RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Archive - Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2007 (Order No. 764)
Mammary gland, unspecified part (C50.9)
general information
Short description
The most common tumor in women, classified as a classic hormone-related cancer; develops in an organ that is part of the body's reproductive system. These tumors originate from the epithelial tissue of the ducts or lobules of the mammary gland - the “target” for hormones produced by the ovaries (estrogens and progestins).
On average, about 3,000 patients with breast cancer are diagnosed annually in the Republic of Kazakhstan, of which more than 1,380 women die. In particular, in 2005, 2954 cases of breast cancer were registered, which amounted to 19.5 (32.3 in Almaty) per 100,000 population. The 1-year mortality rate is 10.8%, and the 5-year survival rate is 49.3%.
Protocol code: H-S-008 "Malignant neoplasms of the breast. Breast cancer"
Profile: surgical
Stage: hospital
ICD-10 code(s):C50 Malignant neoplasm of the breast
Classification
Histological classification of breast tumors
Currently, it is customary to use the histological classification of the International Union Against Cancer (2002, 6th edition).
| A | Non-invasive cancer (in situ): |
| Intraductal (intracanalicular) carcinoma in situ | |
| Lobular (lobular) carcinoma in situ | |
| IN | Invasive cancer (infiltrating carcinoma): |
| Ductal | |
| Lobular | |
| Mucous (mucinous) | |
| Medullary (medullary) | |
| Tubular | |
| Apocrine | |
|
Other forms (papillary, squamous, juvenile, spindle cell, pseudosarcomatous, etc.) |
|
| WITH | Special (anatomical and clinical) forms: |
| Paget's cancer | |
| Inflammatory cancer |
Most often, patients experience invasive ductal cancer (50-70%), followed by lobular cancer (20%). Ductal cancer is characterized by more frequent spread along the milk ducts, and lobular cancer is characterized by primary multiplicity and bilaterality.
INTERNATIONAL CLASSIFICATION TNM
Currently, the classification of tumors according to the TNM system of the International Union Against Cancer (2002) is used. The stage of cancer is established during the initial examination of the patient, and then clarified after surgery (pTNM).
The classification applies only to carcinomas and applies to both the male breast and the female breast.
In the case of the presence of primary multiple synchronous tumors in one mammary gland, the tumor with the highest
category T. Synchronous bilateral breast tumors should be classified independently to allow cases to be separated according to histological type.
The following methods should be used to assess categories T, N and M:
Anatomical areas:
1. Nipple (C 50.0).
2. Central part (C 50.1).
3. Upper inner quadrant (C 50.2).
4. Lower inner quadrant (C 50.3).
5. Upper outer quadrant (C 50.4).
6. Lower outer quadrant (C 50.5).
7. Axillary tail (C 50.6).
Regional lymph nodes:
1. Axillary (ipsilateral), interthoracic nodes (Rotter) and lymph nodes along the axillary vein and its branches which can be divided into the following levels:
Level I (lower part of the axillary fossa): lymph nodes located lateral to the lateral border of the pectoralis minor muscle;
Level II (middle part of the axillary fossa): lymph nodes located between the medial and lateral borders of the pectoralis minor muscle and interthoracic lymph nodes (Rotter);
Level III (apical part of the axillary fossa): apical lymph nodes and nodes located medial to the medial border of the pectoralis minor muscle, with the exception of those defined as subclavian.
Note. Intramammary lymph nodes are coded as axillary lymph nodes.
2. Subclavian (ipsilateral) lymph nodes.
3. Intramammary (ipsilateral) lymph nodes: lymph nodes in the intercostal areas along the edge of the sternum in the endothoracic fascia.
4. Supraclavicular (ipsilateral) lymph nodes.
Metastasis to any other lymph nodes is defined as distant metastases (M1), including cervical or contralateral intramammary lymph nodes.
TNM symbols mean: T - primary tumor.
| Tx | There is insufficient data to evaluate the primary tumor. |
| T0 | The tumor in the mammary gland is not detected. |
| Тis |
Preinvasive carcinoma (carcinoma in situ) Tis (DCIS) - ductal carcinoma in situ Tis (LCIS) - lobular carcinoma in situ Тis (Paget) - Paget's disease (nipple) without tumor Note: Paget's disease with the presence of a tumor is classified into according to the size of the tumor. |
| T1 | Tumor no more than 2 cm in greatest dimension |
| Т1mic |
Microinvasion up to 0.1 cm in greatest dimension Note: microinvasion is the spread of cancer cells beyond limits of basement membrane with lesions less than 0.1 cm If there are multiple foci of microinvasion, the largest one is classified according tosize of the lesion (it is impossible to summarize the sizes of microfoci) Availability multiple foci of microinvasion should be noted additionally |
| T1a | Tumor more than 0.1 cm, but not more than 0.5 cm in greatest dimension |
| Т1b | Tumor more than 0.5 cm but not more than 1 cm in greatest dimension |
| T1s | Tumor more than 1 cm but not more than 2 cm in greatest dimension |
| T2 | Tumor more than 2 cm but not more than 5 cm in greatest dimension |
| T3 | Tumor more than 5 cm in greatest dimension |
| T4 |
Tumor of any size with direct extension to the chest wall or skin Note: The chest wall includes the ribs, intercostal muscles and anteriorserratus muscle, but not pectoralis muscle |
| T4a | Spread to chest wall |
| Т4b |
Swelling (including “lemon peel”) or ulceration of the skin of the breast,or satellites in the skin of the breast |
| Т4c | Signs listed in 4a and 4b together |
| Т4d | Inflammatory form of breast cancer |
Note: Inflammatory breast carcinoma is characterized by diffuse brown induration of the skin with an erysipeloid margin, usually without an underlying mass. If skin biopsy indicates no involvement and there is no localized, detectable primary cancer, category T is pTx for pathohistological staging of inflammatory carcinoma (T4d).
Dimpled skin, nipple retraction, or other skin changes other than those found in T4b and T4d may be scored as T1, T2, or T3 without affecting the classification.
N - regional lymph nodes.
| NX | There is insufficient data to assess the condition of regional lymph nodes |
| N0 | There are no signs of metastatic lesions of regional lymph nodes |
| N1 |
Metastases in displaced axillary lymph nodes (e) on the side defeats |
|
N2 N2a N2b |
Metastasis to a fixed ipsilateral axillary lymph node (s) or in clinically obvious ipsilateral intramammary lymph node(s) In the absence of clinically obvious metastases in the axillary lymph nodes metastasis in axillary lymph node(s) linked to each other or to other structures Metastasis only in clinically obvious intramammary lymph node(s), with absence of clinically obvious metastasis in the axillary lymph node |
| N3 |
Metastasis to the ipsilateral subclavian lymph node(s) withdamage to the axillary lymph nodes or without them; or in clinically obvious ipsilateral intramammary lymph node(s) if clinically present obvious metastases in the axillary lymph nodes; or metastasis in the ipsilateralsupraclavicular lymph node(s) with or without involvement of axillary or intramammary lymph nodes |
|
N3a N3b N3с |
Metastasis in the subclavian lymph node(s) Metastases in intramammary and axillary lymph nodes |
|
Note. “Clinically obvious” means those identified as a result of clinical trial or imaging (for except for lymphoscintigraphy) |
M - distant metastases.
rTNM pathohistological classification.
pT - primary tumor.
