Cyanosis is a darkening of the skin with a blue tint caused by circulatory or metabolic disorders. Develops when the level of reduced hemoglobin increases above 30 g/l. Blood that has a low oxygen concentration is dark in color. It easily shines through the skin and creates a blue tint, which is clearly visible on the face and limbs.
Classification
According to the mechanism of occurrence, cyanosis can be:
- true – in case of impaired blood oxygenation;
- false – when dyes enter the body.
According to the prevalence, cyanosis of the skin can be general (spreads over the entire surface of the body) and local (in a specific area of the body). Generalized cyanosis occurs with pulmonary embolism or airway obstruction. Acrocyanosis (discoloration of the upper half of the body - face, neck) occurs in chronic diseases of the heart and lungs. They also emit red cyanosis, which is formed due to carbon monoxide poisoning.
Depending on the speed of occurrence, it may be as follows:
- Spicy.
- Subacute.
- Chronic.
Depending on the main reason that led to cyanosis, there are:
- respiratory cyanosis;
- cardiac;
- hematological;
- cerebral;
- metabolic.
Causes
In most cases, cyanosis occurs against the background of diseases of the body, and not as an independent symptom. The main factors that lead to its development are:
- Emergency and critical conditions - pulmonary embolism, pulmonary edema, obstruction of the upper respiratory tract, cardiac tamponade, poisoning with poisons (carbon monoxide, sulfonamides), pulmonary atelectasis, intracerebral hemorrhage, cerebral edema.
- Acute diseases – pneumonia, sepsis, convulsive syndrome.
- Chronic diseases - pulmonary hypertension, coronary heart disease, chronic obstructive pulmonary disease, interstitial fibrosis, congenital heart defects, bronchial asthma, anemia, thrombosis of the lower extremities, polycythemia, varicose veins.
In young children, including newborns, cyanosis occurs in the following cases: congenital heart defects, congenital pneumonia, aspiration asphyxia. In the first days of life, all children experience cyanosis, which disappears on its own after a short period of adaptation (1-2 days).
There are localizations of cyanosis that may indicate a specific disease. We list the main ones:
- in the navel area - with acute pancreatitis;
- on the hands and forearm - with Cassirer's angioneurosis;
- distal phalanges of the fingers - with Raynaud's syndrome.
Degrees
Depending on the severity of the underlying disease, its manifestation on the skin can have the following degrees:
- The first is that the symptom appears only during physical activity or stress. The color of the skin is quickly restored to normal.
- The second is that cyanosis on the face is constantly observed; it can periodically occur in the periphery (arms, chest).
- The third is a change in color of the entire surface of the skin, which is difficult to treat.
Additional symptoms
Cyanosis may be accompanied by the following symptoms:
- rapid breathing, cough, foamy sputum, wheezing, difficulty inhaling or exhaling;
- changes in the shape of the chest (heart hump), nails (watch glasses), fingers (drumsticks);
- heartbeat;
- dizziness;
- swelling of the lower extremities, cold snap, trophic disorders, decreased sensitivity;
- increased body temperature, chills, sweating, general weakness.
Diagnostics
The most common causes of cyanosis in adults are heart and lung diseases. To establish a diagnosis, it is necessary to carry out the following examinations:
- study of blood gas composition;
- pulse oximetry;
- determination of hemoglobin and red blood cells in a blood test;
- spirography;
- chest x-ray. You can see the expansion of the heart shadow, changes in the pulmonary pattern, signs of congestion in the lungs;
- electrocardiography. Detects the presence of hypertrophy of the right or left parts of the heart;
- Ultrasound of the heart;
- computed tomography of the chest.
Treatment
Considering that the color of the skin changes under the influence of internal processes, symptomatic treatment is not effective. Once the diagnosis is made, specific treatment is carried out.
In case of poisoning, detoxification therapy is carried out in a hospital setting. Obstruction of the airways requires removal of the foreign body, and if tracheotomy is not possible, cricothyrotomy. Entry of air or fluid into the pleural cavity is treated with drainage or puncture.
Congenital blood diseases associated with impaired hemoglobin transport are eliminated with ascorbic acid in age-related doses. Heart defects are subject to surgical treatment. In the treatment of pulmonary and cardiac diseases that lead to bluish skin, the following is used:
- thrombolytics, anticoagulants, antiplatelet agents;
- antibacterial drugs (in the presence of pneumonia, sepsis);
- diuretics;
- defoamers;
- bronchodilators;
- cardiac glycosides;
- metabolic agents to improve cerebral blood flow;
- respiratory analeptics;
- glucocorticoids.
In almost all cases, the following measures are effective:
- Carrying out oxygen therapy using a mask, probe, pillow, oxygen tent.
- Using an oxygen cocktail - a foamy substance found in an oxygen cylinder.
- Artificial ventilation.
In conclusion, it must be said that cyanosis is an important diagnostic sign. By its nature and distribution, hidden diseases and pathological processes can be identified. If cyanosis occurs for the first time, does not go away within several hours, increases, and the general condition worsens, seek medical help immediately. Be healthy!
Some diseases are quite easily diagnosed by external manifestations. During the examination, the doctor immediately draws attention to the presence of some characteristic signs that indicate pathologies in the functioning of the internal organs. One of these manifestations is cyanosis of the skin.
What is cyanosis?
This is the appearance of an unnatural blue tint on some areas of the skin and mucous membranes. Cyanosis can occur not only in childhood, but also in adults (in the presence of certain diseases). From a medical point of view, cyanosis, or cyanosis, is caused by an increase in the content of pathological hemoglobin in the blood.
The blood is poorly saturated with oxygen and does not reach some areas of the body in the required volume, which provokes cyanosis of the skin.
Important. This condition can be quite dangerous. If you do not provide immediate assistance, it is fraught with serious complications, even death.
With poor blood supply to the capillaries, cyanosis develops - cyanosis of the hands, feet, and nose appears. The degree of manifestation of the symptom depends on the pathology that provoked this condition.
Causes of cyanosis
Doctors divide this condition into two types:
- Central (or diffuse) cyanosis.
- Peripheral.
The central type is caused by insufficient saturation of arterial blood with oxygen. The reasons may be the following:
- Diseases of the respiratory and cardiovascular systems.
- Congenital heart muscle defect.
- Intoxication of the body, which provokes the formation of methemoglobin.

