Health financing system
and health insurance
LECTURE No. 1 - (2 hours)
MAIN SOURCES OF FINANCING OF HEALTHCARE OF THE RUSSIAN FEDERATION.
DEFICIENCY OF FINANCIAL FUNDS AND THE PROGRAM OF STATE GUARANTEES OF PROVIDING FREE MEDICAL CARE TO THE POPULATION.
GLOBAL BUDGET FINANCING METHOD
In the period of transition to a market economy, the search for effective mechanisms to improve the performance of the public health service led to the replacement of centralized budgetary financing of medical institutions with payment for the work actually performed under the contract and the formation of a competitive environment.
The characteristics of health financing systems can be given from the point of view of the source of the formation of funds and from the point of view of the interaction of medical organizations with each other.
According to the source of funding, one can distinguish budgetary, insurance and private systems. However, there is never a purely insurance, budgetary or private financing system. We can talk about the predominant, dominant source of funding. If this is the compulsory medical insurance system, then employers' contributions prevail, if the budget system is dominated by general taxes (profit tax, value added tax, etc.).
By the nature of the interaction of healthcare subjects, an integration, contractual model of the financing system is distinguished, as well as the model of compensation and the model of "managed care". This classification uses the experience of health care financing not only in Russia, but also in foreign countries (see Table 3).
Health financing models
|
By source of funding |
By the nature of the interaction |
||
|
Model financing |
Main features |
Model financing |
Main features |
|
Budgetary |
Based on the collection of taxes, from which the revenue side of the budget is formed, and then the expenditure on health care is determined |
Integration |
1. Merging the functions of financing, management and organization of health care. 2. Healthcare management - the funding party. 3. The manufacturer and provider of services is a state health care institution with a district affiliation. 4. Opportunities to choose a doctor among the population are limited 5. State-owned management system. |
|
Insurance |
Based primarily on earmarked health insurance premium. Often comes in the form of a combination of insurance and budget financing |
||
|
Private |
It is mainly based on contributions from personal funds of citizens, charitable foundations, etc. |
Contractual |
1. Contractual relationship. 2. Principle "Money follows the patient". 3. Economic levers of control. 4. High costs of contractual and administrative relationships. 5. Economic independence of medical service providers (Germany, France). In Russia - relative independence (as a legal entity). |
|
Model reimbursement |
one . Patients pay for services from their own funds, and then reimburse the bulk of the amounts spent from the CHI fund. 2. Prices are free. 3. The number of medical facilities is not limited. There are no contracts. 4. Disadvantage - the product of costly trends in healthcare. |
||
|
The "managed care" model |
one . Funded by the general soul standard. 2. Based on a special form of contracts between the financing party and the manufacturers (providers) of medical services; the insurer is involved in health care planning (USA). 3. It is a medical insurance association with common management structures and internal commercial accounting. Acts like a corporation. 4. Economic independence of health care facilities. 5. General rules of management and administration have been determined. |
||
The sources of financing in the health care system are:
Funds of budgets of all levels;
Compulsory medical insurance funds;
Funds from trust funds intended for the protection of public health;
Income from entrepreneurial activities of healthcare organizations, in particular from the provision of paid medical services.
In general, the healthcare financing system in Russia (by funding sources) is characterized as a budgetary and insurance model.
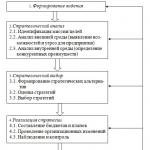
In more detail, the sources of funding for healthcare in the Russian Federation are shown in Scheme 2.
As noted, there are several financial flows directed to the health sector.
Budgetary sources: federal budget; the budget of the constituent entity of the Russian Federation; local budget; non-budgetary reallocation resources. To the lastincludes compulsory health insurance funds.
Medical and prophylactic institutions of any form of ownership, licensed and accredited in the prescribed manner, are financed on the basis of contracts with medical insurance organizations, with the territorial CHI fund, its branches performing the functions of an insurer.
The main source of financing for health care is the state budget, formed from the collection of general taxes from business entities and from the population. Revenues from enterprises are made from income taxes, turnover tax, social insurance contributions, etc. Income from the population is carried out by paying income tax, placing an internal loan and income from cash lotteries.
From the revenues received, the state, represented by the Russian Ministry of Finance, allocates certain funds for the maintenance and development of healthcare. The level of funding is determined through negotiations between the Ministry of Finance and the Ministry of Health and is based on previous experience, modern development requirements and the capabilities of the state. The agreed budget is approved by the Government of the Russian Federation and approved by the supreme body of power - the Federal Assembly. From the moment of approval, the state budget becomes law and is binding.
Credit managers (budget executors) are ministers and heads of local authorities (first degree), heads of organizations and institutions subordinate to ministries (second degree), heads of other organizations and institutions (third degree). Thus, the administration of health care institutions is the administrator of third-degree loans.
Health care institutions are financed from the budgets according to their subordination: republican subordination - at the expense of the republican budget; regional subordination - at the expense of the regional budget; urban - at the expense of the city; local - from local budgets. At the same time, additional financing of health care institutions "from top to bottom" is possible, that is, at the expense of the budgets of higher management bodies.
The main source of financing for healthcare in Russia is still the budget of all levels (federal, regional, local). In 1996, the budget accounted for 62.4% of all financial resources for health care. For these purposes, 8.4% of all expenditures of the country's consolidated budget went. In the federal budget, the share of expenditures on health care was only 1.3%, and in the consolidated budgets of the constituent entities of the Russian Federation - 15.3%. At the same time, significant differences were noted between the subjects of the Russian Federation: if in the Belgorod, Orenburg and a number of other regions this share was over 21%, then in the Voronezh and Kursk Kemerovo regions - 13-14%. The share of the federal budget in total health care expenditures was only 6.0% (in 2001 - 12%). As a result, the population of the regions, which for objective reasons cannot provide an acceptable level of funding for health care, is in a very difficult situation and cannot receive free medical care of a guaranteed volume and quality.
One of the sources of financing for health care is the personal funds of the consumer of health services. The paid sector has existed for almost the entire history of Russia. Every citizen had the right to go to a private practicing doctor or to special, so-called "self-supporting" polyclinics, where for a fee he could receive the necessary advisory or medical outpatient care. The existing opinion that the system of paid medical care arose only in the course of the reform does not correspond to reality. In the course of the reform, new forms of providing paid medical care were developed:
cooperatives, contracts with enterprises for the provision of additional services to their employees. Moreover, the latter became widespread almost throughout the country, and not only in Leningrad, Kemerovo and Samara - the first experimental territories.
The channel for financing health care through the private health care market is becoming increasingly important. Unfortunately, it is difficult to estimate its volume. Data on the volume of paid services rendered to the population by health care institutions (Table 46) indicate that the funds spent by the population on the purchase of paid services are estimated at the level of 1.5% of health care expenditures from all sources.
Table 46
Dynamics of the volume of paid services,
provided by health care institutions to the population,
RUB bln at actual prices
|
Payments |
1985 |
1990 |
1992y |
1993y |
1994 |
1995 year |
1996 |
1997y |
1998 |
|
Voluntary health insurance contributions |
N. d. |
N. d. |
N. d. |
1182 |
2237 |
3386 |
3,80 |
||
|
Paid medical services |
0,13 |
0,41 |
5,41 |
2939 |
5601 |
9329 |
11,40 |
||
|
Total |
0,13 |
0,41 |
5,41 |
1038 |
4121 |
7838 |
12715 |
15,20 |
|
|
Per resident, RUB |
2086 |
However, this estimate is clearly underestimated. Indirect estimates, carried out by calculating the share of the "shadow economy" through the share of "shadow services", makes this indicator to be increased by an order of magnitude. Thus, the real volume of the market for private medical services is estimated by experts at about 15-30% of the total expenditures on health care (Table 47).
It should be borne in mind that different stages of medical technology require different funding structures. Elements of health care provision such as food preparation, laundry, cleaning of premises, and certain types of care, including nursing care, can be highly privatized. At the same time, there are types of medical services where it is desirable to reduce the share of the private sector to zero.
This issue is highly controversial. In preparing the package of laws on private medical practice, two opposing points of view were expressed. According to the first, the private sector should generally not be allowed into the provision of medical care for particularly dangerous infections. Supporters of the second point of view believe that the private sector can operate in any area of medical care, while its activities are regulated through a permitting (licensing) system.
Unfortunately, the issue of legal regulation of private medical activity has not been properly resolved today, so the bulk of the private sector of the medical market is in the "shadow economy".
Finding a solution to the problem of the financial deficitshould focus on:
Reduction of funding for the sectors of secondary and tertiary health care and support of primary health care at the expense of the program of state guarantees;
Transfer of expensive medical technologies to a paid basis;
A clear definition of the minimum volume of free
services, and for additional medical services the introduction of patient co-payments;
The possibility of forming a system of compulsory health insurance at several levels: the basic compulsory health insurance system and additional programs with a higher contribution rate for compulsory health insurance;
Legalization of co-payments of the population.
Along with the organization of compulsory medical insurance, the law on health insurance provides for the introduction of a voluntary health insurance system (VHI). The main distinguishing feature of the VHI is that the payment of the costs of medical services is mainly borne by the patient himself. In addition, if CHI is carried out within the framework of the approved Basic Program of CHI, then with VHI, the provided medical services go beyond the framework of the Basic Program.
VHI is developing as an addition to the CHI programs, providing additional services of a higher level, which ultimately expands the financial capabilities of health care in general.
The growth in the cost of providing medical care in conditions of shortage; resources forces to take measures simultaneously along two oppositely directed paths.
First, it is necessary to increase the share of spending on health care in the structure of GDP by increasing the share of expenditures from budgets of all levels (this can be done either by improving tax collection, or by reducing other types of budget expenditures, or by using both solutions. simultaneously), as well as by increasing the size; insurance payment for compulsory medical insurance (earlier calculations of the Ministry of Health inFFOMS show the need to double the current tariff).
Secondly, it is necessary to develop control over health care costs by regulating the supply and demand for medical services.
Demand management can be done by;
Introduction of a procedure for co-payment by citizens of medical care (or some of its types);
Establishing priorities for regulating the availability of certain types of health care;
Using the return of a part of insurance premiums for compulsory medical insurance to citizens who have not been ill for a year in the form of premiums;
Reducing the amount of income tax for citizens who used their personal funds to receive medical care.
The last two proposals are apparently unrealistic for their application in modern Russian healthcare.
The introduction of co-payment by patients of received medical care is aimed, first of all, at obtaining additional Income for the health care system. There are many arguments in favor of the fact that the use of co-payment mechanisms does not reduce health care costs, but transfers them from the obligations of public funds to the personal costs of sick citizens. At the same time, their use to some extent reduces the turnover of the population to doctors by "cutting off" cases that do not have a medical basis and are mainly "social" appeals.