Pathohistological classification requires examination of the primary carcinoma, in the absence of macroscopic tumor at the resection margins. A case can be classified as pT if there is only microscopic tumor at the margin.
Note. When classifying pT, tumor size is the size of the invasive component. If there is a large in situ component (eg 4 cm) and a small invasive component (eg 0.5 cm), the tumor is classified as pT1a.
рN - regional lymph nodes.
Examination of one or more sentinel lymph nodes may be undertaken for histopathological classification. If the classification is based only on sentinel node biopsy without subsequent axillary node dissection, it should be designated (sn) (sentinel node), for example: pN1 (sn).
| рN1mi | Micrometastasis (more than 0.2 mm, but not more than 2 mm in greatest dimension) |
| РN1 |
Metastases in 1-3 ipsilateral axillary lymph nodes (e) and/or ipsilateral intramammary nodes with microscopic metastasesidentified as a result of sentinel lymph node dissection, but not clinically obvious |
| рN1а |
Metastases in 1-3 axillary lymph nodes (e), among them at leastone more than 2 mm in greatest dimension |
|
рN1b рN1с |
Intramammary lymph nodes with microscopic metastases, identified as a result of sentinel lymph node dissection, but clinically not explicit Metastases in 1-3 axillary lymph nodes and intramammary lymph nodes with microscopic metastases identified as a result of dissectionsentinel lymph node, but not clinically obvious |
| рN2 |
Metastases in 4-9 ipsilateral axillary lymph nodes or in clinically obvious ipsilateral intramammary lymph nodes, with |
|
Note. “Clinically silent” means not detected by clinical examination or imaging (exceptlymphoscintigraphy); “clinically apparent” means those identified by clinical examination or imaging (except lymphoscintigraphy), or macroscopically visual. |
|
| рN2а |
Metastases in 4-9 axillary lymph nodes, including at least one larger than 2 mm |
| рN2b |
Metastasis to a clinically obvious intramammary lymph node(s) with absence of metastases in the axillary lymph nodes |
| рN3 |
Metastases in 10 or more ipsilateral axillary lymph nodes; or in ipsilateral subclavian lymph nodes; or in clinically obvious ipsilateral intramammary lymph nodes, if there is one or more affected axillary lymph nodes; or in more than 3 axillary lymph nodes with no clinically obvious microscopic metastases in intramammary lymph nodes; or in the ipsilateral supraclavicular lymph nodes |
| рN3а |
Metastasis to 10 or more axillary lymph nodes (at least one of which more than 2 mm) or metastases in the subclavian lymph nodes |
| рN3b |
Metastasis to clinically obvious intramammary lymph node(s) if presentaffected axillary lymph node(s); or metastases in more than 3 axillary lymph nodes and in intramammary lymph nodes with microscopic metastasis identified during sentinel dissection lymph node, but clinically not obvious |
| рN3с | Metastasis to the supraclavicular lymph node(s) |
rM - distant metastases. The PM categories correspond to the M categories.
G histopathological classification
G1 - high degree of differentiation.
G2 - average degree of differentiation.
G3 - low degree of differentiation.
R classification
The absence or presence of residual tumor after treatment is described by the symbol R. R classification definitions:
RX - the presence of residual tumor cannot be determined.
R0 - no residual tumor.
R1 - microscopic residual tumor.
R2 - macroscopic residual tumor.
Grouping by stages
| Stage 0 | TiS | N0 | M0 |
| Stage I | T1* | N0 | M0 |
| Stage IIA | T0 | N1 | M0 |
| T1* | N1 | M0 | |
| T2 | N0 | M0 | |
| Stage IIB | T2 | N1 | M0 |
| T3 | N0 | M0 | |
| Stage IIIA | T0 | N2 | M0 |
| T1* | N2 | M0 | |
| T2 | N2 | M0 | |
| T3 | N1, N2 | M0 | |
| Stage IIIB | T4 | N0, N1, N2 | M0 |
| Stage IIIC | any T | N3 | M0 |
| Stage IV | any T | any N | M1 |
Note. *T1 includes T1mic (microinvasion 0.1 cm or less in greatest dimension).
|
Tis T1mic T1a T1b T1c T4a T4b T4d |
in situ £ 2cm £ 0.1 cm > 0.1 to 0.5 cm > 0.5 to 1 cm > 1 to 2 cm > 2 to 5 cm > 5 cm Chest wall/skin Chest wall Skin swelling/ulceration, satellite nodules on the skin Signs characteristic of T4a and T4b Inflammatory carcinoma |
| N1 |
Movable axillary |
pN1mi pN1a pN1b pN1c |
Micrometastases, > 0.2 mm £ 2 mm 1-3 Axillary nodes Intramammary nodes with micrometastasis, identified by sentinel node biopsy, but clinically undetectable 1-3 Axillary nodes and intramammary nodes with micrometastasis detected by sentinel node biopsy, but clinically undetectable |
| N2a |
Fixed axillary |
pN2a | 4-9 Axillary nodes |
| N2b |
Intramammary- clinically defined |
pN2b |
determined without axillary nodes |
| N3a | Subclavian | рN3a |
³ 10 Axillary nodes or subclavian node(s) |
| N3b |
Intramammary- nye and axillary new |
рN3b |
Intramammary nodes, clinically identified with axillary node(s) or> 3 axillary nodes and intramammary nodes with micrometastases that are detected with a biopsy of the sentinel node (sentinel node), but clinically undetectable |
| N3c | Supraclavicular | рN3c | Supraclavicular |
Risk factors and groups
Classification of risk factors
1. Factors characterizing the functioning of the body’s reproductive system:
Menstrual function;
Sexual function;
Childbearing function;
Lactation function;
2. Hyperplastic and inflammatory diseases of the ovaries and uterus.
Endocrine-metabolic factors caused by concomitant and previous diseases:
1. Obesity.
2. Hypertension.
3. Diabetes mellitus.
4. Liver disease.
5. Atherosclerosis.
6. Diseases of the thyroid gland.
7. Dishormonal hyperplasia of the mammary glands.
Genetic factors(carriers of BRCA-1 or BRCA-2 genes):
1. Breast cancer in blood relatives (hereditary and “family” breast cancer).
2. Milk-ovarian syndrome (breast cancer and ovarian cancer in the family).
Exogenous factors:
1. Ionizing radiation.
2. Chemical carcinogens, including smoking.
3. Excessive consumption of animal fats, high-calorie diet.
4. Viruses.
5. Taking hormones.
Diagnostics
Diagnostic criteria
Complaints(no pathognomonic symptoms characteristic of breast cancer).
There may be complaints about the presence of a formation in the mammary glands, hyperemia, swelling, wrinkling, retractions or protrusions on it, narrowing of the areolar field, etc.
Anamnesis: the presence of cancer in close relatives, the onset of menstruation, the age of the first pregnancy and first birth, taking OCs or HRT, gynecological diseases.