- Low speed of blood movement in the capillaries.
Need to know. Rising to an unusual altitude can provoke this condition due to a decrease in atmospheric pressure.
Peripheral cyanosis occurs due to problems with local blood circulation and leads to the appearance of blueness of the fingers and face. The reasons for this condition may be:
- Poor arterial patency.
- The presence of thrombophlebitis of the extremities.

The following diseases and conditions can also cause cyanosis:
- Asthma.
- Emphysema.
- Pneumonia.
- Abdominal cyanosis may be a symptom of acute pancreatitis.
- Taking increased doses of drugs.
- Prolonged cramps.
- Epilepsy.
- Anaphylactic shock.
- Infectious diseases.
- Carcinoid of the small intestine.
Need to know. In a healthy person, the cause of cyanosis of the face or extremities can be hypothermia or being in a stuffy room.

Cyanosis is often diagnosed in newborns, which usually indicates the presence of malformations of the cardiovascular system, lungs, or neurological problems.
Symptoms of cyanosis
Cyanosis of the face and limbs often occurs in newborn babies. The following manifestations may occur:
- Blue tint of nail plates.
- Blueness of the child's feet and fingers.
- The nasolabial triangle takes on a bluish tint.
- The mucous membranes turn blue.
Important! The degree of cyanosis can be expressed in different ways, and the stronger the manifestation, the more serious the child’s condition, and urgent help is required. For example, cyanosis in heart failure without assistance can be fatal.
Signs of cyanosis may differ depending on the cause that provoked it. The following can be noted:
- If there is pathology of the lungs, then cyanosis is manifested by the blue-violet color of the lips and nasolabial triangle. This indicates a lack of oxygen. The condition may be accompanied by fever and sweating.

- In the presence of heart defects and heart failure, in addition to blueness of the lips and mucous membranes, thickening of the phalanges of the fingers, the appearance of wheezing, and shortness of breath can be noted.

Finger pads turn blue and their shape changes - one of the signs of heart disease
Important. Cyanosis in newborns is often caused by physiological reasons. If the symptoms are pronounced and do not disappear for a long time, then the help of doctors is required.

