesis. After the formation of a sufficient number of additional red blood cells, hypoxia disappears and the cells producing this hormone reduce its secretion to normal levels.
Cells that are fully differentiated cannot divide, but their numbers can still be increased by the stem cells from which they originate. Nerve cells cannot divide under any circumstances, but they can increase their function by increasing their processes and multiplying the connections between them.
It should be noted that in adult individuals the ratio of overall sizes various organs remains more or less constant. When the existing ratio of organ sizes is artificially disrupted, it tends to normal (removal of one kidney leads to an increase in the other).
One of the concepts that explains this phenomenon is that cell proliferation is regulated by special substances called kelons. They are assumed to have cell specificity different types, organ tissues. It is believed that a decrease in the number of kelons stimulates cell proliferation, for example, during regeneration. Currently, this problem is being carefully studied by various specialists. Data have been obtained that keylons are glycoproteins with a molecular weight of 30,000 - 50,000.
2.3. Irregular types of cell reproduction
Amitosis. Direct division or amitosis, described earlier than mitotic division, but is much less common. Amitosis is the division of a cell in which the nucleus is in an interphase state. In this case, chromosome condensation and spindle formation do not occur. Formally, amitosis should lead to the appearance of two cells, but most often it leads to the division of the nucleus and the appearance of bi- or multinucleated cells.
Amitotic division begins with fragmentation of the nucleoli, followed by division of the nucleus by constriction (or invagination). There may be multiple nuclear fission, usually of unequal magnitude (with pathological processes). Numerous observations have shown that amitosis almost always occurs in cells that are obsolete, degenerating and unable to produce full-fledged elements in the future. So, normally, amitotic division occurs in the embryonic membranes of animals, in the follicular cells of the ovary, and in giant trophoblast cells. Positive value amitosis occurs in the process of tissue or organ regeneration (regenerative amitosis). Amitosis in aging cells is accompanied by disturbances in biosynthetic processes, including replication, DNA repair, as well as transcription and translation. Are changing physicochemical characteristics chromatin proteins of cell nuclei, the composition of the cytoplasm, the structure and functions of organelles, which entails functional disorders at all subsequent levels - cellular, tissue, organ and organismal. As destruction increases and restoration fades, natural cell death occurs. Amitosis often occurs during inflammatory processes and malignant neoplasms (induced amitosis).
Endomitosis. When cells are exposed to substances that destroy spindle microtubules, division stops, and chromosomes will continue the cycle of their transformations: replicate, which will lead to the gradual formation of polyploid cells - 4 p. 8 p., etc. This transformation process is otherwise called endoreproduction. The ability of cells to undergo endomitosis is used in plant breeding to obtain cells with a multiple set of chromosomes. For this purpose, colchicine and vinblastine are used, which destroy the filaments of the achromatin spindle. Polyploid cells(and then adult plants) differ large sizes, vegetative organs from such cells are large, with a large reserve nutrients. In humans, endoreproduction occurs in some hepatocytes and cardiomyocytes.
Another, rarer result of endomitosis is polytene cells. During polyteny in the S-period, as a result of replication and non-disjunction of chromosomal strands, a multi-stranded, polytene structure is formed. They differ from mitotic chromosomes in their larger size (200 times longer). Such cells are found in the salivary glands of dipteran insects and in the macronuclei of ciliates. On polytene chromosomes, swellings and puffs (transcription sites) are visible - an expression of gene activity. These chromosomes are the most important object of genetic research.
2.4. Problems of cell proliferation in medicine.
As is known, tissues with a high rate of cell turnover are more sensitive to the effects of various mutagens than tissues in which cells are renewed slowly. However, for example, radiation damage may not appear immediately and does not necessarily weaken with depth; sometimes it even damages deep-lying tissues much more than superficial ones. When cells are irradiated with X-rays or gamma rays, gross disturbances occur in the cell life cycle: mitotic chromosomes change shape, they break, followed by incorrect joining of fragments, and sometimes individual parts of chromosomes disappear altogether. Spindle anomalies may occur (not two poles in the cell, but three will form), which will lead to uneven divergence of chromatids. Sometimes cell damage (large doses of radiation) is so significant that all attempts by the cell to begin mitosis are unsuccessful and division stops.
This effect of radiation partly explains its use in tumor therapy. The goal of radiation is not to kill tumor cells in interphase, but to cause them to lose their ability to undergo mitosis, which will slow or stop tumor growth. Radiation in doses that are not lethal to the cell can cause mutations leading to increased proliferation of altered cells and give rise to malignant growth, as often happened to those who worked with X-rays, not knowing about their danger.