Physical examination
1. Examination of the mammary glands.
Upon examination, determine:
Symmetrical location and shape of the mammary glands;
Level of position of the nipples and their appearance (retraction, deviation to the side);
Condition of the skin (hyperemia, swelling, wrinkling, retractions or protrusions on it, narrowing of the areolar field, etc.);
Pathological discharge from the nipple (quantity, color, duration);
The presence of swelling of the arm on the affected side.
2. Palpation of the mammary glands (in vertical and horizontal positions).
3. Palpation of regional and cervical-supraclavicular lymph nodes (usually performed in a vertical position).
Laboratory research
Laboratory tests that must be performed upon the patient’s initial visit before treatment: complete blood count, blood group, Rh factor, general urine test, biochemical blood test (urea, bilirubin, glucose), RW (Wassermann reaction), coagulogram, ECG ( electrocardiography).
Instrumental studies
X-ray diagnostics is one of the leading methods for detecting breast cancer, especially if the tumor is small and not palpable. Mammography is indicated for all patients with breast cancer.
Examination methods that must be performed by the patient before starting treatment:
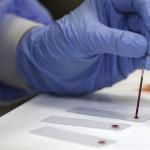
1. Puncture biopsy of the tumor with cytological examination or trephine biopsy with determination of the level of expression of ER, PR, Her-2/neu and other genetic factors.
2. Ultrasound examination of the abdominal organs.
3. X-ray examination of the lungs.
4. Osteoscintigraphy (in institutions equipped with a radioisotope laboratory).
5. Ultrasound examination of the mammary glands, regional lymph nodes.
Mammography and ultrasound complement each other because Mammography may reveal tumors that are not detected by ultrasound, and vice versa.
Morphological diagnosis:
1. Cytological (puncture) biopsy (fine needle biopsy).
2. Trephine biopsy or sectoral resection of the mammary gland.
Indications for consultation with specialists.
Mandatory: consultation with a gynecologist.
If necessary, consultation with an endocrinologist, neurologist, urologist, radiologist, chemotherapist, and other related specialists according to indications.
List of main diagnostic measures:
1. Determination of hemoglobin.
2. Counting leukocytes in the Goryaev chamber.
3. Counting red blood cells for CPK.
4. Determination of ESR.
5. Hematocrit.
6. Calculation of the leukocyte formula.
7. General urine analysis.
8. Determination of total protein.
9. Cytological examination and histological examination of tissue.
10. Determination of capillary blood clotting time.
11. Platelet count.
12. Blood test for HIV.
13. Microreaction.
14. HbsAg, Anti-HCV.
15. Determination of protein fractions.
16. Determination of bilirubin.
17. Coagulogram 1 (prothrombin time, fibrinogen, thrombin time, aPTT, plasma fibrinolytic activity, hematocrit.
18. Determination of residual nitrogen.
19. Determination of glucose.
20. Definition of ALT.
21. Definition of AST.
22. Thymol test.
23. Determination of blood group and Rh factor.
24. Ultrasound of the abdominal organs.
25. Electrocardiography.
26. Chest X-ray in two projections.
27. Ultrasound of the mammary glands.
28. Mammography.
29. Ductography.
30. Ultrasound of the pelvic organs.
31. Magnetic resonance imaging (MRI) of the breast.
32. Computed tomography (CT) of the breast.
List of additional diagnostic measures:
1. Consultation with a cardiologist.
Differential diagnosis
| Complaints |
Physical data |
Ultrasound, mammography |
Morphologicallye signs |
|
| RMJ |
Availability of education in mammary gland, hyperemia, edema, rugosity, bulges on it, |
Upon inspection, presence On palpation the presence of a tumor in the breast, increased regional lymph nodes |
Availability education in dairy gland, calcifications, increase regional lymph nodes |
Presence of cells tumors in smears. Conclusion pathologist about availability malignant tumors |
|
Inflammatory breast diseases |
Hyperemia, hyperthermia, breast pain gland, purulent discharge |
On examination there is hyperemia On palpation presence of painful seals in the breast, possible reactively sometimes enlarged lymph nodes |
The presence of a cavity with liquid content without clear boundaries |
Availability elements purulent inflammation, inflammation leukocytes, neutrophils macrophages, fibroblasts in strokes. Histologically - abscess picture, purulent infiltration |
|
Fibroadenoma, cystadenoma MJ, localized fibroadenoma toz |
Availability of education in mammary gland, pain |
Upon inspection it is possible breast deformation. presence of seal in MJ |
Availability education from clear contours, with mammography - the presence of a "rim" security" |
The presence of peri-, intracanal- cular and mixed fibroadenomas |
|
Cyst mammary gland |
Availability of soft-elastic mammary gland, pain, nipple discharge |
Upon examination possible deformation MJ. On palpation availability of education soft-elastic consistency in the breast |
Availability cavities with liquid content with clear contours |
Presence of a wall cysts, liquid contents |
Treatment abroad
Get treatment in Korea, Israel, Germany, USA
Get advice on medical tourism
Treatment
Treatment tactics
Treatment goals: achieving radical treatment.
Non-drug treatment
Breast cancer is one of the few oncological diseases for which treatment of all stages is multivariate.
Despite significant progress in the development of new methods for treating breast cancer, surgery still remains the main, and in some cases, the only method of treating this disease (Ca in situ).
The choice of one or another type of radical surgery is determined not only by the degree of spread of the tumor process, but also by the clinical form, location of the tumor, the age of the patients and some other factors characterizing their general condition.
Recently, increasing importance has been attached to improving the quality of life, which is achieved by performing organ-preserving operations on the mammary gland, as well as reconstructive operations using local tissues.
Organ-conserving operations for breast cancer provide, along with high survival rates, good cosmetic and functional results. Social and labor rehabilitation of patients after segmental resection of the mammary gland occurs faster than after mastectomy.
Indications for performing organ-preserving operations on the mammary gland:
The presence of a nodular form of cancer up to 2.5 cm in size;
Absence of multicentricity and multifocality of tumor growth (on mammograms, ultrasound, clinically);
Slow and moderate growth rates, doubling of tumor size no faster than 3 months (according to medical history);
Favorable ratio of the size of the breast and tumor to obtain a good cosmetic result of the operation;
No distant metastases;
The presence of single metastases in the axillary region is acceptable;
Reconstructive operations can be performed for stages I-III of breast cancer at the request of the patient at any tumor location.
A woman should be familiar with all types of surgical interventions.
Radiotherapy technique
Radiation therapy of the breast and areas of regional metastasis (supraclavicular, axillary) is carried out with bremsstrahlung radiation from an accelerator (6 MeV) or on gamma therapeutic devices (1.25 MeV), and for the parasternal zone - by alternating photon and electron beams or only with electron radiation up to 20 MeV depending on the depth of the chain of parasternal lymph nodes.
Irradiation of the parasternal zone with 60C o or only with a photon beam with an energy above 4 MeV is fraught with the development of post-radiation pulmonitis, mediastinitis, and pericarditis. Preoperative radiation therapy is not performed in many scientific centers around the world, with the exception of locally advanced breast cancer that is resistant to neoadjuvant chemotherapy and endocrine therapy.