If a decision is made to introduce co-payment by making appropriate amendments to the draft law "On Health Care of the Russian Federation", it will be necessary to provide for:
1) co-payment conditions (for example, each case of referral to an outpatient clinic, each hospital bed-day, for each prescription drug on a preferential basis for outpatient treatment);
2) the amount of co-payment (for each visit, for each day of stay in the hospital, but not more than a certain amount for each case of treatment, for each prescription or for each name of the "preferential" medicine);
3) the possibility of exclusion for certain groups of patients (for example, for patients with diabetes or tuberculosis - exclusion of co-payment for the purchase of insulin and anti-tuberculosis drugs, respectively);
4) strict control over medical personnel to prevent cases of extortion of funds from patients;
5) the need for accurate calculations for each specific type andthe capacity of the institution in terms of the amount of administrative costs associated with the introduction of the co-payment procedure so that additional administrative costs (purchase of a cash register, remuneration of administrative personnel, payment of the necessary forms and forms of accounting and reporting, etc.) do not exceed the income additionally received from co-payment ...
Patient cost sharingfor medical services is associated with specific policy mechanisms that operate in the area of demand in the market for medical services. These mechanisms usually operate within the insurance system and define the following main forms of patient participation in cost coverage.
Complicity in payment for services: a lump sum that the consumer must pay for each service provided, for each prescribed medication.
Coinsurance: A percentage of the total cost of a service that must be paid by the consumer (for example, the patient pays 20% of the total cost of inpatient care).
The need for the participation of the population in paying for medical care is due to the following underlying reasons. The amount of resources that the state can allocate for the development of the social sector, including health care, is directly related to budgetary constraints, especially in a transitional economy. On the one hand, the immaturity of market structures makes it impossible to launch market mechanisms. Our population is accustomed to the system of universal guarantees. At the same time, health care itself objectively cannot develop exclusively on a market basis. On the other hand, a transitional economy requires a decrease in government costs and an increase in the responsibility of citizens. per self-sufficiency, for social development (in conditions of budget deficit and other unfavorable economic realities). All this leads to the wide involvement of extra-budgetary funds in the development of the industry.Strategic directionsof the modern program of state guarantees for the provision of free medical care to citizens of the Russian Federation are:
Reduction in the volume of inpatient care (by about 20%);
Development of hospital-substituting types of care;
Increasing the cost of outpatient care, strengthening its therapeutic function.
The problem of the availability of medical care and, at the same time, a reduction in the volume of inpatient care can be solved mainly at the expense of large cities, where there is a developed network of medical institutions and adjustments to their capacity. However, one cannot go by the way of closing small district hospitals, as this will immediately reduce the level of accessibility of medical care for remote areas, which would be wrong.
The reform process in health financing continues, with the following changes planned for the next decade.
√ The state must ensure the constitutional rights of citizens to receive free medical care by allocating funds for health care from budgets of all levels and compulsory health insurance funds necessary to finance the program of state guarantees. Also, the state undertakes to ensure the priority of health care development by allocating funds in the amount of at least 6% of the gross domestic product.
√ In the federal budget for health care should be allocated funds in the amount of at least 5% of its expenditure side. In the budgets of the constituent entities of the Russian Federation, it is planned to allocate funds for health care in the amount of at least 20% of their expenditure side. When funds are received from extra-budgetary sources, it is prohibited to reduce the amount of budget funds allocated for health care.
Financial standards to compensate for the cost of providing free medical care per person per year (per capita standards) are used for:
Planning the volume of medical care to citizens;
calculations of payments for compulsory health insurance of unemployed citizens;
distribution of financial resources when leveling the conditions for the provision of medical care on the territory of the Russian Federation;
Settlements with manufacturers of medical services for the provision of medical care in the compulsory health insurance system
The procedure for determining the per capita standards for compulsory medical insurance of unemployed citizens is approved by the Federal Compulsory Medical Insurance Fund in agreement with other federal executive bodies in the field of health care.
√ The budgets of all levels allocated for health care should provide for the share of funds allocated for the purposes of health education of the population and the prevention of diseases.
The amount of budgetary financing in the field of health care is set depending on the tasks performed within the framework of state programs. If healthcare organizations, the source of funding for which is the federal budget, are directly involved in the implementation of regional target programs in the field of healthcare, then such activities are provided at the expense of the budgets of the constituent entities of the Russian Federation and extra-budgetary funds.
Extremely insufficient budget financing of medical institutions, the inability of territorial compulsory medical insurance funds to compensate for the budget deficit requires the commercialization of the healthcare sector, and therefore the creation of medical organizations on the basis of various forms of ownership, including joint-stock, cooperative, etc. This leads to the fact that today healthcare is represented not only by budgetary institutions of federal and local subordination, but also by commercial structures. The patient acts as a customer in the medical services market and gets the opportunity to choose a more attractive medical institution. This stimulates the drive to improve the quality of health care.
In a market economy, it is possible to distinguish budgetary, insurance and private (by source) health care financing systems.
The amount of budgetary financing in the field of health care is set depending on the tasks performed within the framework of state programs. If a healthcare organization, a source of fundingwhich is the federal budget, are directly involved in the implementation of regional target programs in the field of health care, such activities are provided at the expense of the budgets of the constituent entities of the Russian Federation and extra-budgetary funds (Table 4).
The centralized budget of health care significantly narrows the possibilities of operational management, minimizing the influence of the factors of the current situation on the management of resources, which inevitably reduces the overall economic efficiency of budgetary health care. With the constant budget cuts, centralized funding becomes a tool for the self-destruction of the health care system.
Table 3. Types of health financing systems


According to the general WHO recommendation, the state should allocate at least 6-7% of the gross domestic product (GDP) to healthcare as an industry that ensures the national security of the country. Unfortunately, Russia lags behind this indicator (Table 5), while the size of the population's expenditures on drug provision and medical care (4.5% of GDP in 1998) exceeds the volume of state funding for health care (3.1%). The total volume of government and population spending on healthcare in our country is 7.6% of GDP. This is significantly higher than in the 1990s (from 3.3 to 4.5% of GDP).
Table 5. Total expenditures on health care in Western Europe,% of GDP
|
The country |
1995 year |
1996 year |
1997 year |
1998 year |
1999 year |
2000 |
|
Austria |
||||||
|
Belgium |
||||||
|
Denmark |
||||||
|
Finland |
||||||
|
France |
||||||
|
FRG |
10,6 |
10,9 |
10,7 |
10,6 |
10,7 |
10,6 |
|
Greece |
||||||
|
Iceland |
||||||
|
Ireland |
||||||
|
Italy |
||||||
|
Canada |
||||||
|
Luxembourg |
||||||
|
Netherlands |
||||||
|
Norway |
||||||
|
Portugal |
||||||
|
Spain |
||||||
|
Sweden |
||||||
|
Switzerland |
10,0 |
10,4 |
10,4 |
10,6 |
10,7 |
10,7 |
|
Great Britain |
||||||
|
USA |
13,3 |
13,2 |
13,0 |
12,9 |
13,0 |
13,0 |
The compulsory medical insurance system, being an integral part of health care, radically changed the situation, as it made it possible to transfer health care to multi-channel financing.
In a market economy, extra-budgetary sources of financing for the health care system of the Russian Federation can be funds:
1) compulsory medical insurance and voluntary medical insurance;
2) organizations that have concluded contracts with healthcare organizations for the provision of medical services;
3) investors financing innovative projects carried out on the initiative and (or) on the basis of healthcare organizations, grants and inventions in the field of new medical technologies;
4) educational medical and pharmaceutical institutions using healthcare organizations as a clinical base;
5) from the rent for the use of property assigned to healthcare organizations on the basis of operational management;
6) from activities related to training medical technologies for medical workers, as well as activities on health education of the population on the basis of contracts with customers;
7) enterprises and other organizations on claims brought against them for reimbursement of expenses for the treatment of citizens in connection with occupational diseases and accidents at work, road traffic accidents, poisoning and infectious diseases associated with violation of the sanitary-epidemic regime;
8) humanitarian activities - in the form of grants (gratuitous subsidies) or other assistance (support);
9) from other receipts not prohibited by the legislation of the Russian Federation;
10) from patients for providing them with paid medical services.
A transitional economy in conditions of budget deficit and other unfavorable economic realities requires a reduction in government spending and the wide involvement of extra-budgetary funds in the development of the industry, including the complicity of patients in the cost of medical services.
The variety of forms of ownership, entrepreneurship and competition is a precondition for the formation of a market system that creates new potential for meeting social needs. This potential includes:
Increasing the opportunities for citizens to receive income and provide themselves and family members with social services;
The emergence of new sources of satisfaction of needs through the development of private entrepreneurship.
Over the years, Russian healthcare has taken a sharp turn from an overly centralized to a fragmented system.
The health care system was fragmented. On the one hand, there is a tendency to divide the unified public health system according to the principle of the main sources of funding - through the compulsory medical insurance system, state and municipal budgets. The unified public health system was divided into 2 sectors - budgetary and insurance. One and the same health care institution operates on the basis of completely different financing and management schemes within the budgetary and insurance systems. Each of them is built on the basis of its own rules, which has an extremely negative impact on the health care economy and prevents the implementation of a unified approach to management and planning.
The current legislation on the foundations of local self-government enshrines the autonomy of local authorities in addressing health issues. As a result, each municipality builds its own closed system.
To some extent, the fragmentation of the system is compensated by the efforts of the territorial CHI funds, which are trying to build a single funding system for the subject of the Federation. The current legislation on health insurance provides an opportunity to centralize financial resources to level the playing field for health care financing. Nevertheless, the possibilities of the CHI system are very limited. Today, only 30-35% of all health care resources pass through its structures. This is not enough to ensure reasonable centralization and a unified management strategy.
There is a tendency towards weakening of the interaction between the individual levels of health care delivery and health services. Due to the low level of planning, one district is forced to maintain unnecessary capacities, while in the neighboring territory there is an acute shortage of them. There are many examples of the idle time of expensive equipment purchased by small district hospitals (usually due to a lack of qualified personnel). As a result, the existing network of medical institutions is less and less consistent with the real needs of the population and the requirements for rational use of resources.
In addition, the most important principle of the organization of the system - the staging of the provision of medical care - was under threat. The health care system cannot be built in one separate area; to increase the efficiency of resource use, a reasonable regionalization of the network of medical institutions is required, based on the division of their functions, taking into account the level and type of each institution.
This implies a higher level of centralization of management and financing than prevailing today. This is the fundamental difference between health care and other systems of the social sphere, which have been managed by the municipal authorities.
The public nature of health care financing
High priority of health care among nationalgoals and the trend of the 70s. XX v. to the "socialization" of health care led to the fact that in the early 80s. health care was funded by more than 3/4 from public funds. At the same time, in most countries, almost the entire population received access to outpatient and hospital care at the expense of public funds. In the United States alone, public health funding does not exceed 50%.
Public funds are understood as funds of the state, national compulsory insurance programs, local authorities (district, district, municipal, etc.), public organizations (trade unions, churches, parties, etc.).
In subsequent years, when the demand for resources began to exceed the capacity of the state, the share of public spending in total spending on health care decreased slightly in most economically developed countries (see Table 36). Moreover, in Great Britain, Ireland, Italy, Greece and France by more than 5 points, and in Portugal - by 10 points in 1990 compared with 1980. Only in Australia, Finland, Japan and Turkey did the share of public spending increase slightly.
The idea is quite widespread that in the event of a shortage of public funds, funds from patients and other private sources should be actively mobilized. This idea is supported incl.The World Bank.