Cell proliferation is influenced by many chemical substances, including medications. For example, the alkaloid colchicine (contained in colchicum corms) was the first medicine, which relieved joint pain due to gout. It turned out that it also has another effect - stopping division by binding to tubulin proteins from which microtubules are formed. Thus, colchicine, like many other drugs, blocks the formation of the spindle.
On this basis, alkaloids such as vinblastine and vincristine are used to treat certain types of malignant neoplasms, becoming part of the arsenal of modern chemotherapeutic anticancer agents. It should be noted that the ability of substances such as colchicine to stop mitosis is used as a method for the subsequent identification of chromosomes in medical genetics.
Of great importance for medicine is the ability of differentiated (and germ) cells to maintain their potential for proliferation, which sometimes leads to the development of tumors in the ovaries, in the section of which cell layers, tissues, and organs are visible as a “mush”. Scraps of skin, hair follicles, hair, ugly teeth, pieces of bones, cartilage, nervous tissue, fragments of the eye, etc. are revealed, which requires urgent surgical intervention.
2.5. Pathology of cell reproduction
Mitotic cycle abnormalities.. The mitotic rhythm, usually adequate to the need for restoration of aging, dead cells, can be changed under pathological conditions. A slowdown of the rhythm is observed in aging or poorly vascularized tissues, an increase in the rhythm is observed in tissues under various types of inflammation, hormonal influences, in tumors, etc.
The cell is the elementary unit of all living things. There is no life outside the cell. Cell reproduction occurs only through division of the original cell, which is preceded by the reproduction of its genetic material. Activation of cell division occurs due to the influence of external or internal factors on it. The process of cell division from the moment of its activation is called proliferation. In other words, proliferation is the multiplication of cells, i.e. an increase in the number of cells (in culture or tissue) that occurs through mitotic divisions. The period of existence of a cell as such, from division to division, is usually called the cell cycle.
INTRODUCTION 3
CHAPTER I. Proliferation 4
Cell cycle 5
Cell cycle regulation 6
Exogenous regulators proliferation 7
Endogenous regulators of proliferation 7
CDK 8 regulatory pathways
Regulation G1 phase 10
S phase regulation 11
Regulation G2 phase 12
Regulation of mitosis 12
DNA Damage 13
1.10.1 Ways to repair DNA double-strand breaks 13
1.10.2 Cellular response to DNA damage and its regulation 14
1.11. Tissue regeneration 15
1.11.1 Forms of regeneration 16
1.11.2. Regulation of tissue regeneration 17
CHAPTER II. APOPTOSIS 18
2.1. Characteristic signs apoptosis 19
2.2. Mechanism of apoptosis 19
2.3. The role of apoptosis in protection against oncological diseases 20
2.4. Regulation of apoptosis 21
REFERENCES 24
The work contains 1 file
Russian State Pedagogical University named after A. I. Herzen
Faculty of Biology
COURSE WORK
Cell proliferation
St. Petersburg 2010
TABLE OF CONTENTS
INTRODUCTION 3
CHAPTER I. Proliferation 4
- Cell cycle 5
- Cell cycle regulation 6
- Exogenous regulators of proliferation 7
- Endogenous regulators of proliferation 7
- Pathways of CDK regulation 8
- G1 phase regulation 10
- S phase regulation 11
- G2 phase regulation 12
- Regulation of mitosis 12
- DNA damage 13
1.10.1 Pathways to repair DNA double-strand breaks 13
1.10.2 Cellular response to DNA damage and its regulation 14
1.11. Tissue regeneration 15
1.11.1 Forms of regeneration 16
1.11.2. Regulation of tissue regeneration 17
CHAPTER II. APOPTOSIS 18
2.1. Characteristic signs of apoptosis 19
2.2. Mechanism of apoptosis 19
2.3. The role of apoptosis in protection against cancer 20
2.4. Regulation of apoptosis
21
BIBLIOGRAPHY 24
Introduction
The cell is the elementary unit of all living things. There is no life outside the cell. Cell reproduction occurs only through division of the original cell, which is preceded by the reproduction of its genetic material. Activation of cell division occurs due to the influence of external or internal factors on it. The process of cell division from the moment of its activation is called proliferation. In other words, proliferation – this is cell reproduction, i.e. an increase in the number of cells (in culture or tissue) that occurs through mitotic divisions. The lifetime of a cell as such, from division to division, is usually calledcell cycle.