Postoperative irradiation of the anterior chest wall after mastectomy or irradiation of the remaining mammary gland after radical resection is carried out with a 1.25 MeV or 6 MeV photon beam from tangential fields directed so that no more than 2 cm of lung tissue falls into the 100% isodose zone.
Tangential fields. Borders:
1. Upper - level of the sternoclavicular joint (Louis angle); if necessary, the upper border can be positioned higher to include the entire breast.
2. Medial - along the middle of the sternum.
3. Lower - 2 cm below the submammary (transitional) fold.
4. Lateral - 2 cm lateral to the palpable breast tissue, usually along the mid-axillary line.
In the postoperative period after mastectomy, the boundaries of the tangential fields are as follows:
1. Upper - corner of Louis.
2. Medial - the midline of the body.
3. Lower - at the level of the submammary fold of the opposite gland.
4. Lateral - middle axillary line.
If the localization of the postoperative scar is atypical and it is located outside the designated boundaries of the irradiation fields, additional irradiation of the scar zone is recommended with tissue coverage at least 2 cm beyond its boundaries. Such irradiation should be carried out with an electron beam or using contact radiation therapy.
Suprasubclavian field.
Irradiation of the supraclavicular and axillary lymph nodes occurs from the anterior field and the beam is tilted 10-150 to the side of the same name to avoid irradiation of the esophagus and trachea.
The upper edge of the field is at the level of the upper edge of the cricothyroid recess.
The medial border is the middle of the sternum.
Lateral border - medial edge of the humeral head; if it is necessary to irradiate the entire axilla, the lateral border should be expanded to the lateral edge of the humeral head, which should be covered with a protective block.
The lower border is in contact with the upper border of the tangential field at the level of attachment of the second rib to the sternum (Louis angle).
The larynx, esophagus, and trachea are always protected with a lead block.
The posterior axillary field is used when it is necessary to irradiate the entire axillary zone.
The medial border of the field is located 1 cm inward from the edge of the chest.
The superior border is the upper edge of the clavicle.
Lateral border - the lateral edge of the head of the humerus.
The inferior border is the same level as the inferior border of the supraclavicular field.
Parasternal field. Borders:
The medial edge is the midline of the sternum.
The lateral edge is 4-5 cm lateral to the midline.
The superior edge is the lower edge of the supraclavicular field.
The lower edge is the base of the xiphoid process of the sternum.
When irradiating several adjacent fields, the distance between the boundaries of these fields should be determined depending on the selected type of radiation energy.
The dimensions of the irradiation field are selected individually during pre-radiation preparation using ultrasound, computed tomography, and an x-ray simulator.
Standard postoperative irradiation is carried out in the usual dose fractionation mode (ROD 2 Gy, SOD 40 Gy) to the mammary gland, chest wall and areas of regional metastasis. If the institution has an electron beam, in patients undergoing segmental resection, the area of the postoperative scar (i.e., the tumor bed) can be additionally irradiated at a dose of 12 Gy.
Adjuvant therapy for breast cancer
Different subtypes of breast cancer have become clearly recognized based on genetic profile and immunohistochemical demonstration of selected targets (Sorlie, 2001; Regan, 2006). The overall treatment strategy emphasizes the primary importance of targeted therapy whenever possible, although additional less “target-specific” chemotherapy may be required.
The absolute importance of timely, accurate and reliable histopathological assessment, including target identification, has become apparent. Therefore, a close collaboration between clinicians and pathologists will provide significant improvements in long-term treatment outcomes.
Further clarification of terminology also concerned the definition of endocrine sensitivity. The three sensitivity categories described in 2005 remained essentially unchanged but were made more specific in the 2007 guidance:
1. Tumors are highly sensitive to endocrine therapy (high expression of estrogen receptors (ER) and progesterone receptors (PR) in most tumor cells).
2. Tumors that are incompletely (insufficiently) sensitive to endocrine therapy (lower expression of ER and/or PR).
3. Tumors insensitive to endocrine therapy (complete absence of both ER and PR).
The degree of endocrine sensitivity varies quantitatively and is correlated with an assessment of the risk of relapse to decide whether endocrine therapy alone will be sufficient. Although it is not possible to define an absolute threshold for high endocrine sensitivity, patients at low risk (Table 1) may be considered suitable for endocrine therapy alone, while additional chemotherapy may be required in patients also with highly endocrine-sensitive tumors in the presence of intermediate or high risk factors for relapse, as well as patients with insufficient endocrine sensitivity of the tumor.
Peritumoral vascular invasion must be extensive (ie, tumor emboli observed in 2 or more tumor blocks) to be considered at increased risk;
Some small tumors and histologic subtypes may be considered low risk despite lacking steroid hormone receptor expression (eg, medullary carcinoma, apocrine carcinoma, etc.);
The level of expression or amplification of HER2 are both risk factors and, at the same time, therapeutic targets.
The proposed algorithm (Table 2) should help in choosing the optimal therapy in the near future.
Three sensitivity categories are defined:
1. Tumors that are highly sensitive to endocrine therapy. These are tumors with high expression of both steroid hormone receptors (determined by acceptable immunohistochemical methods).
2. Insufficient sensitivity to endocrine therapy (in the 2005 classification, designated as unclear endocrine sensitivity). In these tumors, there is some expression of steroid hormone receptors, but at low levels, or lack of expression of one of the receptors: ER or PR.
3. Tumors insensitive to endocrine therapy. There is no expression of steroid hormone receptors. Although this group is clearly defined as endocrine-resistant, it includes tumors of varying phenotypes (Sorlie, 2003).
HER2 positivity
There are two technologies for determining HER2 positivity.
Immunohistochemical technique - staining (up to 3+) of more than 30% of tumor cells.
An alternative method is to determine gene amplification by the FISH method (fluorescent in situ hybridization: the ratio of HER2 gene copies to the centromeres of chromosome 17 is more than 2.2) or the CISH method (chromogenic in situ hybridization) (Wolff, 2007).
It has already been clearly shown in a number of clinical trials that the presence of overt immunohistochemical staining (HER2+++) is associated with sensitivity to trastuzumab. Theoretically, weaker staining (1+ or 2+), even in the presence of amplification, should be associated with less activity of trastuzumab. Study 9831 (Perez, 2007) evaluates this hypothesis, but more large trials of the correlation between specific biological markers and anti-HER therapy are needed.
In 2007, the Panel made minor changes to the risk classification (Table 1).
Peritumoral vascular invasion increases the risk category only if it is extensive (Colleoni, 2007). Complete absence of steroid hormone receptors and amplification or increased expression of HER2 are each considered sufficient to exclude low risk, with the exception of rare forms of tumors such as medullary or apocrine carcinoma, which usually do not contain these receptors.
As in 2005, the Panel did not accept the so-called “Qncotype Dx™ molecular approach”, “Mamma Print™ gene expression profile” as sufficiently accurate tests for determining risk category. Both methods are currently being tested in prospective clinical studies (Sparano, 2006; Bogaerts, 2006).