At the same time, the introduction of payment for doctors' visits even at the level of 1.5-2 Canadian dollars. dollars led to a decrease in aid in Canada in the 70s. by 7%, and for the poor this decline was even 12%, which meant a relative increase in access to health care for the rich. A similar picture was observed in France in the early 1980s. The introduction of a co-payment for outpatient care in the United States in the 70s. within the program " Medicaid "led to an 8% reduction in outpatient care while a 17% increase in hospital care.
Available data indicate that in many countries the government and / or national insurance system reimburses the bulk of health care costs.
In recent years, interest in the dynamics of health care costs has been growing. However, the reasons for this vary from country to country. If in developing countries and countries with economies in transition, such as Russia, this interest is associated with maintaining the health care system, despite the budget deficit, and, at least, preventing a decrease in health care costs, then in economically developed countries are interested in the need to contain costs, improve the efficiency of resource use.
For the latter group of countries, it is characteristic that the growth in health care costs is associated to a greater extent with the growth in the cost of medical services and, to a lesser extent, with the actual growth in the volume of care provided.
SYSTEM OF STATE GUARANTEES TO PROVIDE CITIZENS OF THE RUSSIAN FEDERATION WITH FREE MEDICAL CARE
The transition to a compulsory health insurance system has marked the emergence of fundamentally new economic relationships in the health care system. As a result, the industry has moved from funding on a “content” basis to “earning money” for health care provided.
At the same time, there is an imbalance in the industry between the obligations of the state to provide free medical care to citizens and the financial resources allocated for this. The inconsistency of the furnishing in the “money-commodity” system does not allow to fully realize the economic potential of the idea of health insurance.
To solve this problem, the program of state guarantees for the provision of citizens of the Russian Federation with free medical care was developed, which determines the minimum necessary volumes of medical care and financial resources for their provision not only in the compulsory medical insurance system, but in the entire health care system.
The formation of a system of state guarantees of the Russian Federation in terms of the provision of free medical care provides for the strengthening of the budgetary and insurance form of financing health care by clearly dividing the types and volumes of free medical care according to adequate funding sources.
In order to implement the constitutional rights of citizens of the Russian Federation, by the Decree of the Government of the Russian Federation since 1998. the Program of state guarantees for the provision of free medical care to citizens of the Russian Federation (hereinafter referred to as the Program) is approved annually.
The objectives of the development of the Program are:
Creation of a single mechanism for the implementation of the constitutional rights of citizens to receive free medical care of a guaranteed volume and quality throughout the country;
Creation of a unified system of planning and financing of medical care;
Ensuring compliance with the obligations of the state to provide the population with free medical care and the funds allocated for this;
Improving the efficiency of the use of health care resources. The basic principles of building the Program include the following provisions:
Determination of the required volumes of medical care in accordance with the level of morbidity of the population;
Per capita calculation of the probability of an insured event (illness and (or) seeking medical help);
Determination of socially necessary costs for the implementation of the corresponding unit of the volume of medical care;
Compliance of the guaranteed volumes of free medical care to citizens and the financial resources necessary for their implementation according to their sources;
Establishment of obligations of executive authorities of all levels for the implementation of this Program;
Introduction of a unified system for planning health care expenditures at the expense of budgets of all levels and compulsory health insurance funds.
The program provides for the priority development of the outpatient and polyclinic sector and increasing the efficiency of inpatient care through its intensification.
The program consists of 6 sections and includes a list of types of medical care provided to the population free of charge, the basic program of compulsory medical insurance, the volume of medical care, the procedure for the formation of per capita health financing standards that ensure the provision of guaranteed volumes of medical care.
The section "General Provisions" formulates the principles and identifies the sources of funding for the Program. In particular, the section indicates that it was developed on the basis of the standards for the volume of medical care, which are the basis for the formation of health care costs in the budgets of all levels and in the corresponding budgets of compulsory health insurance funds.
The section "List of types of medical care" contains the types of medical care included in the Program:
Ambulance for conditions that threaten the life or health of a citizen or those around him, caused by sudden illnesses, exacerbations of chronic diseases, accidents, injuries and poisoning, complications during pregnancy and childbirth;
Outpatient medical care, including the implementation of measures for the prevention (including dispensary observation), diagnosis and treatment of diseases both in the clinic and at home;
Inpatient care for acute diseases and exacerbations of chronic diseases, poisoning and injuries requiring intensive care, round-the-clock medical supervision and isolation for epidemiological indications, with pathology of pregnancy, childbirth and abortion, with planned hospitalization for the purpose of treatment and rehabilitation, requiring round-the-clock medical supervision.
In the provision of emergency medical and inpatient care, free drug assistance is provided. The conditions and procedure for the provision of medical care to the population are determined by the Ministry of Health of Russia in agreement with the Federal Compulsory Medical Insurance Fund.
Citizens of the Russian Federation are provided with the followingconditions for the provision of medical care.
1. In outpatient clinics:
Possibility of a patient's choice of a doctor and a medical institution within the framework of contracts for the provision of medical and preventive care in the system of compulsory medical insurance;
The scope of diagnostic and therapeutic measures for a particular patient is determined by the attending physician;
The possibility of having a queue of patients for an appointment with a doctor and carrying out diagnostic tests, medical procedures. The maximum waiting times are determined by the territorial Programs;
For emergency indications, medical care in the clinic is provided from the moment the patient applies;
Routine referral of the patient to hospitalization is carried out by the medical institution or health authority in accordance with clinical indications.
2. In stationary institutions:
Hospitalization of patients is carried out according to clinical indications requiring intensive diagnostic and treatment methods, as well as round-the-clock observation;
In case of emergency, the patient is hospitalized out of turn;
The possibility of having a queue for planned hospitalization. The maximum waiting times are determined by the territorial Programs.
Patients are accommodated in wards for 4 or more beds;
Examination and treatment for the patient is provided according to the doctor's prescription;
While in the hospital, the patient receives free examination, treatment, medical nutrition in accordance with the standards of medical care;
Providing the opportunity for one of the parents or another family member, at the discretion of the parents, to stay with a sick child up to 1 year old.
The section "Basic program of compulsory health insurance" defines the types of diseases for which outpatient and inpatient care is provided at the expense of compulsory health insurance.
The basic program is implemented on the basis of contracts concluded between participants (subjects) of medical insurance - a citizen of the Russian Federation, a medical insurance organization, a territorial compulsory medical insurance fund, a medical organization.
Medical assistance within the framework of the basic compulsory health insurance program is provided to citizens throughout the Russian Federation in accordance with compulsory health insurance contracts.
The section "Medical care provided to the population at the expense of budgets of all levels" lists the types of medical care provided to citizens free of charge at the expense of budgets of all levels.
At the expense of the federal budget, citizens are provided free of charge medical care provided in health care institutions of federal subordination, including high-tech (expensive) medical care, the list of which is approved by the Ministry of Health of Russia.
At the expense of the budgets of the constituent entities of the Russian Federation and municipalities, citizens are provided with emergency medical care, provided by stations (departments, points) of emergency medical care. From the same sources, the provision of outpatient and inpatient care is provided, provided in specialized dispensaries, hospitals (departments, offices) for sexually transmitted diseases, tuberculosis, acquired immunodeficiency syndrome, mental disorders and behavioral disorders, drug addiction diseases, with congenital anomalies ( malformations), deformities and chromosomal abnormalities in children, certain conditions arising in the perinatal period, expensive types of medical care, the list of which is approved by the healthcare management body of the constituent entity of the Russian Federation.
At the expense of budgets of all levels, preferential provision of drugs and prosthetics (dental, eye, ear) is carried out, as well as financing of medical care provided by feldsher-obstetric points, hospices, nursing hospitals, leper colony, trachomatous dispensaries, centers for combating acquired immunodeficiency syndrome , centers for medical prevention, medical and physical dispensaries, departments and centers of occupational pathology, children's sanatoriums, children's homes, bureaus of forensic medical examination and pathological examination, centers of emergency medical care, stations, departments, offices of blood transfusion, air ambulance.
The section "Volumes of medical care" defines the standards for the volume of medical and preventive care per 1000 people.
The basic standards for the volume of medical care were approved in order to achieve compliance with state guarantees for providing the population with free medical care and financial resources (budget funds of all levels and insurance premiums) allocated for their implementation, increasing the efficiency of using financial resources by improving the structure of medical care.
The indicator of the volume of outpatient care is expressed in the number of visits per 1000 people and the number of days of treatment in day hospitals, day hospitals and hospitals at home per 1000 people.
For example, consider the standards for the volume of medical care approved for 2002.
The number of visits is 9198, including 8458 visits for the basic program.
The standard for the number of days of treatment in day hospitals, day care hospitals and home hospitals is 749 days, including 619 days for the basic program.
The indicator of the volume of inpatient care is expressed in the number of bed-days per 1000 people.
This indicator is calculated by multiplying the hospitalization rate by 1000 people. on the average duration of the patient's stay in the hospital.
In 2001, this indicator averaged 3330 in Russia, which is several times higher than foreign indicators (1000-800). Analysis of the current volume (3330 bed-days per 1000 people) shows that there are often patients in the hospital who can be treated on an outpatient basis with the same quality. In addition, patients are treated in a hospital until complete recovery, which is extremely irrational. With planned hospitalization, almost all examinations are carried out in a hospital setting.
After intensive examination and treatment, patients in most cases should be followed-up on an outpatient basis, primarily in day hospitals at polyclinics and hospitals.
Inpatient care is the main health care cost. The transfer of a part of medical care to hospital-replacing technologies (day hospitals, etc.) to the outpatient stage will allow not to reduce the volume and level of accessibility of medical care and to actually increase the level of use of health care resources. Therefore, the decrease in the volume of inpatient care provided for in the program, compared with the actual volume of this type of care, corresponds to an increase in the volume of days of treatment in day hospitals, day hospitals and home hospitals.
The standard for the volume of inpatient care is 2812.5 bed-days, including 1942.5 bed-days for the basic program.
The indicator of the volume of ambulance services is expressed in the number of calls per 1000 people. The standard of calls is 318 calls.
The section “Health financing per capita standards” provides concepts and principles for determining these standards.
Head standardsfinancing of health care are indicators that reflect the amount of funds to compensate for the cost of providing free medical care per 1 person.
The per capita standards for financing health care are formed by the executive authorities of the constituent entities of the Russian Federation based on the indicators of the cost of medical care according to its types, determined by them.The equalization of the conditions for financing territorial programs of state guarantees for the provision of free medical care to citizens of the Russian Federation is carried out in the manner prescribed by the budgetary legislation and the legislation on compulsory medical insurance of the Russian Federation. In accordance with the current procedure, budgets of a higher level subsidize budgets of a lower level by allocating transfers in the event of a justified shortage of financial resources from the latter. In the system of compulsory health insurance, the Federal Compulsory Health Insurance Fund allocates subventions to territorial compulsory health insurance funds.
The program is being implemented at the level of the constituent entities of the Russian Federation in accordance with the territorial programs of state guarantees for the provision of free medical care to citizens of the Russian Federation, which have the same structure as the federal program.
One of the main directions for improving management in the industry is the development of mechanisms for long-term planning of the Program of state guarantees for the provision of free medical care to the population of the Russian Federation for the medium term up to 5 years. The transition to a system of medium-term and then long-term planning of the Program will ensure a qualitatively new level of development of the system, the transition from the conditions of its survival to the intensification of development in accordance with the requirements of scientific and technological progress in health care. XXI century.