In the adult human body, cells of different tissues and organs have different abilities to divide. In addition, with aging, the intensity of cell proliferation decreases (i.e., the interval between mitoses ). There are populations of cells that have completely lost the ability to divide. These are, as a rule, cells that are at the terminal stagedifferentiation, for example, mature neurons, granular blood leukocytes, cardiomyocytes . In this regard, the exception is immuneMemory B and T cells, which, being in the final stage of differentiation, when a certain stimulus appears in the body in the form of a previously encountered antigen , are able to begin to proliferate. The body has constantly renewing tissues - various types of epithelium, hematopoietic tissues. In such tissues there is a pool of cells that constantly divide, replacing spent or dying cell types (for example,intestinal crypt cells, cells of the basal layer of the integumentary epithelium, hematopoietic cells bone marrow ). There are also cells in the body that do not reproduce in normal conditions, but again acquire this property under certain conditions, in particular, if necessary regeneration tissues and organs.
The process of cell proliferation is tightly regulated by both the cell itself (regulation of the cell cycle, cessation or slowdown of synthesis autocrine growth factors and their receptors), and its microenvironment (lack of stimulating contacts with neighboring cells and matrix, cessation of secretion and/or synthesis paracrine growth factors). Dysregulation of proliferation leads to unlimited cell division, which in turn initiates the development of the oncological process in the body.
Proliferation
The main function associated with the initiation of proliferation is assumed byplasma membranecells. It is on its surface that events occur that are associated with the transition of resting cells to an activated state that precedes division. Plasma membrane cells, due to the receptor molecules located in it, perceives various extracellular mitogenic signals and ensures transport into the cell of the necessary substances involved in the initiation of the proliferative response. Mitogenic signals can be contacts between cells, between a cell and a matrix, as well as the interaction of cells with various compounds that stimulate their entry into cell cycle , which are called growth factors. A cell that has received a mitogenic signal to proliferate starts the process of division.
Cell cycle
Entire cell cycle consists of 4 stages: presynthetic (G1),
synthetic (S), postsynthetic (G2) and mitosis proper (M).
In addition, there is a so-called G0 period, which characterizes
cell resting state. In the G1 period, cells have diploid
DNA content per nucleus. During this period, cell growth begins
mainly due to the accumulation of cellular proteins, which is due to
increasing the amount of RNA per cell. In addition, preparations for DNA synthesis begin. In the next S-period the quantity doubles DNA and accordingly the number of chromosomes doubles. The post-synthetic G2 phase is also called premitotic. In this phase, active synthesis occurs mRNA (messenger RNA). This stage is followed by the cell division itself, or mitosis.
Division of all eukaryotic cellsassociated with the condensation of doubled (replicated) chromosomes. As a result of division these chromosomes are transferred to daughter cells. This type of division of eukaryotic cells - mitosis (from the Greek mitos - threads) - is the only complete way to increase the number of cells. The process of mitotic division is divided into several stages: prophase, prometaphase, metaphase, anaphase, telophase.
Cell cycle regulation
The purpose of the regulatory mechanisms of the cell cycle is not to regulate the passage of the cell cycle as such, but to ensure, ultimately, the error-free distribution of hereditary material during the process of cell reproduction. The regulation of cell reproduction is based on the change in states of active proliferation andproliferative dormancy. Regulatory factors that control cell reproduction can be divided into two groups: extracellular (or exogenous) or intracellular (or endogenous).Exogenous factorsare located in the cell microenvironment and interact with the cell surface. Factors that are synthesized by the cell itself and act inside it are referred to as
endogenous factors. This division is very arbitrary, since some factors, being endogenous in relation to the cell producing them, can leave it and act as exogenous regulators on other cells. If regulatory factors interact with the same cells that produce them, then this type of control is called autocrine. With paracrine control, the synthesis of regulators is carried out by other cells.
Exogenous regulators of proliferation
In multicellular organisms, the regulation of the proliferation of various cell types occurs due to the action of not one growth factor, but a combination of them. In addition, somegrowth factors, being stimulators for some types of cells, behave as inhibitors in relation to others. Classicgrowth factorsrepresent polypeptides with a molecular weight of 7-70 kDa. To date, more than a hundred such growth factors are known.
PDGF platelets. Freed by destruction vascular wall PDGF is involved in the processes of thrombus formation and wound healing. PDGF is a powerful growth factor for dormant fibroblasts . Along with PDGF, epidermal growth factor has been studied no less thoroughly ( EGF ), which is also capable of stimulating fibroblast proliferation. But, in addition to this, it also has a stimulating effect on other types of cells, in particular on chondrocytes.