Cyanosis itself does not require special therapy, but the lack of treatment for the diseases that provoked it can result in the development of serious complications. The nervous system is affected, the body's resistance decreases, sleep problems appear, and appetite disappears. In the most severe cases, the patient may fall into a coma.
Diagnosis of pathology
There is no direct treatment for cyanosis. To eliminate all symptoms, it is necessary to identify the provoking disease and get rid of it. To do this, the first thing you need to do is go to the doctor.
The doctor's actions will be as follows:
- Examining the patient and listening to complaints.
- The doctor finds out when the signs appeared, whether they are constant or occur periodically.
- The doctor finds out the presence of chronic pathologies.
- Prescribes special studies, such as:
- General blood analysis.
- Determination of blood gas composition.
- Pulse oximetry.

- The speed of blood flow is determined.
- A study of the functioning of the lungs and heart is carried out.
- X-ray examination.
- Computed tomography of the chest.
Remember. Only after establishing the cause of cyanosis can treatment begin that will help eliminate the manifestations of this condition.
Treatment of cyanosis
What is an attack of cyanosis, how does it manifest itself is clear, but how to provide help, are there special methods of therapy? Treatment of such a condition should be aimed at eliminating the disease that provoked its appearance.
The main areas of therapy can be identified:
- Oxygen therapy.
- Treatment with drugs.
- Traditional methods.
Drug therapy
Since this condition is often associated with circulatory problems, the use of medications aims to improve the supply of oxygen to tissues and organs. Doctors recommend that patients start taking medications to enhance cardiac activity, normalize blood flow, and improve its properties.
To eliminate the symptoms of cyanosis, the following is prescribed:
- Bronchodilators, e.g. "Berodual".

- Antihypoxants ( "Actovegin").
- Heart medications ( "Korglikon", "Strofanthin").
- Anti-clotting agents ( "Warfarin", "Fragmin").
- Vitamin preparations.
Need to know. If, as a result of diagnosis, it is determined that the cause of cyanosis is a congenital heart defect, then the symptoms can only be eliminated through surgery.
Oxygen treatment
The use of oxygen therapy can reduce the appearance of cyanosis. A special oxygen mask is used to saturate the blood. If there is heart or pulmonary failure, then this method helps to significantly improve the condition of patients. An attack of cyanosis after physical activity practically disappears after oxygen is supplied.

Oxygen cocktails are also often used. They are foam saturated with oxygen. The product has the following effects:
- Vitality is restored.
- Cells and tissues are saturated with oxygen.
- Metabolic processes improve.
- The quality of life of patients improves.

You can purchase an oxygen canister and prepare such cocktails at home.
Use of traditional methods of treatment
There are quite a lot of traditional methods, but they must be used taking into account the reason that caused the development of cyanosis:
- If the cause of the appearance of cyanosis of the skin is a decrease in the speed of blood flow, then you can use a mask made from honey and aloe juice, taken in equal parts. Apply the composition to the blue areas.
- If cyanosis of the legs occurs due to thrombophlebitis, horse chestnut can come to the rescue. It is necessary to prepare an infusion from the shell of the fruit. Pour the dried raw material with water and leave for 12 hours, and then bring to a boil. After complete cooling, take 1 tablespoon before meals (three times a day). The course of treatment should be at least 2 weeks.

Plant “helpers” help cope with many pathologies
- If the cause of cyanosis is poisoning, then viburnum will help cope with the symptoms. This plant perfectly removes toxic substances from the body. You can use not only fruits, but also leaves. The raw material must be poured with a liter of water and boiled for at least an hour, and then taken between meals.
Advice. All traditional medicine should be used for therapy only after visiting a doctor.
Prevention of cyanosis
Essentially, to prevent symptoms of cyanosis from occurring, you must:
- Lead a healthy lifestyle.
- Play sports, but in moderation.
- Eat properly.
- Be outdoors more often.
- Monitor your health and prevent hypothermia.
Blue discoloration of the skin (cyanosis) is a sign of insufficient oxygen concentration in the bloodstream. It indicates that there is an increased amount of hemoglobin in the blood, deprived of oxygen.