The implementation of this direction will require a longer time, but this is the most promising and significant direction of the Program's development.
In addition, there is such a method of financing as the development of a global budget. The economic sense of the global budget method - the alignment of the economic interests of the healthcare facility and the purchaser of medical services - is that the paying party changes the funding priorities.This method stimulates:
1) the validity of referring the patient from the clinic to the hospital;
2) creation of hospital-substituting forms of providing medical services;
3) the search for forms of cooperation with doctors of polyclinics or the creation of their own outpatient departments, if they do not exist;
4) cost savings for complex cases.
The global budget is formed as a financial plan. The condition for its implementation is the free disposal of resources, the maneuvering of them. The results of the transition to the global budget method should be:
Reducing the number of hospitalizations;
Increase in resources for one case of inpatient care;
More efficient use of outpatient care;
Establishment of contractual rates of payment for services rendered instead of fixed tariffs.
Thus, one of the most important problems in health care is the financing of the industry. In the strategic plan, financing of health care from public funds (budget and compulsory medical insurance) should retain its dominant role and provide opportunities for the state to carry out its policy and legal regulation of the health care system. At the same time, the practice of prioritizing financing (for example, community care) should be strengthened while taking measures to reduce the cost of beneficial interventions and to strengthen control over the effectiveness of the use of available limited resources.
The most striking indicator of the degree of socio-economic development of a society are indicators of population health. The statistics of the last decade indicate a decrease in the birth rate and life expectancy, as well as the provision of assistance to the population from the health care system. The relevance of this problem lies in its vital importance for every person.
In the new economic conditions, one of the forms of social protection of the country's population is medical insurance, which is mandatory. The law of the Russian Federation, which approved the organizational and economic aspects of contributions covering health care costs, increases the interest and responsibility of each person, as well as enterprises and the state in general, in health protection. This normative act ensures the rights of a citizen of the Russian Federation to receive medical care, which are enshrined in the country's constitution. The purpose of this law is to finance preventive measures and guarantee the provision of medical services to everyone who has an insured event.
The public health system is also funded by voluntary contributions. VHI is used to provide residents of the country with additional medical services. Their provision is not included in the CHI system. Both individual citizens who are capable of acting and enterprises that represent the interests of their employees can act as insurers under VHI. According to the system of supplementary insurance, health care institutions are provided only to those citizens who timely and in full transfer under the concluded agreement. The amount of premiums depends on the health status of the insured and the prices that medical institutions set for their services. Typically, a VHI agreement is concluded for a period that does not exceed twelve months. However, it is advisable to sign it for a longer period of time. Voluntary health insurance does not apply to services provided through compulsory health insurance.
Currently, domestic health care requires an additional infusion of monetary resources, as well as their most efficient use. This should happen by increasing competition between medical institutions and improving the insurance system.
The territorial CHI fund acts as an economic intermediary in the medical services market.
The subjects of the federation funds collected from the VHI funds are transferred to the CHI funds as follows: 40% - to the Federal CHI fund, and 60% - to their territorial CHI fund. In addition, the territorial CHI fund receives funds from the Federal CHI fund. The funds received, which make up the territorial CHI fund, are distributed as follows:
5% is left by the territorial CHI fund for its own needs (business management, salaries of employees, etc.);
15% of funds go to the Insurance Stock of Funds for fixing medical care in unforeseen circumstances;
80% of the funds are transferred to insurance companies, which leave 2% for the purposes (of doing business), the remaining 78% are used to finance health care facilities.
VHI funds in the Russian Federation also act as an intermediary in the medical services market. The funds collected under individual contracts of patients with the VHI fund are used as follows:
5% are transferred for additional financing of the budgetary and insurance health care of the administrative territory in which the VHI fund is located;
20% of the territorial fund of the VHI leaves for their own needs;
75% is used to personally finance the treatment of policyholders in accordance with the terms of the contract.
The main tasks of the VHI fund:
improve health financing;
protect the patient from abuse by health care providers.
Funding sources can be:
1. General tax revenues of all types and levels.
2. Targeted tax revenues.
3. Target contribution for compulsory health insurance (or payroll tax).
4. Personal funds of citizens and other sources.
A system based on general tax revenues is called a budget system.
Systems based primarily on earmarked health insurance contributions are called compulsory health insurance systems.
Personal funds of the population as the main source of payment for medical care are the basis of the private financing system. No country has a purely budgetary, insurance or private financing system.
In addition to financing from taxes, health care should have other sources of funding: excise taxes, taxes and fines imposed on tobacco products, alcoholic beverages, environmental violations, gambling and other activities that have an adverse effect on health.
Population aging has become a major socio-demographic problem in developed countries. On the one hand, there is an increase in demand for medical services, and on the other, an increase in the demographic burden on workers, which complicates the problem of financing health care. The increase in demand for medical services is also caused by the development of modern technologies, which provide new opportunities in the field of treatment of various diseases, and, accordingly, the basis for the emergence of new expectations from the population.
Sources of funding for medical activities.
1.budgetary funding;
2. insurance premiums of compulsory medical insurance;
3.VHI insurance premiums;
4. paid services;
5. income from securities;
6. gratuitous contributions and donations;
7. other sources not prohibited by law. At the moment, funds from the budget are sorely lacking. Budget funding is not fully implemented, i.e. the level of funds is very low, and the list of diseases for which the budget is financed is very small.
Financing of health care facilities in the CHI system is carried out according to several schemes:
1) according to the estimate provided by the healthcare facility;
2) for each patient treated;
3) by the end result (medical efficiency).
Currently, the principle of payment for each treated patient is becoming more widespread, taking into account the degree of his cure and the economic efficiency of the activity of medical institutions. This contributes to a more efficient use of funds.
No. 39 Cost minimization method
This method reduces decision making to a simple choice of the cheapest option, but is not at all limited to just estimating costs. To form a qualified opinion about the advantages of a particular option, it is necessary to be sure that there are no differences in the results of options or that these differences are insignificant.
At the level of healthcare institutions, a method of minimizing costs for state or municipal purchases of the same type of equipment, food, medicines. In recent years, the legislation in this area has been improved, which greatly facilitates the task of applying this method in practice. Savings from conducting competitive and quotation procedures can be very significant.
The cost minimization method can also be applied in the development of medical and economic standards (protocols) for the treatment of individual diseases. For this, several options for the standard of treatment should be created:
Simple (minimal) - with the use of the simplest drugs, the simplest operations and manipulations and a minimum of diagnostic studies using simple diagnostic equipment.
Complex (extended) - with the use of the most effective drug treatment regimens, the use of manipulations and surgical interventions according to the latest achievements of medical science and the capabilities of world-class equipment.
Optimal (average) is a certain average value from the first two options.
The following indicators are used to analyze the efficiency of expenditures in health care using the cost minimization method:
characterizing the structure of health care financing from various sources in general and per capita (budget, compulsory health insurance funds);
characterizing the structure of financing by type of care (inpatient, outpatient, inpatient replacement, ambulance);
characterizing the structure of financing health care organizations according to the economic classification of costs;
depreciation of fixed assets of health care;
the volume of medical care per capita in the context of types of medical care.
Cost-effectiveness method.
This method involves comparing options for spending funds aimed at achieving a single goal and differing not only in costs, but also in the degree of achievement of the final result. It is important that using the cost-effectiveness method it is possible to compare completely different health programs aimed at a common goal. So you can compare programs aimed at treating heart disease, preventing tuberculosis, kidney dialysis for kidney failure, and so on. The main thing is that these programs set a common goal (for example, prolonging the life of the population).
To assess the effectiveness of healthcare using the cost-effectiveness method, along with the listed indicators of the volume of medical services (bed-days per 1000 people by profiles and levels of medical care, the number of patients treated, the number of visits per 1000 people, the number of ambulance calls per 1000 people, the number of days spent in day hospitals per 1000 people), you can use a group of the following indicators to measure the results of the health care system and its institutions:
morbidity of the population (the number of diseases registered in patients with a newly diagnosed diagnosis per 1000 people), including by the main classes of diseases;
the totality of all patients with this disease who applied to outpatient clinics both in the current and in previous periods and registered at the end of the reporting period;
morbidity of the population with temporary disability is characterized by the number of calendar days of temporary disability;
primary disability - the number of persons recognized as disabled for the first time in the current year;
mortality;
the number of complaints from the population about the quality of medical services provided.
Social efficiency is the degree to which a social outcome is achieved. In relation to a particular patient, this is his return to work and active life in society, satisfaction with medical care. At the level of the entire industry, this is an increase in the life expectancy of the population, a decrease in the level of mortality and disability rates, and the satisfaction of society as a whole with the system of medical care.
Economic efficiency is the ratio of the results obtained and the costs incurred. The calculation of economic efficiency is associated with the search for the most economical use of available resources. This indicator is a necessary component in assessing the functioning of the health care system as a whole, its individual subdivisions and structures, as well as the economic justification of measures to protect the health of the population. Economic efficiency in health care is considered in two directions: firstly, the efficiency of using various types of resources, and secondly, from the point of view of the impact of health care on the development of social production as a whole. The peculiarity of health care is that often medical measures of a therapeutic and prophylactic nature can be economically unprofitable, but the medical and social effect requires their implementation. So, when organizing medical care for elderly people with chronic and degenerative diseases, patients with mental retardation, etc. with obvious medical and social efficiency, the economic effect will be negative. With the use of modern medicines, intensive therapy and resuscitation, a medical and social effect is achieved - a person's life is saved, but he can become disabled and lose the opportunity to engage in socially useful work. Economic efficiency in health care cannot be decisive when choosing one or another means of prevention, treatment, organizational forms of medical care. However, cost-effectiveness criteria - along with medical and social effectiveness - can help to prioritize interventions in resource-limited settings.
With regard to targeted programs in the health sector, the effectiveness of the implementation of programs is assessed on the basis of an analysis of the achievement of target values of performance indicators established by the passports of these programs.
The effectiveness of the implementation of the program assesses the ratio of the results and the resources spent on their achievement. It is the analysis of effectiveness that is the key goal in assessing the implementation of programs, since it allows one to judge not only the effectiveness of the implementation of the program, but also calculates the cost of the results achieved, which provides more complete and balanced information on the feasibility of implementing the program at the preliminary stage of assessment and the results of implementation at the final stage. ...
In a number of works, in order to systematize approaches, the concept of effect means the difference between benefits and costs incurred, while efficiency is understood as the ratio of these values. Thus, the effect and effectiveness of programs is assessed based on objective quantitative criteria - indicators of effect and effectiveness, respectively. Due to the fact that budget target programs are aimed at implementing the expenditure obligations of the state (municipality) in the field of social and economic development of society, the benefits from the implementation of the program are understood as a set of socially significant (hereinafter - social) results. According to other classifications, the effect of targeted programs is understood as a set of social effects, and efficiency is the difference or ratio of social effects and budgetary allocations aimed at their implementation.
The social effect of the implementation of budget target programs means direct and indirect socially significant results obtained in the implementation of activities of budget target programs.