A large group of growth factors are cytokines (interleukins, tumor necrosis factors, colony-stimulating factorsetc.). All cytokines are multifunctional. They can either enhance or inhibit proliferative responses. For example, different subpopulations of CD4+ T lymphocytes, Th1 and Th2 , producing a different spectrum of cytokines, are antagonists towards each other. That is, Th1 cytokines stimulate the proliferation of cells that produce them, but at the same time suppress the division of Th2 cells, and vice versa. Thus, normally the body maintains a constant balance of these two types of T-lymphocytes. The interaction of growth factors with their receptors on the cell surface leads to the launch of a whole cascade of events inside the cell. As a result, transcription factors are activated and proliferative response genes are expressed, which ultimately initiates DNA replication and the cell enters mitosis.
Endogenous regulators of the cell cycle
In normal eukaryotic cells, progression through the cell cycle is tightly regulated. Reasononcological diseases is a transformation of cells, usually associated with violations of the regulatory mechanisms of the cell cycle. One of the main results of cell cycle defects is genetic instability, since cells with defective cell cycle control lose the ability to correctly duplicate and distribute theirgenome . Genetic instability leads to the acquisition of new features that are responsible for tumor progression.
Proliferative processes during acute inflammation begin soon after the influence of the phlogogenic factor on the tissue and are more pronounced along the periphery of the inflammation zone. One of the conditions for the optimal course of proliferation is the attenuation of the processes of alteration and exudation.
Proliferation
Phagocytes also produce and release into the intercellular fluid a number of biologically active substances that regulate the development of either immunity, allergies, or a state of tolerance. Thus, inflammation is directly related to the formation of immunity or immunopathological reactions in the body.
Proliferation - a component of the inflammatory process and its final stage - is characterized by an increase in the number of stromal and, as a rule, parenchymal cells, as well as the formation intercellular substance at the site of inflammation. These processes are aimed at the regeneration of altered and/or replacement of destroyed tissue elements. Various biologically active substances, especially those stimulating cell proliferation (mitogens), are essential at this stage of inflammation.
The forms and degree of proliferation of organ-specific cells are different and are determined by the nature of the cell populations (see the article “Cell Population” in the Appendix “Reference of Terms”).
In some organs and tissues (for example, liver, skin, gastrointestinal tract, respiratory tract) cells have a high proliferative ability, sufficient to eliminate structural defects in the inflammation site.
In other organs and tissues this ability is very limited (for example, in tissues of tendons, cartilage, ligaments, kidneys, etc.).
In a number of organs and tissues, parenchymal cells have virtually no proliferative activity (for example, cardiac muscle myocytes, neurons). In this regard, upon completion of the inflammatory process in the tissues of the myocardium and nervous system, stromal cells, mainly fibroblasts, which also form non-cellular structures, proliferate at the site of inflammation. As a result, a connective tissue scar is formed. At the same time, it is known that parenchymal cells of these tissues have high ability to hypertrophy and hyperplasia of subcellular structures.
Activation of proliferative processes correlates with the formation of biologically active substances that have an anti-inflammatory effect (a kind of anti-inflammatory mediators). The most effective among them include:
Inhibitors of hydrolases, in particular proteases (for example, antitrypsin), microglobulin, plasmin or complement factors;
Antioxidants (eg, ceruloplasmin, haptoglobin, peroxidases, SOD);
Polyamines (eg putrescine, spermine, cadaverine);
Glucocorticoids;
Heparin (suppresses adhesion and aggregation of leukocytes, activity of kinins, biogenic amines, complement factors).
Replacement of dead and damaged tissue elements during inflammation is noted after their destruction and elimination (this process is called wound cleansing).
The proliferation reactions of both stromal and parenchymal cells are regulated by various factors. The most significant among them include:
Many inflammatory mediators (for example, TNF, which suppresses proliferation; leukotrienes, kinins, biogenic amines, which stimulate cell division).
Specific metabolic products of leukocytes (for example, monokines, lymphokines, ILs, growth factors), as well as platelets, that can activate cell proliferation.
Low molecular weight peptides released during tissue destruction, polyamines (putrescine, spermidine, spermine), as well as nucleic acid breakdown products that activate cell reproduction.
Hormones (GH, insulin, T4, corticoids, glucagon), many of them capable of both activating and suppressing proliferation depending on their concentration, activity, synergistic and antagonistic interactions; for example, glucocorticoids in low doses inhibit, and mineralocorticoids activate regeneration reactions.
Proliferation processes are also influenced by a number of other factors, for example, enzymes (collagenase, hyaluronidase), ions, neurotransmitters and others.