SPECIFIC APPROACHES TO THE CHOICE OF TREATMENT
Local and regional treatment
Surgical treatments presented at the San Gallen conference mainly focused on breast-conserving surgery, technology for detecting and removing sentinel lymph nodes in order to avoid unnecessary axillary dissection. The rationale for breast surgery in the presence of distant metastases was also presented. However, these aspects of surgical treatment were not specifically addressed by the panel.
Some issues of radiation therapy were discussed. It is agreed that the ASCO and EUSOMA guidelines can be used as practice guidelines for planning postoperative radiotherapy (Recht, 2001; Kurtz, 2002).
Modern standards of radiation therapy involve the use of a CT scanning simulator when planning radiation therapy (especially on the left half of the chest) and the use of the technique of “minimal radiation exposure” to the heart (Korreman, 2006).
There was complete agreement among experts in refusing radiation therapy after mastectomy in patients with breast cancer without regional metastases (pNO) with tumors of category T1-T2. At the same time, slightly more than half of the experts consider it advisable to carry out radiation treatment in the presence of 4 or more affected lymph nodes. Data from the Oxford EBCTCG group presented in San Antonio in December 2006 indicate the appropriateness of radiation treatment after mastectomy and in women with 1-3 lymph nodes involved.
In patients with involved lymph nodes, it is recommended to include the chest wall and supraclavicular region in the irradiation volume. Experts agreed that irradiation of the axillary region. should be avoided if complete axillary dissection is performed. Most experts prefer to avoid radiation
Therapy (even after organ-sparing surgery) in elderly patients who are planning endocrine therapy. Only a few Panel members believe that older patients should also follow the standards of radiotherapy if it is indicated.
Many other “innovations” of radiation therapy were not supported by experts: simultaneous (combined) chemo-radiation therapy, “partial” radiation therapy of only the tumor bed, shortening the duration of radiation therapy with hypofractionation. The proposal to defer endocrine therapy until the end of radiation therapy is not supported.
SYSTEMIC ADJUVANT THERAPY PROGRAM
As in 2005, the main decision was to determine acceptable targeted therapy. For highly sensitive and insufficiently sensitive tumors to endocrine therapy, the choice of hormonal treatment will depend on the patient's menopausal status. It may be difficult to determine in patients who have just received cytotoxic chemotherapy when deciding whether to prescribe aromatase inhibitors. Experts have insisted on mandatory confirmation of postmenopausal status before and during the use of aromatase inhibitors.
Other factors characterizing the body and concomitant diseases are also important when choosing treatment. For example, a history of thromboembolism precludes the use of tamoxifen. The presence of concomitant cardiac pathology may influence the choice of certain chemotherapeutic agents (anthracyclines) or the possibility of treatment with trastuzumab. The patient's age and concomitant pathology may limit the use of more intensive chemotherapy regimens. Different types of expected side effects may influence patients' preferences from one treatment strategy to another.
Endocrine therapy for postmenopausal patients
The well-proven high efficacy of third-generation aromatase inhibitors (AIs) has greatly facilitated the choice of appropriate treatment after a quarter century of fairly successful use of tamoxifen (Winer, 2005; Coates, 2007; Coombes, 2007; Goss, 2005; Howell, 2005; Jakesz, 2005). However, the majority of Panel members believe that 5 years of tamoxifen alone remains a reliable adjuvant treatment for some patients. Among the strategies for using AIs, the panel of experts expressed a clear preference for “sequential” endocrine therapy - switching to AIs after 2-3 years of tamoxifen therapy.
A significant minority of the Panel also supported the initial use of IA. And very few Panel members favored a “prospective” policy: 5 years of tamoxifen followed by an AI. For patients who have already completed 5 years of tamoxifen treatment, the Panel supports subsequent additional use of AIs, but only in patients with regional metastases. Initial (up front) use of AIs is more appropriate in patients with a high risk of relapse or with HER 2-positive breast cancer. Initial use of AIs in patients receiving SSRI antidepressants is also advisable.
The panel clearly preferred sequential rather than simultaneous administration of cytotoxic chemotherapy and endocrine therapy. The total duration of optimal adjuvant endocrine therapy can range from 5 to 10 years.
Most experts believe it is necessary to screen for ovarian suppression in younger postmenopausal women, although the timing and age for such testing remains unclear.
The panel supports the need to assess bone mineral density before prescribing AIs and the use of calcium and vitamin D and, especially, exercise to reduce the risk of bone loss and symptoms associated with AI use.
Endocrine therapy in premenopausal patients
The panel of experts unanimously accepted as the standard of adjuvant endocrine therapy for premenopausal patients with breast cancer or -
- administration of tamoxifen in combination with suppression of ovarian function or
- treatment with tamoxifen alone.
One suppression of ovarian function is considered possible if the patient plans a future pregnancy, although refusal of simultaneous treatment with tamoxifen cannot be completely justified.
The panel supports the use of a gonadotropin-releasing hormone (GHR) analogue as a means of suppressing ovarian function. A large majority of experts consider surgical oophorectomy to be an acceptable method. The method of “switching off” the ovaries depends on the type of disease and other circumstances. Most experts rejected irradiation of the ovaries to suppress them. It is important to be aware that in some patients, a single GnH analogue may not completely suppress ovarian function (Jimenz-Gordo, 2006).
Although the optimal duration of ovarian function suppression with GnRH analogues remains unclear, most experts believe that such treatment should be continued for 5 years, especially in patients with ER+ breast cancer at high risk of recurrence and/or with HER2 (+) disease (Mauriac , 2007).
Again, without sufficient evidence, most experts suggest delaying the use of GnRH analogues until chemotherapy is completed.
The use of aromatase inhibitors (AIs) as the only endocrine therapy for premenopausal breast cancer patients is considered unacceptable.
The use of AIs in the setting of ovarian function suppression is currently being tested in clinical trials.
And outside of clinical trials, such a combination (AI + GnRH analogue) is allowed if there are contraindications to the use of tamoxifen. Patients who were premenopausal at the time of diagnosis but became postmenopausal after chemotherapy or during adjuvant endocrine therapy can also receive AIs, but cessation of ovarian function should be clarified before and while receiving AIs, since such treatment usually stimulates endocrine-ovarian function
(Barroso, 2006).
CHEMOTHERAPY
Perhaps the most difficult issue when planning modern adjuvant therapy is the selection of patients with tumors that are highly or insufficiently endocrine sensitive, to whom, in addition to endocrine therapy, additional chemotherapy should be prescribed. Signs suggestive of questionable adequacy of endocrine therapy alone include relatively low expression of steroid hormone receptors, metastatic involvement of regional lymph nodes, high grade or high levels of “proliferative” markers, large tumor size, and extensive peritumoral vascular invasion. Proposed molecular genetic technologies (Oncotype DXTM, Mamma printTM) to facilitate treatment selection have not been supported by experts due to the lack of convincing evidence of their contribution to planning therapeutic approaches.