Thus, effect indicators are a limited set of socio-economic indicators that are selected separately for each of the assessment parameters. According to generally accepted approaches, performance indicators must meet a number of requirements, which in the modern scientific literature include:
measurability - the indicator is measurable in constant units;
validity - the indicator reflects as fully as possible what needs to be assessed;
unambiguity - the indicator has a clear, generally accepted definition and units of measurement;
sustainability - during the assessment, time (dynamic) slices of the indicator's data are available;
availability - the data required to calculate the indicator are available in traditional sources of information;
achievability - the set target value of the indicator can be achieved using available resources;
attachment to a certain reporting period;
specificity and specificity - the indicator refers to a specific organization or program.
The goal of reforming the health care system is to improve public health by increasing the availability and quality of medical care for the general population, developing the preventive focus of medical institutions and promoting a healthy lifestyle while increasing the efficiency of using the financial, material and human resources of the industry. Currently, the main directions of health care reform are the improvement of the regulatory framework and the financial and economic mechanism of the industry, the scientific organization of the provision of medical care, including the use of the principles of evidence-based medicine and mathematical modeling of the activities of medical and preventive institutions (LPI), the formation of personal attitudes of people in favor of a healthy lifestyle and perception of health as the most important value in life. Thus, the systemic reform of the industry should include at least three mandatory components: 1. Financial and economic reform, including the restructuring of health care. 2. Improving the quality of industry management based on scientifically based technologies of modern healthcare management. 3. Development of medical practice based on the principles of evidence-based medicine and the results of clinical and economic analysis.
By order of the Government of the Russian Federation No. 2511-p of December 24, 2012, the "State program for the development of healthcare in the Russian Federation" was approved.
The main principles of public health protection, enshrined in the Federal Law "On the Fundamentals of Public Health Protection in the Russian Federation", determined the structure and objectives of the Program. These include:
ensuring the priority of prevention and development of primary health care,
increasing the efficiency of the provision of all types of specialized medical care,
development and implementation of innovative methods of diagnosis, prevention and treatment, as well as the basics of personalized medicine,
improving the efficiency of obstetrics and childhood services,
development of a rehabilitation system, spa treatment, palliative care,
improvement of drug supply for the population,
providing the health care system with highly qualified personnel motivated to work effectively,
ensuring the consistency of the organization of health care and management of the industry,
increasing the effectiveness of control and supervisory functions in the field of health protection.
Thus, the Program reflects systemic approaches to solving such fundamental issues for the industry as
formation of a unified preventive environment,
improving the quality of medical care and satisfaction of the population with its quality,
increasing the level of training and qualifications of medical personnel, increasing the salaries of medical workers on the basis of an effective contract,
carrying out institutional transformations in the industry, improving the medical infrastructure and informatization of health care.
The state program includes 11 subprograms, each of which corresponds to one of the assigned tasks.
The implementation of the Program is planned in two stages.
The first stage (2013–2015) is dedicated to the completion of systemic transformations laid down in the Federal Law "On the Fundamentals of Health Protection of Citizens in the Russian Federation"
The second stage (2016-2020) is the development of the first and is dedicated to building the quality potential of health care based on an optimized organizational model and maintaining the financial balance of state guarantees
Economic evaluations in health care. Question number 40.
Cost-benefit method. Recently, great importance has been attached to the use of economic analysis and economic assessments in health care.This is due to many reasons, among which one can single out the limited resource provision of health care (personnel, equipment, funds, information resources), which is typical not only for our country, the need for a more complete and rational use of available resources, the importance of improving the efficiency of the entire system, its individual services and institutions. In this case, efficiency is understood as the ratio of the results of activities to the costs of resources produced, which, in fact, is the content of economic analysis. Previously, this kind of work was simply not feasible, since there were no specialists in the field of economic analysis in health care, which, moreover, acquired its fullest shape only in recent years. Performing economic analysis and evaluating its results is a rather complicated process, often requiring special knowledge and skills. That is why in developed countries the course of economic analysis of medical programs is an integral part of the training of economists and health managers. In addition, economic analysis is already being used in clinical practice to assess the effectiveness of treatment technologies used for various diseases. Especially this direction has been developed with the use of Evidence-Based Medicine methods, based on statistically proven links between the chosen treatment methods (technologies) and treatment results. By the way, efficiency is one of the main characteristics of quality assurance of medical care. Now is the time when healthcare cannot develop further without such work, especially in the context of external market relations. The time has come, as they say, to count and take everything into account. Almost all programs, projects and activities in health care require economic analysis and evaluation. At the same time, the assessment should be systematic - at the pre-project stage, in the process of implementing projects (activities) and as a result of project implementation. Thus, for a reasonable assessment of efficiency, it is necessary to have not only reliable resultant indicators, but also quite definite costs, and both the results and costs should be presented not only in general form, but also for individual sections of the service or medical institution. Economic analysis methods. There are four main methods of complete economic analysis: cost - minimization analysis - costs - cost - effectiveness analysis - costs - cost - benefit analysis - costs - usefulness or usefulness of costs (cost - utility analysis). A complete economic analysis involves identifying, measuring and comparing the costs and benefits of two or more alternatives, providing the basis for a qualified and informed choice. Based on the definition of economic analysis, any form (any method) should include an assessment and comparison of costs and benefits. Methods for identifying, measuring in monetary terms and comparing costs are practically the same for all forms of analysis. However, the methods for assessing the results of various actions and programs critically depend on the alternatives being compared and, moreover, differ significantly from each other. That is why the methods of economic analysis differ in the way they evaluate the results. Cost-benefit method or economic cost-benefit analysis. The results of alternative options for the activity of the service can not always be reduced to a single natural indicator. Some measures aim to improve certain working conditions for workers, others - to improve the quality of nutrition in hospitals, and still others - to optimize the length of hospital stay or reduce levels of environmental pollution, etc. To compare such heterogeneous alternatives, it is necessary either to single out a single priority indicator in all compared alternatives, which is rarely possible, or to find an indicator that will unambiguously express the value of the whole set of diverse results. One of the measures of value is money, so you can try to measure all the results for each alternative in monetary terms, in terms of the benefits obtained, and then compare this benefit with the costs incurred. The method of expressing both costs and results in monetary terms is called the cost-benefit method. The result of applying this method is expressed either in the form of a ratio of monetary costs to monetary gain, or in the form of a sum (possibly negative) showing the net profitability or unprofitability of one alternative compared to another. In the latter case, you can evaluate the resources that have been saved or created by choosing this alternative. Presenting results in monetary terms has several advantages and disadvantages. The main advantage is that by expressing the results in rubles or in any other currency, one can compare extremely heterogeneous alternatives aimed at achieving qualitatively different results. The main disadvantage of the method is a direct consequence of its advantage: it can be extremely difficult to present some effects in rubles. Therefore, cost-benefit analysis is applicable only in cases where such a representation can be reasonably convincing and clearly justified. There are, however, cases where this method is a simple and natural form of economic valuation. For example, preventive programs, food quality control, etc. lead to savings in subsequent costs of treatment for those patients who could become ill without such programs and activities. The resulting savings are the benefits. The second case where such an analysis is acceptable is the provision of paid services. Here the benefit is simply the difference between the amount of revenue and the costs incurred. Take a health care enterprise as an example and consider how management responds during an epidemic such as influenza. It is known that every year, and sometimes twice a year, influenza epidemics break out all over the world. During a typical epidemic, 10 to 30 percent of the population falls ill. The most susceptible to diseases are children attending children's institutions and adults who work in large teams or have extensive contacts due to their production activities: during a typical epidemic, up to 60% of children and adult groups fall ill. The disease is most severe in the elderly, children and in persons suffering from chronic diseases, causing frequent complications (in risk groups up to 20%). In a mild form of flu, people who get sick often continue to work without going to a doctor, but infecting other members of the team. Mortality from complications of influenza reaches 2.9% of the number of cases. Naturally, the world is looking for ways to prevent influenza. There are several basic approaches to prevention. 1. Vaccination of the population. Modern vaccines, the composition of which is changed annually in accordance with WHO recommendations. Timely vaccination reduces the incidence of influenza by 84-98% (according to various sources) within at least 9 months from the date of vaccine introduction. The price of a vaccine per person ranges from 150 to 300 rubles, increasing as the seasonal outbreak of influenza approaches. If the disease does occur, then it proceeds easily and in the vast majority of cases without complications. 2. Preventive measures during an influenza epidemic (interferon, oxalic ointment, vitamins, remantadine, etc.) reduce the likelihood of illness by 25% and do not change the likelihood of complications. The cost of medicines is approximately 30-50 rubles. depending on the drugs chosen. Purpose of the analysis: to determine the economic effect of each course of prevention. The analysis should be performed from the point of view of the management of the specified enterprise, who wants to minimize the economic damage from absenteeism of employees during an outbreak of influenza. Analysis. The losses incurred by an enterprise from an outbreak of influenza are primarily associated with non-manufactured products. Suppose that the average daily output of one employee of the enterprise is 200 rubles. Let the company have 200 employees. During an epidemic, about 20% of all workers fall ill, half of them see a doctor and receive a sick leave for about 10 days, the rest continue to go to work, but for 10 days of illness, their productivity decreases by 50%. With vaccination, the incidence decreases by 90%, and with prevention during an epidemic, by 25%, while the behavior of the sick remains the same, that is, only half of them will go to the doctor. In the absence of preventive measures, the losses of the enterprise amount to 20x200x10 + 20x100x10 = 60,000 rubles. The cost of the vaccine is 150x200 = 30,000 rubles. Losses of the enterprise from morbidity during vaccination are 2x200x10 + 2x100x10 = 6000 rubles. The benefit of the enterprise during vaccination is 60,000-30,000-6000 = 24,000 rubles. The benefit-to-cost ratio is 24,000: 30,000 = -0.8, that is, for every ruble spent on vaccinations, the company receives an additional 80 kopecks. benefits. In the case of prophylaxis during an epidemic, the costs are 40x200 = 8000 rubles, losses due to morbidity are 15x200x10 + 15x100x10 = 45,000 rubles. The benefit of the enterprise due to preventive measures during an epidemic is 60,000-45,000-8,000 = 7,000 rubles. The benefit-to-cost ratio is 7000: 8000 = 0.875, that is, the company receives an additional 87.5 kopecks. for every ruble spent. What kind of preventive program should the management of the enterprise choose? It depends on the means at the disposal of the enterprise and on the social policy it pursues.