Causes of blue skin
There is peripheral cyanosis, in which there is a violation of blood circulation in a certain area of the body - lips, cheeks, ears, tip of the nose or fingers. With central cyanosis, the skin and mucous membranes become bluish. In any case, blue skin indicates insufficient oxygen saturation of the blood.
Cyanosis is a serious sign of respiratory failure, which develops for many reasons:
- from the respiratory tract, these are bronchial asthma, pneumosclerosis, pneumonia, bronchiolitis, pulmonary diseases, tuberculosis, pulmonary embolism. The consequence is left ventricular failure with possible pulmonary edema;
- occupational bronchitis (anthracosis, silicatosis, asbestosis);
- cardiovascular diseases (myocardial infarction, heart defects, pericarditis);
- mediastinal tumors, superior vena cava syndrome;
- poisoning, intoxication syndrome with the appearance of methemoglobin, sulfhemoglobin.
Attention should also be paid to symptoms accompanying cyanosis, such as shortness of breath, cough with sputum, hemoptysis, chest pain, pyrexia and high blood pressure.
Depending on the cause of respiratory failure, during auscultation of the lungs, moist rales of various sizes, weakened breathing or crepitus are heard.
With insufficient oxygen saturation of the blood, hypoxia of the brain is observed, which is manifested by encephalopathy, confusion, and even hypoxic coma.
If cyanosis is noticed on the lower extremities, there is reason to suspect chronic venous insufficiency. It is possible with varicose veins, thrombophlebitis and phlebothrombosis.
Diagnosis of blue skin
If cyanosis of the skin appears, you should consult a pulmonologist. He will analyze the complaints, conduct auscultation of the lungs and determine the tactics for further examination.
Using a pulse oximeter, the level of saturation (oxygen saturation in the blood) is recorded, which, in combination with other instrumental methods, makes it possible to assess the degree of respiratory failure.
In addition, a chest X-ray, tomography, and, if a tumor formation is detected, a puncture followed by a cytological analysis are performed. Spirography is also performed to assess the effectiveness of respiratory function.
If necessary, a consultation with a cardiologist, ECG and ultrasound examination of the heart are prescribed.
If cyanosis is observed exclusively in the lower extremities, you should contact a phlebologist or vascular surgeon.
Among instrumental methods, ultrasound Dopplerography of veins is used, with the help of which the venous wall, blood clots are visualized, and the condition of the valve apparatus is assessed.
Treatment of cyanosis
First aid for cyanosis and shortness of breath is to provide the patient with access to oxygen and a sitting position. Depending on the cause of cyanosis, the doctor prescribes bronchodilators, mucolytics, anticoagulants or hormonal agents, and, if necessary (for lung cancer, heart defects), surgery is performed.
Blue skin is a harbinger of respiratory failure, so if a symptom appears, you should rush to see a doctor.
Cyanosis of the skin or mucous membranes is a bluish discoloration of the skin or mucous membranes that occurs in response to an increase in the level of hemoglobin uncombined with oxygen (deoxyhemoglobin) in the blood. The appearance of this color is due to a change in the color of the blood, which becomes dark in color when the oxygen content is low. This discoloration is most noticeable on the mucous membranes or on the thinnest areas of the skin (fingers, ears, face, neck).
Cyanosis is not a separate disease. This symptom can occur with various ailments and is most often provoked specifically by the respiratory system. In some cases, its appearance may signal a critical condition and the need for emergency care, and in others it may indicate the development or progression of an acute or chronic disease that requires treatment. The only variant of the physiological norm for the appearance of cyanosis of the skin is its occurrence during prolonged exposure to high altitude. In such situations, the color of the skin changes due to the body's protective reaction. This process is not dangerous to health, eliminates itself and does not require therapy.
In this article, we will introduce you to the main causes, types, manifestations, and methods of treating cyanosis of the skin and mucous membranes. This information will help you suspect problems in the body in time, and you will be able to take the necessary measures to restore your health.
Cyanosis of the skin and mucous membranes is often observed in diseases of the heart and blood vessels, when blood cannot be fully delivered to the cells of organs and tissues. This circulatory disorder leads to the development of hypoxia in the skin. As a result, the mucous membranes and skin acquire a bluish tint. The following symptoms may precede the appearance of such a sign of cardiovascular diseases:
- increased fatigue;
- headache;