A wide range of chemotherapeutic regimens is considered acceptable, but there is little agreement on a specific “favorite.” Most experts support the use of anthracyclines in all patients, including those with HER-positive tumors.
The panel of experts considers it appropriate to include DNA-damaging drugs in patients with triple-negative tumors (ER-, PR-, HER2-) (James, 2007). Combinations of cyclophosphamide, 5-fluorouracil and anthracyclines (CAF, CEF, FEC, FAC) have broad support from the Panel, as does a combination of anthracyclines and cyclophosphamide followed by paclitaxel or docetaxel. Few Panel members supported dose-dense chemotherapy and strongly rejected high-dose chemotherapy, which requires the maintenance of peripheral blood stem cells.
In general, the Panel allows the use of “less intensive” chemotherapy (4 courses of the AC regimen or 6 courses of the CMF regimen) in patients with highly endocrine-sensitive tumors but at high risk of relapse or in patients with insufficiently endocrine-sensitive tumors and HER 2-negative disease. Other regimens are also considered suitable for this group of patients, including the CAF regimen and the combination of docetaxel with AC (TAC regimen).
Most Panel members consider shorter durations of chemotherapy (12 to 16 weeks) to be appropriate for older patients, and early initiation of such therapy is particularly important for patients with receptor-negative tumors (ER-/PR-). However, elderly patients with sufficient life expectancy should be offered standard chemotherapy. Although Panel members appreciate the value of hematopoietic factors in patients with febrile neutropenia, few support their routine use. An increased risk of acute leukemia has been reported in older patients treated with hematopoietic factors (Hershman, 2007).
However, this information does not come from randomized trials, and no such complications were noted in prospective studies.
Table 3 summarizes the treatment approaches and concepts discussed above.
In 2007, oncologists had two therapeutic targets for targeted therapy: steroid hormone receptors (ER/PR) and HER 2. In treatment planning, the risk of disease relapse plays a secondary role, although the magnitude of the risk should be taken into account in patients with endocrine-sensitive tumors when determining indications for additional chemotherapy (before endocrine therapy).
Patients with tumors that are highly sensitive to endocrine therapy, especially in the absence of other unfavorable prognostic features (low and intermediate risk of relapse, HER2-), may successfully receive endocrine therapy alone, while those at high risk of relapse may require additional chemotherapy.
Decisions about additional chemotherapy should be based on an assessment of the degree of endocrine sensitivity of the tumor, risk factors, and patient preferences. Experts emphasize that there are no absolute rules when justifying treatment decisions, which remain the subject of discussion between the patient and the attending physician.
Preoperative systemic therapy
Clinically, one often encounters a difficult choice of treatment for patients with locally advanced breast cancer. The proportion of such tumors ranges from 5% to 40%. The rationale for prescribing neoadjuvant systemic therapy for MIBC is:
1. High probability of latent (micrometastatic) spread.
2. The ability to reduce the volume of surgical intervention within the “clean” surgical margins.
3. The ability to evaluate the clinical response to therapy in vivo.
4. Availability of accurate pathomorphological assessment of the degree of tumor regression.
5. Possibility of special studies of biopsy tumor material before, during and after completion of primary systemic treatment.
The goals of this type of systemic treatment are:
1. Achieve tumor regression and carry out radical local-regional treatment.
2. Taking into account the extremely unfavorable prognosis in this group of patients, using systemic therapy to improve long-term treatment results.
Scheme of neoadjuvant systemic treatment:
Mammography, ultrasound, trephine biopsy with determination of the level of ER, PR, Her 2/neu. 4 courses of neoadjuvant chemotherapy - surgery - 4 courses of adjuvant chemotherapy. If there is no effect after 4 courses of neoadjuvant chemotherapy, it is necessary to change the chemotherapy regimen.
Based on the already routine use of such treatment for large tumors, the majority of Panel members supported the use of preoperative systemic therapy (including chemotherapy and/or endocrine therapy for ER+ tumors) to improve surgical treatment, including breast-conserving treatment of breast cancer (Kaufmann, 2006; Semiglazov, 2007 ) Evaluation of the magnitude of response to neoadjuvant treatment may serve (in the opinion of some Panel members) as the basis for prescribing the same treatment in adjuvant regimens. The majority of Panel members also supported the inclusion of trastuzumab in preoperative treatment programs for patients with HER 2-positive breast cancer.
Table 1. Determination of risk categories in patients with operable forms of breast cancer. San Gallen, 2007.
| Risk category | |
| Low risk |
Absence of affected lymph nodes (p NO) and all the following signs: p T ≤2 cm and degree of malignancy (G 1) and Expression of ER and PR and No increased expression or amplification of HER 2/neu Age≥35 years |
| Intermediate risk |
Absence of affected lymph nodes (p NO) and at least at least one of the following: p T> 2 cm or Presence of extensive peritumoral vascular invasion or Increased expression or amplification of HER 2/neu Age< 35 лет |
|
Presence of single regional metastases (1-3 involved l/u) Expression of ER+ /PR+, No increased expression or amplification of HER2/neu |
|
| High risk |
The presence of single regional metastases (1-3 involved lymph nodes and lack of expression of steroid hormone receptors (ER-PR-) or |
| Presence of 4 or more affected lymph nodes |
Table 2. Planning for adjuvant treatment of breast cancer. San Gallen, 2007.
|
Highly sensitive to endocrine therapy |
Not enough endocrine sensitive |
Insensitive to endocrine therapy |
|
| HER (-) |
Endocrine therapy, additionally chemotherapy for high risk groups relapse |
Endocrine therapy, additionally chemotherapy for intermediate and high risk of relapse |
Chemotherapy |
| HER (+++) |
Endocrine therapy + trastuzumab+* Chemotherapy** |
Endocrine therapy + Trastuzumab + Chemotherapy |
Trastuzumab + Chemotherapy |
*Trastuzumab (Herceptin®) is not considered a standard of care in women with tumors smaller than 1 cm and without metastatic lymph nodes (pNO), especially in women with highly endocrine-sensitive tumors.
**Available clinical trial data do not support the recommendation of trastuzumab without prior or concomitant chemotherapy.