Basic terms. Cost analysis is the process of assessing the cost of resources or benefits received in monetary terms. Investments (input) - the total amount of target resources used to achieve the goals and orderly functioning of the system. Activity - a general definition of the work performed by personnel in achieving their goals. Each such activity includes a group of tasks. A group of activities is a way of performing a specific function. Costs (cost) - resources expended in the process of achieving the goals or the implementation of specific activities. This also includes unrealized benefits. DALY index (Disability-adjusted life years) - an index reflecting the number of years of life, adjusted for disability. The QALY (Quality-adjusted life years) index is an index reflecting the years of good quality. Quality of life is a life that does not have any obstacles to the performance of vital functions from health and disabilities. Benefit - a positive result of purposeful actions that have caused certain costs of resources. Calculation of cost (costing) - methods, processes for determining the amount of costs (actual or estimated) that are necessary for specific purposes, products, services, processes or activities. Calculation of the cost of a unit of production is a method by which the result is divided into separate units of measure, for example, the cost of one analysis, measurement, one vaccination, one visit to the object, etc. can be determined. Cost is the average price of the service or material used for a given real unit. An outcome (outcome) is a characteristic of the state of an object, process, phenomenon, system obtained in the process of achieving the final goal or when it is achieved. The result can be expressed in physical terms, in value (economic) form or other measures of measurement. The effectiveness, for example, of the state sanitary and epidemiological supervision is defined as the real value of changes in sanitary and epidemiological welfare and the effectiveness of the influence of objects that have occurred over a certain period of time (Kutsenko G.I. and others). Cost containment - any regulation of prices for goods, services and activities that prevent the increase in the cost of health care costs. Service (service) - the result of single actions of the supplier to meet the needs of consumers. Health care economics - all economic aspects of health care, from assessing the cost of services and resource costs to assessing their effectiveness. Efficacy - The degree to which medical or hygiene interventions are effective to improve health under ideal (laboratory, experimental) conditions. Effectiveness - the degree to which a health or hygiene intervention is effective in improving health in a real-world setting, i.e. improve the result. Efficiency is the ratio of results, including improved health, to costs incurred, i.e. spent resources (first of all, financial, personnel, material and technical, time, information and intellectual). It is important to know that efficiency is always relative, i.e. when we talk about efficiency, it means that alternative solutions for the use of resources are always compared. There can be no absolute efficiency, because the value of the ratio "results-costs" in itself does not say anything without comparison with another of the same ratio, but characterizing an alternative use of resources (another preventive program, other sanitary and hygienic measures, another treatment tactics etc.). Ensuring efficiency means making informed decisions about the alternative use of resources and implementing them. Why is the question of choosing among the possible alternatives being raised? Because the resources noted above are always limited, the "product" of the activities of both sanitary-epidemiological and medical-preventive institutions is also limited, because the results do not always depend only on them. Technological efficiency (technical efficiency) - such an organization (technology of use) of existing resources, which allows you to get the best result. In other words, resources should not be lost, they should not be idle or not fully utilized. Cost-effectiveness efficiency is achieved with an optimal combination of results and resources expended. To ensure cost efficiency, direct and inverse optimization problems can be solved: direct - obtaining the maximum result at a given acceptable cost and inverse - minimizing costs for a given, necessary, expected result. But in practice, as will be shown below, most often they strive to simultaneously solve two problems - and get the maximum possible result and at the same time minimize costs. For all three options, it is necessary to build models and carry out the corresponding calculations, the complexity of which increases from the first to the third task. It is usually assumed that when solving cost efficiency problems, the problem of technological efficiency of using available resources has already been solved (a resource unit gives the maximum possible result and does not stand idle). Efficiency of investments (allocative efficiency) - includes investments and allocation of resources to achieve maximum compliance of the results obtained with the needs of the population.
Characteristics of the Healthcare system. Question number 41.
In recent years, the healthcare system of the Russian Federation is undergoing a reorganization process, which is carried out under the influence of three most important factors.
First, the intensive implementation of the Federal Law of 06.10.03. №131-ФЗ "On general principles of organization of local self-government in the Russian Federation" in terms of the redistribution of powers of different levels of government in providing the population with medical care, in particular, the transfer of specialized types of assistance from the municipal government to the regional level.
Secondly, the implementation of the national priority project "Health", which created a resource basis for the implementation of the main principle of structural reorganization - increasing the role of primary health care.
The third most important factor of state policy that influenced the increase in the structural efficiency of health care is the improvement of the quality and availability of drug supply for the population, during which a list of vital drugs was approved for additional provision of certain categories of citizens.
The mechanism for providing citizens of the Russian Federation with high-tech medical care has been changed. The standards have been introduced and the norms of financial costs for the provision of high-tech types of assistance have been calculated.
From January 1, 2006, the issuance of the "Birth certificate" began, which allowed pregnant women during pregnancy and childbirth to fully exercise their right to choose an antenatal clinic and a maternity hospital, as well as to form healthy competition among health care institutions that provide assistance to women during pregnancy and childbirth.
In accordance with the instruction of the President of the Russian Federation on the development of Russian health care in 2006-2008, mechanisms for managing the industry were developed, which make it possible to implement public obligations of the state in the field of health care in accordance with a standard that is uniform in all territories of the Russian Federation, which ensures an increase in the quality of services in the health care system.
1. The healthcare system of the Russian Federation
Today, "health care" is understood as the social and social function of society (state) to protect and improve the health of the population. The peculiarity of the current moment is the organizational restructuring of health care, characterized by a multitude of types of medical care. Along with the main budgetary and health insurance system, new models of medical care for the population are being formed, primarily private medicine.
The budgetary insurance system of health care is provided with funds from the state budget (federal and regional) and extra-budgetary means of health insurance - compulsory state social health insurance (MHI) and voluntary, private health insurance (VMI).
1.1 Health care structure
The “vertical” of management and control over health care institutions includes ministerial (federal), regional (large centers and cities) and local (municipal) levels. State (federal, regional, municipal) health authorities have the right to control the work of private medical institutions and private practicing doctors. In turn, the administrative executive bodies responsible for the public health system are under the jurisdiction of the legislative authorities (State Duma, Federation Council). Supervision over the implementation of laws in the field of health care, in turn, is carried out by bodies and institutions of the judiciary.
A special role in our state is assigned to the structures of presidential power. According to the constitution, it is the President of the Russian Federation who directs the state policy in the field of protecting the health of citizens. Structurally, organizationally, the public health system integrates various types of enterprises and institutions:
federal and regional bodies and health care institutions (state, budgetary health care system); ... State health care system
The state health system includes the Ministry of Health of the Russian Federation, the ministries of health of the republics within the Russian Federation, health authorities of the autonomous region, autonomous districts, territories, regions, cities of Moscow and St. Petersburg, the Russian Academy of Medical Sciences, the State Committee for Sanitary and Epidemiological Surveillance of the Russian Federations, which, within their competence, plan and implement measures to implement the state policy of the Russian Federation, implement programs in the field of health care and develop medical science. The state health care system also includes the state-owned and subordinate to the state health system management bodies, medical and preventive and research institutions, educational institutions, pharmaceutical enterprises and organizations, pharmacies, sanitary and preventive institutions, forensic medical examination institutions, financial services. - technical support, enterprises for the production of medicines and medical equipment and other enterprises, institutions and organizations.
The state health care system includes medical and preventive institutions, pharmaceutical enterprises and organizations, pharmacies created by ministries, departments, state enterprises, institutions and organizations of the Russian Federation in addition to the Ministry of Health of the Russian Federation, ministries of health of the republics within the Russian Federation.
Enterprises, institutions and organizations of the state healthcare system, regardless of their departmental subordination, are legal entities and carry out their activities in accordance with these Fundamentals, other acts of legislation of the Russian Federation, republics within the Russian Federation, legal acts of an autonomous region, autonomous districts, territories, regions, cities of Moscow and St. Petersburg, regulations of the Ministry of Health of the Russian Federation, ministries of health of the republics within the Russian Federation, health authorities of the autonomous region, autonomous districts, territories, regions, cities of Moscow and St. Petersburg.
Municipal health care system
The municipal health care system includes municipal health authorities and municipal-owned medical and preventive and research institutions, pharmaceutical enterprises and organizations, pharmacies, forensic medical institutions, educational institutions that are legal entities and operate in accordance with with these Fundamentals, other acts of legislation of the Russian Federation, republics within the Russian Federation, legal acts of an autonomous region, autonomous okrugs, territories, regions, cities of Moscow and St. Petersburg, regulations of the Ministry of Health of the Russian Federation, ministries of health of republics within the Russian Federation and local government bodies.
Municipal health authorities are responsible for the sanitary and hygienic education of the population, ensuring the availability of the guaranteed volume of medical and social assistance to the population, the development of the municipal health care system in the subordinate territory, exercise control over the quality of the provision of medical and social and drug assistance by enterprises, institutions and organizations of the state, municipal , private health care systems, as well as those in private medical practice.
Financing of the activities of enterprises, institutions and organizations of the municipal health care system is carried out at the expense of budgets of all levels, trust funds intended to protect the health of citizens, and other sources not prohibited by the legislation of the Russian Federation.
Private healthcare system
The private health care system includes medical and prophylactic and pharmaceutical institutions, the property of which is in private ownership, as well as persons engaged in private medical practice and private pharmaceutical activities.
The private health care system includes treatment-and-prophylactic, pharmacy, research institutions, educational institutions, created and financed by private enterprises, institutions and organizations, public associations, as well as individuals.
The activities of institutions of the private health care system are carried out in accordance with these Fundamentals, other acts of legislation of the Russian Federation, republics within the Russian Federation, legal acts of the autonomous region, autonomous districts, territories, regions, cities of Moscow and St. Petersburg, regulations of the Ministry of Health of the Russian Federation, ministries of health of the republics within the Russian Federation and local governments.
To ensure diverse activities and medical functions, a profile of health care institutions is distinguished:
Treatment-and-prophylactic.
Protection of motherhood and childhood.
Sanitary and Epidemiological Service.
Sanatorium and health resort.
Pathological, forensic, forensic psychiatric examination.
Pharmacy.
Medical industry enterprises: medical devices and pharmaceuticals.
Educational and research.
1.2 Ministry of Health
The scope of activity of the Ministry of Health and Social Development of the Russian Federation is determined by the Regulation on the Ministry, approved by the Government of the Russian Federation of June 30, 2004 No. 321, which is the federal executive body responsible for the development of state policy and legal regulation in the field of health care, social development, labor, physical education, sports, tourism and consumer protection. Key business issues:
healthcare, including the organization of medical prevention and medical care, pharmaceutical activities;
quality, efficacy and safety of medicines;
resort business;
sanitary and epidemiological welfare;
living standards and incomes of the population;
salary;
pension provision;
social insurance;
working conditions and labor protection;
social partnership and labor relations;
employment of the population and unemployment;
work migration;
alternative civilian service;
social protection;
demographic policy;
physical Culture and sport;
consumer rights Protection.
Structural divisions are departments for the main areas of activity of the Ministry:
Federal Service for Labor and Employment.
Federal Service for Supervision of Consumer Rights Protection and Human Welfare.
Federal Service for Surveillance in Healthcare and Social Development.
Federal Agency for Healthcare and Social Development.
Federal Agency for Physical Culture, Sports and Tourism.
Federal Medical and Biological Agency.
Federal Agency for High-Tech Medical Assistance.
The Ministry also coordinates the activities of the Pension Fund of the Russian Federation, the Social Insurance Fund of the Russian Federation, and the Federal Compulsory Medical Insurance Fund.
Goals and objectives of the Ministry:
Raising the material standard of living of the population;
Improving the level of health of the population;
Meeting the needs for social services and social support;
Providing productive employment and decent working conditions;
Reproduction and development of the potential of labor resources.
The measures carried out in these areas, along with other measures of social orientation, primarily to increase wages and increase employment of the population, will contribute to solving the main task - a consistent increase in the level and quality of life of the population, poverty reduction, and ensuring universal accessibility of basic social services.
The mission of the Ministry of Health and Social Development of the Russian Federation in the light of the implementation of constitutional guarantees and the rights of citizens of the Russian Federation on the basis of the provisions of the messages of the President of the employment, strengthening social protection of vulnerable groups of the population.