- sleep disorders, etc.
Similar circulatory disorders can be observed in many pathologies of the heart and blood vessels: thrombosis, and such complications of heart disease as and.
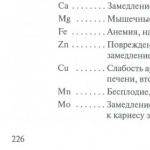
Other causes of cyanosis may be the following diseases and conditions:
- pathologies of the respiratory system: pneumonia, pneumothorax, pleurisy, bronchial asthma, emphysema, chronic obstructive pulmonary disease, foreign bodies in the respiratory system, pulmonary infarction, respiratory failure, etc.;
- blood pathologies: anemia, polycythemia;
- seizures and epilepsy;
- Quincke's edema or anaphylactic shock;
- drug overdose;
- poisoning with drugs or poisons: alcohol, nitrites, aniline, sulfonamides, phenacytin, sedatives, drugs with nitrobenzene;
- food poisoning;
- infections: plague, cholera;
- small intestinal carcinoid;
- hereditary forms of methemoglobinemia;
- frostbite or hypothermia;
- injuries with tissue compression;
- being in a stuffy room.
Cyanosis in newborns can develop in the following cases:
- aspiration asphyxia;
- congenital heart defects;
- congenital pneumonia.
In some cases, in newborns, cyanosis is a variant of the norm and is caused by incompletely stopped embryonic circulation. It goes away completely without any treatment after a short adaptation period (about 1-2 days).
Classification
 Peripheral cyanosis. On the left - normal skin color, on the right - cyanotic brush
Peripheral cyanosis. On the left - normal skin color, on the right - cyanotic brush Depending on the origin, cyanosis can be of the following types:
- cardiac - caused by unproductive blood circulation and insufficient blood supply to the tissues and oxygen deficiency;
- respiratory - caused by an insufficient amount of oxygen in the lungs and a violation of its flow into the blood, other tissues and organs;
- cerebral - caused by the inability to attach oxygen to hemoglobin and leads to ischemia of brain cells;
- hematological – caused by blood pathologies;
- metabolic - caused by a violation of oxygen absorption by tissue cells.
As a rule, only respiratory cyanosis can disappear 10 minutes after oxygen therapy. Other types last longer.
Depending on the speed of appearance of cyanosis, it happens:
- spicy;
- subacute;
- chronic.
According to the nature of distribution, experts distinguish the following types of cyanosis:
- central (or diffuse) - manifests itself over the surface of the entire body, caused by impaired respiratory function or general circulatory disorders;
- peripheral - provoked by dysfunction of the heart or arteries and the development of ischemia of the tissues of the arms, legs or face;
- acrocyanosis - cyanosis appears only at the “extreme points” (fingertips, wings of the nose, ears, lips), its appearance is provoked by venous stagnation and is observed in chronic heart failure;
- local - detected during examination of the nasopharynx, pharynx or genitals and is caused by stagnation of blood.
Manifestations of cyanosis
Cyanosis itself does not affect general well-being, but the causes that cause it always need to be eliminated and are a reason to consult a doctor. In some cases, the occurrence of cyanosis indicates the development of critical conditions and the need to provide emergency care to the patient. In this condition, cyanosis appears suddenly, is clearly expressed and increases rapidly.
Depending on the cause of its appearance, cyanosis is accompanied by various symptoms: fever, cough, shortness of breath, tachycardia, pain, intoxication and other signs. It is from them that the doctor can make a diagnosis and determine further treatment tactics.
Cyanosis itself does not require therapy. It is eliminated after the start of treatment of the underlying disease and oxygen therapy. Subsequently, a decrease in its manifestations will indicate the effectiveness of the measures taken.
Diagnostics
To identify the cause of cyanosis, the doctor determines the area of its localization, listens to the patient’s complaints and analyzes his medical history. The following points must be clarified:
- when and under what circumstances did cyanosis occur;
- how the bluish tint changes during the day or under the influence of some factors;
- cyanosis appears constantly or periodically.
After this, the specialist listens to the lungs and heart. To obtain more detailed data, the following types of laboratory and instrumental diagnostics may be prescribed:
- blood gas analysis;
- clinical blood test;
- pulse oximetry;
- spirography;
- chest x-ray;
- CT scan of the chest.
After diagnosis, the patient may be recommended other types of examinations to create a more effective treatment plan for the underlying disease.
Treatment
The main goal of treatment when cyanosis is detected is aimed at eliminating the underlying disease. And to eliminate oxygen starvation, the patient may be prescribed oxygen therapy and certain medications.
Oxygen therapy
 A person with acute cyanosis is indicated for oxygen therapy, possibly in a pressure chamber