Table 3. Adjuvant treatment depending on therapeutic targets and risk categories. San Gallen, 2007.
| HER 2 (-) | HER 2 (+++) | |||||||||||
|
High endocrine feels. |
Incomplete feelings. To endocrine |
Insensible To endocrine therapy |
High endocrine feels |
Incomplete feelings. To endocrine |
Insensible To endocrine therapy |
|||||||
| Low risk | uh | uh | uh | uh | ||||||||
|
Prome- creepy ny risk |
x→ |
x→ |
x→ uh |
x→ uh |
x | x |
x→ e+t |
x→ e+t |
x→ e+t |
x→ e+t |
x+t | x+t |
|
x→ |
x→ |
X→ |
X→ EE |
X→ EE |
x |
x→ e+t |
x→ e+t |
x→ e+t |
x→ e+t |
x+t | x+t | |
| High risk |
heh |
heh |
heh |
heh |
x+t | x+t | ||||||
|
x→e |
x→e | x→e | x→e | X | X |
x→ e+t |
x→ e+t |
x→ e+t |
x→ e+t |
x+t x+t |
x+t x+t |
|
X-chemotherapy
E- Endocrine therapy
T-trastuzumab (Herceptin)
Adjuvant treatment of breast cancer patients in accordance with sensitivity to endocrine therapy
AI - aromatase inhibitors
CT - chemotherapy
There - Tamoxifen
SOF - suppression of ovarian function (surgery, radiation therapy,
Conservative)
AC - anthracycline + cyclophosphamide
CEF, FEC - cyclophosphamide + epirubicin + 5-fluorouracil
CAF - anthracycline + cyclophosphamide + 5-fluorouracil
Tah - taxanes
Let - letrazole
EXE - exemestane
Ana - anastrazole
TREATMENT FOR DIFFERENT STAGES OF BC
0, stage I
1. Organ-preserving treatment.
After organ-conserving surgery, taking into account the level of expression of ER, PR, Her-2/neu, one of the types of systemic treatment is prescribed. If there is no need for systemic treatment, radiation therapy may be prescribed. Irradiation of the mammary gland is carried out using photon radiation (6 MeV) from a linear accelerator or gamma radiation from a 60Co installation (1.25 MeV) from two tangentially located fields, aimed at ensuring the most homogeneous irradiation of the gland. ROD 2 Gy, SOD 60 Gy. The postoperative area is additionally irradiated at a dose of 12 Gy (2 Gy each). Electron trigger irradiation is preferred.
2. Radical mastectomy.
For all of the above localizations of stage I of the disease, it is possible to perform a radical mastectomy with restoration of the shape of the gland or without restoration (at the patient’s request).
Systemic treatment includes: chemotherapy in patients under 50 years of age with invasive forms, hormone therapy with tamoxifen in postmenopausal patients with receptor-positive tumors for 5 years. Patients under 50 years of age with preserved menstrual function: bilateral oophorectomy or LHRH analogues monthly for 2 years while taking tamoxifen.
Patients with negative ER, PR - PCT (CMF or CAF) do not undergo hormone therapy.
Chemotherapy regimens for stages 0 and I:
CMF Bonadonna regimen
Methotrexate 40 mg/m*2 IV 1 day.
5FU 600 mg/m*2 IV 1 day.
Repeat every 3 weeks for 6 cycles
Cyclophosphamide 100 mg/m*2 orally for 1-14 days.
5FU 600 mg/m*2 IV 1 and 8 days.
Prednisolone 40 mg/m*2 orally 1 and 14 days.
Repeat every 4 weeks for 6 cycles.
Doxorubicin 60 mg/m*2 IV 1 day.
Cyclophosphamide 600 mg/m*2 IV 1 day.
Stage II
Treatment is identical to that for stage I, however, in patients with N0, but with the presence of unfavorable prognostic signs (age under 35 years, negative hormonal receptors, positive Her 2-neu status) in the postoperative period, except for the entire breast, when the tumor is localized in internal quadrants or central zone, as well as in all patients with N+ (with metastatic lesions of three or fewer axillary lymph nodes), the parasternal and supraclavicular zones from the side of the main lesion are additionally irradiated.
Postoperative RT is carried out in the classical dose fractionation mode (ROD 2 Gy, SOD 30 Gy) after performing organ-sparing surgery and systemic therapy. The postoperative area is additionally irradiated at a dose of 12 Gy (2 Gy each).
In patients with N+, when four or more axillary lymph nodes are affected and/or when the tumor invades the capsule of the lymph node, in addition to the remaining mammary gland, the parasternal, suprasubclavian-axillary zone on the affected side is irradiated.
ALL stage II patients should receive adjuvant systemic chemotherapy (CMF, AC, TAC, AC+T, FAC, CAF, FEC, A+ CMF).
With +ER tamoxifen for 5 years.
For -ER - chemotherapy.
For patients with positive Her 2-neu - trastuzumab 8 mg/kg on 1 day, every 21 days 4 mg/kg
Chemotherapy regimens:
cyclophosphamide 100 mg/m*2 orally for 1-14 days.
5FU 600 mg/m*2 IV 1 and 8 days.
repeat every 28 days.
methotrexate 40 mg/m*2 intravenously on days 1 and 8.
5FU 600 mg/m*2 IV 1 and 8 days.
repeat every 28 days.
repeat every 21-28 days.
5FU 500 mg/m*2 IV 1 and 8 days.
doxorubicin 50 mg/m*2 IV continuous infusion 72 hours 1-3 days.
cyclophosphamide 500 mg/m*2 IV 1 day.
repeat 21 if hematological parameters are restored.
Taxotere 75 mg/m*2 IV 1 day.
Doxorubicin 50 mg/m*2 IV 1 day.
Cyclophosphamide 500 mg/m*2 IV 1 day.
repeat every 21 days.
Cyclophosphamide 600 mg/m*2 IV 1 day.
5FU 600 mg/m*2 IV 1 day.
Repeat every 21-28 days.
Doxorubicin 60 mg/m*2 IV 1 day.
Cyclophosphamide 600 mg/m*2 IV 1 day.
Repeat every 3-4 weeks depending on the recovery of hematological parameters.
doxorubicin 60 mg/m*2 IV 1 day.
cyclophosphamide 600 mg/m*2 IV 1 day. X 4 cycles.
continue paclitaxel 175 mg/m*2 IV for a 3-hour infusion once every 3 weeks for 4 cycles.
Doxorubicin 60 mg/m*2 IV 1 day.
Cyclophosphamide 600 mg/m*2 IV 1 day x 4 cycles.
Continue docetaxel 75 mg/m*2 IV once every 3 weeks for 4 cycles.
Cyclophosphamide 75 mg/m*2 orally for 1-14 days.
Epirubicin 60 mg/m*2 IV 1 day.
5FU 500 mg/m*2 IV 1 and 8 days. every month 6 cycles.
Doxorubicin 75 mg/m*2 IV 1 day every 3 weeks for 4 cycles.
Cyclophosphamide 600 mg/m*2 IV 1 day.
Methotrexate 40 mg/m*2 IV 1 and 8 days.
5FU 600 mg/m*2 IV 1 and 8 days.
Repeat 8 cycles every 3 weeks.
In stage IIA, general effects are prescribed in accordance with table. 4.
Table 4. Absence of metastases in axillary lymph nodes
|
Menstrual status |
Low risk |
Intermediate and high risk |
|
Hormone-sensitive tumors |
||
|
Menstruating |
Tamoxifen zoladex or diferelin |
Chemotherapy chemotherapy + tamoxifen (if turning off ovarian function) |
|
Postmenopause |
Tamoxifen IA |
Tamoxifen or chemotherapy + Tamoxifen or AI |
|
Hormone-resistant tumors |
||
|
Menstruating |
Chemotherapy |
|
|
Postmenopause |
Chemotherapy |
|
Patients with positive Her 2-neu - trastuzumab 8 mg/kg on 1 day, every 21 days 4 mg/kg for 1 year. In patients of reproductive age with ER (-) and PR (-) status in combination with PCT (taxanes or SMF, excluding anthracyclines). In postmenopausal patients with ER(+) and PR(+) status in combination with IA, with ER(-) and PR(-) status it is necessary to carry out therapy in combination with PCT (taxanes or SMF, excluding anthracyclines).