In addition, the Ministry of Health and Social Development of the Russian Federation is involved in achieving the following strategic goals of the country:
Increasing the level of satisfaction of the need for education;
Development of scientific potential;
Development of the potential of public administration (increasing the efficiency of the activities of executive authorities);
Development of the potential of international relations.
Accessibility of medical services: the essence of the regulatory aspects of the problem. Question number 42. Currently, most of the volume of mass medical care is provided in medical and prophylactic institutions (LPI) at the municipal level. Thus, it is the budgetary institutions that bear the main burden in the healthcare sector. In connection with the transition to market relations in the field of medical care, activities began to appear, carried out both free of charge and on a paid basis. In this regard, problematic situations arise due to the unintentional and sometimes even deliberate substitution of medical care for medical services, which entails serious consequences in medical, economic and legal aspects. For any patient, getting medical care or getting medical care instead of it makes a significant difference. As noted in the literature, this issue is extremely serious, since behind this are living people, the resources used, paid and free, quality, accessibility and much more, which ultimately cannot but affect the health of citizens and the moral foundations of health care. 41 of the Constitution of the Russian Federation, everyone has the right to medical care. Thus, it is medical care that is the object of constitutional law. This is the main legal difference between medical care and medical services, which is the fundamental principle of legal, economic and medical features. It is similar to the fact that the Constitution is the foundation for all regulatory legal acts of the Russian Federation, which only develop its provisions. Thus, the Constitution of Russia enshrines the right to medical care in general, and the specification of various aspects of the implementation of this right is reflected in the regulatory legal acts of the federal and regional levels. At the federal level, such documents are the Fundamentals of Legislation of the Russian Federation on the Protection of Citizens' Health<2>(Fundamentals) and the Program of state guarantees for the provision of free medical care to citizens of the Russian Federation, which includes the basic program of compulsory medical insurance (MHI), in accordance with which the citizens of Russia are provided with a guaranteed amount of free medical care. Unfortunately, these legal acts do not provide clear criteria for distinguishing between medical care and medical services. Among the fundamental regulatory legal acts in the modern healthcare system of the Russian Federation, it is necessary to highlight the Law of the Russian Federation "On medical insurance of citizens in the Russian Federation"<3>regulating the issues of both the provision of medical care and medical services. At the same time, these categories are used by the legislator as synonyms, which leads to the emergence of a number of legal conflicts due to the substitution of these concepts. Regions in the development of federal legislation adopt their own regulations .. The legal framework for the provision of medical services to the population is based on the Civil Code<4>and the Federal Law "On Protection of Consumer Rights"<5>... The procedure and conditions for the provision of paid medical services to the population (in addition to the guaranteed volume of free medical care) are approved at the federal level by Decree of the Government of the Russian Federation of January 13, 1996 N 27 "On approval of the rules for the provision of paid medical services to the population by medical institutions"<6>... The procedure for the provision of paid medical services is also regulated by the relevant legal acts at the regional level. One of the important legal differences between medical care and medical services is the need to obtain voluntary informed consent from the patient for medical intervention. So, in accordance with Art. Art. 30, 32 Fundamentals every patient has the right to informed voluntary consent to medical intervention. The provision of medical services should be carried out only after obtaining such consent - it is a prerequisite for any medical intervention. The provision of medical care has its own characteristics. So Art. 34 of the Fundamentals allows the provision of medical care (medical examination, hospitalization, observation and isolation) without the consent of citizens or their legal representatives. In such situations, the question of holding it in the interests of the citizen in accordance with Art. 34 Fundamentals are decided by a council, and if it is impossible to collect a council, by the attending (duty) doctor directly with the subsequent notification of the officials of the medical and preventive institution. In turn, the Criminal Code of the Russian Federation even obliges in a number of cases to provide medical care, including without the consent of the patient (Articles 124, 125 of the Criminal Code of the Russian Federation). The differences between medical care and medical services are most pronounced in the economic sphere. This is primarily due to funding issues. Funds from the provision of medical services come from the funds of the customer (or payer) - legal entities and individuals with whom contracts are concluded for the provision of a certain amount of medical services either directly from a healthcare facility or through medical insurance organizations (voluntary medical insurance system). In turn, the provision of medical care in accordance with Art. 37.2 of the Fundamentals and Section III of the State Guarantee Program is financed from the CHI funds in accordance with the basic CHI program, as well as funds from the budgets of all levels of the budgetary system of the Russian Federation in accordance with the Program of state guarantees for the provision of free medical care to the citizens of the Russian Federation. In financing the provision of medical care, the municipal order of the healthcare facility for the provision of medical care to the population of a specific territory is of great importance.<7> ... Meanwhile, the question of the application of the state order to medical services is one of the poorly developed both in legal and methodological and organizational terms. At the same time, the state order for medical care is a long-established system. It is necessary to pay attention to the distinctive features of accounting (budgetary) accounting in the provision of medical care and medical services, which is due to the specifics of the legal status of budgetary healthcare institutions. One of the responsibilities of budgetary medical institutions is budget accounting (Article 162 of the Budget Code of the Russian Federation). Due to the peculiarities of the budget accounting account, consisting of 26 categories, where the type of funds is indicated in the 18th category (budget funds, paid activities, earmarked funds and funds in temporary disposal), it is possible to ensure the need for separate accounting by funding sources (budget funds; off-budget - from activities that generate income; targeted - funds of the compulsory medical insurance). In this regard, in budgetary medical institutions, the above financial flows are not mixed, but accounted for in different accounts. And consequently, in budgetary health care facilities, separate accounting of activities for the provision of medical care (budget) and medical services (extra-budgetary funds) is kept, which is reflected in the forms of financial statements. This is one of the features that distinguish medical care from medical services at the accounting and reporting level. There are also peculiarities in the maintenance of tax accounting for activities related to the provision of medical care, which distinguishes it from medical services. According to Art. 321.1 of the Tax Code of the Russian Federation, budgetary institutions as taxpayers financed from the budgets of the budgetary system of the Russian Federation or receiving funds in the form of payment for medical services provided to citizens within the framework of the territorial compulsory health insurance program, as well as receiving income from other sources, for tax purposes are required to maintain separate accounting of income and expenses received and made within the framework of targeted financing and from other sources. Other sources (income from commercial activities) include income of budgetary institutions received from legal entities and individuals from transactions in the sale of goods, works, services, property rights, and non-operating income. Income received by health care institutions from the provision of paid medical services, after taxes and other mandatory payments, in accordance with the current legislation, are directed to expenses related to the statutory activities of the institution, including the wages fund. The activity of the medical institution in the provision of medical care does not bring profit, and accordingly, the budgetary medical institution does not pay taxes on this type of activity. When determining the medical aspects of the differences between medical care and medical services, it is necessary to refer to the scientific medical literature. There is an established opinion according to which medical care is provided to a patient who is primarily in an urgent state, in cases of a threat to his life and health. It is free of charge. Medical services are provided on a reimbursable basis, and above all to improve the patient's quality of life. It is not imposed on the patient from the outside by the medical staff, but is requested by the patient himself from among the types of services provided by the healthcare facility according to the license and the price list. Thus, all actions in relation to patients that are not related to vital indications for them can be attributed to services. In other words, everything that provides the conditions for the provision of necessary medical care is in fact services that in health care can be of a service or paramedical nature.<9>... This approach is constructive due to the fact that it allows the most obvious differentiation of medical care from medical services. As can be seen from the above, medical care, being an object of the constitutional law of citizens of the Russian Federation, has a number of objective features in the legal, economic and medical aspects that distinguish it from medical services. In this regard, situations when there is an unintentional or even deliberate replacement of medical care for a medical service is unacceptable. Therefore, the above differences should be the basis for improving the regulatory framework of both local, regional and federal levels, which will allow not only a differentiated approach to resolving controversial situations in court between a patient and a healthcare facility, considering this or that situation, but also more objectively. and to reasonably distinguish whether in each specific case medical care or medical service was provided both for medical reasons and for the costs accounted for in the primary accounting documents in relation to this patient, which will subsequently prevent the emergence and need to resolve legal conflicts on this issue. Thus, in order to further avoid the emergence of legal collisions associated with the substitution of the concepts of "medical care" and "medical service" and, as a consequence, the replacement of medical care with a medical service, it is necessary to improve the regulatory framework in terms of unification of the conceptual apparatus, not limited only in the field of health care or in the economic sphere on a separate group of legal acts, and in the aggregate, taking into account the objectively existing triune (medical, economic and legal) essence of medical care as an object of the constitutional law of citizens of the Russian Federation. Here it becomes clear the need to systematize the existing regulatory and legal framework on this issue, which would make it possible to link existing regulatory legal acts into a single integral complementary, non-contradictory system, which can be effectively implemented, primarily due to the codification of medical legislation.
Health care is one of the branches of the state's activity, the purpose of which is to organize and provide medical services to the population, to maintain and improve the standard of living. The need to assess the effectiveness of the distribution of finances stems from the importance of the public finance reform taking place in Russia over the past ten years.
In the context of an acute shortage of resources in the health care sector, there is no multilevel system for assessing and ensuring the efficiency of the use of health care resources. At the same time, the weakening of the management base, in particular the planning function, predetermines a decrease in the level of personal responsibility of the heads of health authorities and institutions for the final results of their activities.
The most important problem of increasing the efficiency of administrative management, experts call the irrational use of funds. At the same time, delaying the solution of this problem in health care is the most expensive - at the cost of a decrease in the quality of the region's population (an increase in disability, mortality, and morbidity). Mechanisms are needed to control the spending and auditing of budgetary funds in the framework of the study of the impact of activities and their cost on the final results of the functioning of the health care system.
Traditionally, there are four main sources of financing for health care, including: receipts from general taxation, patient cash, as well as contributions to the compulsory health insurance system, contributions to the voluntary health insurance system.
In a market economy, the following models of health care financing can be distinguished:
- Budgetary - the collection of taxes, with the help of which the revenue side of the budget is formed, and then the expenditure on health care is determined.
- Insurance - targeted contributions for health insurance, can be manifested in the form of a combination of insurance and budget financing.
- Private - charity, personal contributions from citizens.
To date, the federal budget remains the only possible source of coverage for underfunding. Public funding for health care increased by 7% in 2014, in 2015 the growth was 117%, and in 2016 the overall increase is planned to be up to 20%. In absolute terms, this difference is 691 billion rubles. In 2016, government spending is projected to amount to 3.4% of GDP. Comparing healthcare spending in 2016 with 2014, the difference was 470 billion rubles in comparable prices.
It should be noted that the Government of the Russian Federation in April 2014 approved a 22% reduction in expenditures for 2 programs. Namely, adopted at the end of 2012 for the period 2013-2020: "Development of health care" and "Development of the pharmaceutical and medical industry", which includes the program "Pharma 2020", and the initial budget from 122 billion rubles. reduced to 99 billion rubles. The rest of the costs are transferred to the CHI system.