A person with acute cyanosis is indicated for oxygen therapy, possibly in a pressure chamber Additional supply of oxygen to the patient’s body allows the blood to be saturated with oxygen and reduces the bluishness of the skin. However, this method of treatment is effective only for acute cyanosis. In the chronic presence of cyanosis (for example, with heart disease or anemia), eliminating tissue hypoxia in this way will be a temporary measure, and to treat the underlying disease, the patient must undergo a course of conservative or surgical treatment.
Oxygen therapy can be carried out using:
- oxygen mask (simple, non-reversible or Venturi);
- nasal catheters;
- oxygen tent;
- artificial lung ventilation device;
- barotherapy.
The method of supplying the oxygen mixture to the body is determined individually and depends on the clinical case. Oxygen therapy can be carried out both in a hospital setting and at home (using portable oxygen cylinders or concentrators).
Drug therapy
To eliminate cyanosis and oxygen starvation of tissues, patients may be prescribed medications that normalize blood flow, enhance erythropoiesis, the activity of the heart and lungs, or improve blood flow. The goal of such drug therapy is to improve the supply of oxygen and its delivery to tissues suffering from hypoxia.
To reduce the manifestations of cyanosis, the following may be prescribed:
- respiratory analeptics - Cititon, Etimizol, etc.;
- bronchodilators - Berodual, Salmbutamol, etc.;
- – Korglykon, Strophanthin;
- neuroprotectors – Piracetam, Nootropil, Phezam, etc.;
- – Fragmin, Warfarin, etc.;
- vitamin preparations.
If cyanosis is caused by a chronic disease, then after treatment the patient is recommended to undergo clinical observation. Such constant monitoring of the course of the disease allows timely adjustment of therapy and prevent the development of more severe cases of tissue hypoxia.
Cyanosis of the skin and mucous membranes is a symptom of many diseases, but is more often detected in pathologies of the respiratory organs, heart or blood vessels. Its appearance should always be a reason to consult a doctor. To eliminate the causes of its occurrence, the patient should undergo a comprehensive diagnosis, the data of which will allow the doctor to draw up the most productive treatment plan. In some cases, with the sudden appearance and rapid increase of cyanosis, cyanosis indicates the development of a critical condition and requires emergency assistance and calling an ambulance.
Main symptoms:
- Blue discoloration of the nasolabial triangle
- Blue soles
- Blue ears
- Blue discoloration of the phalanges of the fingers
- Blueness of the skin
- Bluishness of the extremities
- Blueness of nails
- Blueness of mucous membranes
Cyanosis of the skin and mucous membranes is the appearance of an unnatural bluish tint in certain areas of the body and mucous membranes, which can occur in both a child and an adult. According to medical research, this pathological condition is caused by the fact that there is an increased amount of abnormal hemoglobin in the blood, which makes its color similar to blue. In this case, there is insufficient oxygen saturation of the blood, as a result of which blood is not supplied to certain areas of the body in the required volume, which causes cyanosis of the skin and mucous membranes.
In some cases, this pathological condition is extremely severe, as it is accompanied by suffocation. And if a patient in such a condition is not provided with timely medical care, there is a high risk of death.
Varieties and reasons
The most common phenomenon is acrocyanosis, characterized by a change in the color of the skin on the distal parts of the body, that is, the limbs and face. Acrocyanosis predominantly develops in patients with cardiac pathology and may be evidence of development in a child or adult. In adults, acrocyanosis is also a sign of the development of some other pathologies. But the pathology also occurs in infants who do not have anomalies in the development of the cardiovascular system.
With this type of pathology, cyanosis is localized on the hands and feet, ears, tip of the nose and lips. For a baby in the first days of life, acrocyanosis is a normal phenomenon, since his lungs have not yet begun to function fully, which is manifested by an insufficient supply of oxygen to the blood. Acrocyanosis is more pronounced when the baby cries, makes excessive efforts during feeding, or is restless.
It is important to understand that there are different varieties of this pathological condition. So, in medical practice they talk about central and local cyanosis. Central cyanosis develops in cases where arterial blood is not sufficiently saturated with oxygen, which happens in severe diseases such as erythrocytosis, and others. This condition may indicate the need for urgent medical care for a person. This type is also called diffuse cyanosis, and it has the maximum severity.