One of the problems in the distribution of finances in the field of health care is the lack of uniform maximum purchase prices for medicines and medical devices established at the federal level. Thus, according to the data of the All-Russian Popular Front (ONF), in the neighboring regions of the Russian Federation, prices for the same drugs can fluctuate from 10 to 40%. There is also a perception that public funds are not spent on priorities. For example, in 2014, more than 50 billion rubles were withdrawn from the FFOMS budget. for the construction of perinatal centers in the constituent entities of the Russian Federation. Despite the fact that in the Russian Federation, the main priorities are the health of men of working age, children and adolescents. In 2015, expenditures on high-tech medical care (HMP) in the amount of 28.6 billion rubles were financed from the budget of the FFOMS. Previously, these expenses were paid exclusively by the federal budget.
At the present stage, it is planned to pay from the FFOMS budget both the costs of the high-tech medical care and a number of investment costs, including the purchase of ambulances. The total amount of funds allocated this year from the FFOMS budget to the federal budget is about 127 billion rubles.
The consolidated budget of the Russian Federation and state extra-budgetary funds (GVBF) also play a leading role in the structure of health care expenditures. According to statistics, the volume of the consolidated budget is increasing every year, in 2016 it will amount to 2 trillion 852 billion rubles, which is 7 billion more than in 2015. A significant weight of health care expenditures in the total amount of expenditures falls on the budgets of territorial GVBFs. During 2010-2014. this figure was about 80%, which indicates that, first of all, health care is financed by the funds of the territorial GVBF.
Table 1 - The volume of state funding for health care in 2013-2016 by main expense items.
| Expenditure items, RUB bln / year | 2013 | 2014 | 2015 | 2016 | Growth rate 2016/2013,% |
| Primary health care on an outpatient basis | 520 | 573 | 613 | 636 |
122,31 |
| Emergency | 98 | 107 | 114 | 119 | 121,43 |
| Specialized inpatient care | 826 | 888 | 951 | 988 | |
| Medicines for the population on an outpatient basis | 150 | 151 | 161 | 167 |
Table 1 presents data on the items of expenditure of the most basic types of medical care for the general population.
Obviously, the largest share is occupied by the costs of specialized care in inpatient conditions, which increased by 19.6% during the study period. The smallest share is occupied by expenses for emergency medical care, which increased by 21.4%. Outpatient primary health care spending also increased by 22.3%. As for the costs of drug provision of the population on an outpatient basis, they also tend to grow, but only by 11.3%.
Also, the source of financing for health care can be the personal funds of the consumer of health services. Paid services have existed throughout the history of Russia. Every citizen had and has the right to turn to a private doctor or specialist for the necessary service. Financing of health care through personal contributions of citizens is becoming more and more significant, but it is rather difficult to estimate its volume. The funds of the population spent on the purchase of paid services account for about 1.5% of health care expenditures from all sources.
The private model is characterized by the absence of an integral health care system and access of a significant part of the population to guaranteed medical care. It should be borne in mind that different stages of medical technology require different funding structures. There are types of services where it is desirable to reduce the share of the private sector to zero. There are two points of view on this issue. Supporters of the first point of view believe that the private sector should generally not be allowed into the provision of medical services for especially dangerous infections.
In the second point of view, the private sector can operate in any area of health care. This issue, according to legal regulation, has not been resolved to date, therefore, most of the private sector for the provision of medical care is in the "shadow economy".
Most of the regional programs of state guarantees for the provision of free medical services are in short supply. In total, about 50 regions of the country are underfunded by 125 billion rubles. As a result, in most regions, the basis for planning the volume of medical care is not the actual need for it by the population, but the financial capacity of the region. To solve this problem, it is necessary to carry out the following measures:
1. a clear definition of the minimum volume of free services provided;
2. the possibility of forming a system of compulsory health insurance of several levels (basic system and additional programs with a higher contribution rate);
3. Maintaining state guarantees of primary health care at the expense of programs (with a reduction in funding for the sectors of secondary and tertiary health care).
The strategy for the development of healthcare in the Russian Federation for the long term recognizes the further development and strengthening of the private sector of the industry as the main direction of development. It is planned to increase the share of commercial medical services. Investments will be attracted from various other sources: scientific grants, subcontracts with national companies, insurance companies, and the issue of securities.
The introduction of new principles of financing, systemic transformations, as well as the introduction of advanced medical technologies and international standards for the quality of medical care as part of the formation of an innovative model is necessary in order to equalize the financial conditions for the implementation of territorial compulsory health insurance programs, taking into account the aggregate income sources of their financial support, as well as stimulate efficiency implementation of territorial programs in accordance with the legislation of the Russian Federation. Systematic work within the framework of reforming the industry and improving its financial mechanism, taking into account the advanced experience of developed countries and new management technologies, is able to bring healthcare and medical organizations funded under the territorial guarantees program at the expense of FFOMS funds to a new level of efficiency. A systematic approach to the formation of a quality system of medical services allows predicting the development trends of the main parameters of the economic state of an organization, taking into account the role in improving the efficiency of activities and management of the organization.
I... Health financing in the context
compulsory health insurance
In the former Soviet Union, health care guaranteed free and generally available medical care to citizens. In practice, financing the industry from the state budget led to a constant decrease in the share of medical expenses in the total amount of budget allocations, as a result, insufficient funding and irrational use of funds led the industry to a critical state. The sharp drop in most of the indicators characterizing the level of medical care made it obvious the need for a fundamental restructuring of domestic health care. One of the ways out of the crisis for the industry was the introduction of new forms of management, planning and financing into the health care system, beginning in the early 1990s.
Based on the analysis of the practice of financing and organizing health care in foreign countries, three basic models of the economic mechanism of health care can be distinguished:
1. Predominantly public free medical care, as, for example, in England, Denmark, Greece, Ireland.
2. Funding of the bulk of medical care by private insurance companies, for example, in the United States.
3. The mixed budgetary and insurance nature of health care financing, when targeted programs, capital investments and some other expenses are paid from the state, and the financing of basic medical care is carried out through the health insurance system: France, Germany, Italy, etc.
In the modern period, the insurance systems of medical and social assistance continue to develop. Health insurance systems are usually run by the state, but funded from three sources: earmarked contributions from employers, government subsidies, and employee contributions. In some countries, there are no government subsidies for health care payments, and health insurance premiums are provided by employers and workers.
The health insurance system is financed, like the budgetary one, from public consumption funds and is formed on a targeted basis; it is more protected from the residual financing principle that is characteristic of many budgetary health care systems. That is why in our country, in order to combine the positive aspects of public and private medicine, a budget-insurance model was chosen. On June 28, 1991, the RF Law “On Health Insurance of Citizens in the Russian Federation” was adopted, which defines a fundamentally new model of financing and organizing health care in the new economic conditions.
The law establishes two types of health insurance: compulsory and voluntary. The purpose of the introduction of compulsory health insurance was to provide all citizens of the Russian Federation with equal opportunities in obtaining medical and pharmaceutical care provided at the expense of compulsory health insurance funds in the amount of relevant programs. Voluntary health insurance allows citizens to receive additional health care services.
The economic basis of health insurance is made up of state health funds and compulsory health insurance funds. With the introduction of compulsory health insurance, the entire health care system in the Russian Federation began to represent a combination of two systems: the state (municipal) health care system and the state compulsory health insurance system.
The sources of financial resources for the healthcare system in the Russian Federation are:
Funds from the federal budget, territorial budgets of the constituent entities of the Federation, local budgets;
Funds of organizations, enterprises and other economic entities, regardless of the form of ownership;
Personal funds of citizens;
Income from securities;
Gratuitous and charitable contributions and donations;
Other sources not prohibited by the legislation of the Russian Federation.
The financial basis of the state system of compulsory health insurance is the deductions of policyholders for compulsory health insurance and budgetary payments for compulsory health insurance of the non-working population. Financial resources are accumulated in compulsory health insurance funds - federal and territorial, which are independent non-profit financial and credit institutions and created to ensure the stability of the state system of compulsory health insurance. The financial resources of the funds are not included in the budgets, other funds and are not subject to withdrawal.
Non-departmental control over the activities of health care institutions is carried out by licensing and accreditation commissions, medical insurance organizations, territorial compulsory health insurance funds, executive bodies of the Social Insurance Fund of the Russian Federation, etc. and checking the efficiency of use of health care resources and compulsory health and social insurance funds. It is carried out in the following areas:
Analysis of the results of the provision of medical care to the population,
Verification of the fulfillment of contracts between health care institutions and medical insurance organizations, between the insured and the insurer, and other types of control.
The experience of implementing the Law of the Russian Federation "On Health Insurance of Citizens in the Russian Federation" has shown the promising nature of the compulsory health insurance system and posed a number of problems, without the solution of which further development is impossible. First of all, this is insufficient legal support of the compulsory health insurance system, the need to improve the quality control system of medical care in medical institutions and the creation of a system to ensure the rights of the insured.
II... Planning and financing of activities
medical institutions
In accordance with the approved nomenclature, healthcare institutions are divided into groups:
1. Treatment-and-prophylactic institutions.
A) Outpatient clinics - when they receive help both at home and in a polyclinic (polyclinics, medical centers, dispensaries, medical assistant points, antenatal clinics, children's clinics, pharmacies, pharmaceutical factories).
B) Hospitals - when the patient receives treatment on a bed (hospitals, clinics at scientific medical institutes, military hospitals, sanatoriums, dispensaries (beds).
1.1. Hospital institutions, including: a city hospital, a city emergency hospital, a hospital for war veterans, a medical unit, specialized hospitals, a hospice, a territorial medical association.
1.2. Health care institutions of a special type: a leper colony, a center for the prevention and control of AIDS, a forensic medical examination bureau, a bureau of medical statistics.
1.3. Dispensaries: physical education, cardiology, narcological, dermatovenerological, oncological, anti-tuberculosis, neuropsychiatric.
1.4. Outpatient clinics: outpatient clinic, city polyclinic, children's city polyclinic, dental clinic, medical unit, consultative and diagnostic center for children, etc.
1.5. Ambulance and blood transfusion facilities: ambulance station, blood transfusion station.
1.6. Institutions of motherhood and childhood: children's home, maternity hospital, etc.
1.7. Sanatoriums: sanatorium, children's sanatorium, sanatorium-preventorium, etc.
2. Institutions of preventive medicine.
3. Pharmacy institutions.
The costs of maintaining health care institutions account for the largest share in health care costs. The work of each health care institution is characterized by operational-network indicators, such as: the average annual number of beds (total and by bed profiles), the number of days of bed functioning per year, the number of bed days, the average annual number of staff units for all categories of personnel, the number of medical visits.
A medical and prophylactic institution can provide medical care to the population in two forms: inpatient and outpatient. One of the main indicators of the work of the hospital is the bed capacity, and of the outpatient clinic, the number of doctor's posts and visits. Depending on this, a methodology for calculating costs is selected. In the modern period, only natural norms of expenditures for food and medicines (depending on the type of institution) have been centrally established. Calculations of the value of natural indicators are carried out by local departments independently. In an outpatient clinic, the main indicators in planning costs are: the average annual number of doctor's posts and the number of doctor's visits.
The main document that determines the total volume, target direction and quarterly distribution of the institution's funds is the cost estimate compiled for the calendar year in the prescribed form for the economic items of the budget classification. The estimate may include only the costs, the need for which is due to the nature of the activities of the institution. The appropriations provided in the estimate must be justified by calculations for each cost item. The main economic items for which the planning of the institution's costs is carried out include the costs of paying wages, purchasing goods, paying for services, purchasing durable equipment, and overhauling.