With local cyanosis, impaired blood circulation is observed in a localized area due to local disruption of blood circulation. This form of pathology is observed in places of increased accumulation of blood vessels - around the mouth, around the eyes.
The local form is also called peripheral cyanosis. The causes of this form of the disease can be the following pathological conditions:
- slowing down of blood flow in the capillaries due to their compression by a tumor;
- poisoning of the body;
- heart and vascular diseases;
- and, preventing sufficient oxygen from entering the blood;
- chest deformation as a result of traumatic injury with impaired respiratory function.
Cyanosis of the nasolabial triangle is often diagnosed in infants, which indicates malformations of the lungs, heart and neuralgia.
In general, peripheral cyanosis occurs in medical practice more often than central cyanosis, since there are many more reasons that cause it.
Symptoms
If a patient has a form of pathology such as acrocyanosis, which is mainly found in infants, its symptoms will consist of blue discoloration of the nails, phalanges of the child’s fingers and soles, ears and nasolabial triangle, including mucous membranes. Blueness of the mucous membranes, nails and skin can be mild or severe - and the more pronounced it is, the more severe the child’s condition, which indicates acute respiratory failure.
Very often, cyanosis of the nasolabial triangle, as well as peripheral cyanosis, occurs in people with such pathological conditions as:
- convulsions;
- drug overdose;
- food poisoning.
Symptoms of the pathological condition, manifested by blueness of the skin, nails and mucous membranes, differ depending on the type of disorder that caused acrocyanosis. Thus, in diseases of the lungs or bronchi, cyanosis of the lips, nasolabial triangle and mucous membranes is manifested by the dark purple color of this area, indicating a lack of oxygen.
In heart disease, acrocyanosis also occurs, but the clinical picture is complemented by other symptoms, such as:
- thickening of the phalanges of the fingers like drumsticks;
- wet rales;
- hemoptysis;
- dyspnea.
Cyanosis of the extremities occurs in the peripheral form of the pathology, and is diagnosed quite often in both adults and children. At the same time, cyanosis in newborns, as mentioned above, can be both pathological and physiological in nature, so medical care is required for infants only when the cyanosis is severe and does not go away for a long time.
Diagnostics
Acrocyanosis and other varieties of this pathological condition are not a disease in themselves. This is just a symptom of a serious pathology in the body of a child or adult, so when such a symptom appears, diagnosis is important. First of all, if a child or adult has facial cyanosis, their respiratory system is checked, identifying the causes of the lack of oxygen in the blood. If a child is diagnosed with acrocyanosis, that is, blue discoloration of the limbs, mucous membranes, and nails, disorders in the functioning of the cardiovascular system are diagnosed first.
The main tests that are prescribed for patients with suspected acrocyanosis are:
- general blood test;
- blood gas analysis;
- blood flow velocity analysis;
- pulse oximetry.

Then, taking into account complaints and symptoms, as well as test data, research methods such as electrocardiography, chest CT, or chest x-ray may be prescribed.
Features of treatment
Acrocyanosis, as mentioned above, is a symptom of a pathological condition of internal organs. Therefore, treatment in this case will be aimed at eliminating the underlying disease that caused the bluishness of the face, limbs, mucous membranes or nails.
One of the methods that is used to treat this pathological condition is oxygen therapy, in which the patient is given oxygen to inhale, thereby increasing its concentration in the blood. Treatment with oxygen therapy is used in conjunction with other measures to treat cardiac or respiratory failure that causes acrocyanosis.
Drug treatment is also used - drugs are prescribed that improve blood flow and increase the saturation of capillaries. Such drugs include:
- antihypoxants;
- bronchodilators;
- respiratory analeptics;
- cardiac glycosides and some other medications used as prescribed by a doctor.
Unfortunately, in most cases, treatment will be ineffective if acrocyanosis in a child or adult develops as a result of cardiac pathologies. In such situations, only surgical treatment is effective, especially often used in infants born with heart abnormalities.
Is everything in the article correct from a medical point of view?
Answer only if you have proven medical knowledge