In premenopausal women with 8 or more metastatic lymph nodes after completion of 6 courses of chemotherapy and ongoing menstrual function, bilateral oophorectomy or switching off ovarian function by prescribing LHH releasing hormone agonists (giserelin - 3.6 mg subcutaneously in the abdominal wall every 28 days) is indicated for 2 years, triptorelin 3.75 mg every 28 days for 2 years) while taking tamoxifen 20 mg per day for 5 years. If menstrual function ceases after 6 courses of PCT, tamoxifen 20 mg per day is prescribed for 5 years.

Patients with positive Her 2-neu - trastuzumab 8 mg/kg on 1 day, every 21 days 4 mg/kg, for 1 year. In patients of reproductive age with ER (-) and PR (-) status in combination with PCT (taxanes or SMF, excluding anthracyclines). In postmenopausal patients with ER(+) and PR(+) status in combination with IA, with ER(-) and PR(-) status it is necessary to carry out therapy in combination with PCT (taxanes or SMF, excluding anthracyclines).
Surgery 3 weeks after the end of treatment in the scope of RME according to Maden, radical resection of the mammary gland, organ-preserving or reconstructive plastic surgery.
Surgical treatment. The surgical procedure is performed according to the generally accepted method in the scope of radical mastectomy (according to Madden, Patey). The extent of surgical intervention (mastectomy option) is determined by the extent of the tumor process. In all cases, removal of regional lymph nodes of three levels is indicated: axillary, subclavian, subscapular with their subsequent marking. The tumor must be marked according to size and location in the quadrants of the mammary gland.
It is possible to perform immediate or delayed reconstructive surgery (at the patient’s request).
Postoperative radiotherapy. Postoperative RT is carried out in a classical dose fractionation mode (ROD 2 Gy, SOD up to an equivalent dose of 60 Gy). Irradiation fields: supraclavicular, axillary, parasternal, chest wall (at рТ3, 4). 61. Red blood cell cytological or histological verification of diagnosis, general blood test (6 indicators), general urinalysis, blood for chemistry (9 indicators), blood for coagulogram, electrocardiography, fluorography or R-graphy of the lungs, ultrasound mammary glands, regional zones, liver, pelvic organs, mammography. Ductography, magnetic resonance imaging, computed tomography of the mammary glands, determination of hormone levels (ER -, ER +, Her-2-neu), apoptosis, CA15-3 if possible and according to indications.
Information
Sources and literature
- Protocols for diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 764 of December 28, 2007)
- 1. V.F. Semiglazov, V.V. Semiglazov, K.Sh. Nurgaziev. Justification of standards for the treatment of breast cancer., 362 pp., Almaty, 2007. 1. Barroso G, Menqcal g. Felix H. Roias-Ruis J.C. et al. Comparison of the efficacy of the aromatase inhibitor letrozole and clomiphene citrate as adjuvants to recombinant folliclestimulating hormone in controlled ovarian hyperstimulation: a prospective, randomized, blinded clinical trial. //Fertil Steril .- 2006.- Vol 86p.1428-1431 2. Bogaerts J, Cardoso F, Buyse M, et al. Gene signature evaluation as a prognostic tool: challenges in the design of the MINDACT trial.//Nat Clin Pract Oncol .-2006.- Vol .3: p.540-551 3. Clarke CA, Glaser SL. Recent declines in hormone therapy utilization and breast cancer incidence: clinical and population-based evidence. // J Clin Oncol.-2006.-Vol.24.p 49 4. Coates AS, Keshaviah A, fthurlimann B, et al. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1-98 // J Clin Oncol .-2007 -Vol. 25 p.486-492 5. Colleoni M, Rotrnensz N, Peruzzotti G, et al. Prognostic role of the extent of peritumoral vascular invasion in-operable breast cancer. Ann Oncol .-2007 (accepted for publication) 6. Coombes RC, Kilburn LS, Snowdon CF, et al. Survival and safety of exemestane versus tamoxifen after 2-3 years" tamoxifen treatment (Intergroup Exemestane Study): a randomized controlled trial. // Lancet.- 2007.- Vol.349.p.1110-1117 7. Goldhirsch A, Glick JH , Gelber RD et al. Meeting highlights: international expert consensus on the primary therapy of early breast cancer.//Ann Oncol.-2005.-Vol.16.p.1569-1583 8. Goldhirsch A; Cda^es AS, Gelber RD et al. First-select the target: better choice of adjuvant treatments for breast cancer patients. // Ann Oncol.-2006.-Vol. 17 p.1772-1776 9. Goss PE, Ingle JNJ Martino S, et al. Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. // JNCI Cancer Spectrum.-2005.- Vol.97.p.1262-1271 10. Howell A, Cuzick J, Baum M, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years" adjuvant treatment for breast cancer. // Lancet.- 2005.- Vol 365.p.60-62 11. Jakesz R, Jonat W, Gnant M, et al. Switching of postmenopausal women with endocrine responsive early breast cancer to anastrozole after 2 years" adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trial. // Lancet.- 2005.- Vol 366.p.455-462 12. James CR, Ouinn JE, Mullan PB et al. BRCA1, a Potential predictive biomarker in the treatment of breast cancer //Oncologist.-2007.-Vol. 2.p. 142-150 13. Jimenez-Gordo AM. De Las Heras B. Zamora P. et al.: Failure of Goserelin ovarian* ablation in premenopausal women with breast cancer: two case reports. //Gynecol Oncol .- 2000. - Vol 76 p.126-127 14. Joensuu H, Kellokumpu-Lehtinen PL, Bono P, et al. Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. // N Engl J Med .- 2006.- Vol 354. p.809-820 15. Kaufmann M, Hortobigyi GN, Goldhirsch A, : et al. Recommendations from an international expert panel on the use of neoadjuvant (primary) systemic treatment of operable breast cancer: an update // J Clin Oncol .- 2006.-Vol 24p.1940-1949 16. Korreman SS. Pedefsen AN. Aarup LR et"al. Reduction of cardiac and pulmonary complication probabilities after breathingadapted radiotehrapv for breast cancer. Int J Radiot //Oncol Biol Phvs.-2006.- Vol 65.p.1375-1380 17. Kurtz J. EUSOMA Working Party. The curative role of radiotherapy in the treatment of operable breast cancer. //Eur J Cancer.-2002.- Vol 38.p.1961-1974 18. Mauriac L, Keshaviah A. Debled M Mouridsen H et al. Determinants of early relapse in postmenopausal women with hormone receptor-positive breast cancer in the BIG 1-98 trial//Ann Oncol.- 2007.- Vol. 14 p.320-327 19. Perez EA. Combining adjuvant chemotherapy with biological therapy. St. Gallen. .- //Breast.-2007 .- Vol.16 (Suppl): p105-111 20. Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al. Trastuzumab after Adjuvant Chemotherapy in HER2-Positive Breast Cancer. // N Engl J Medi -2005.-Vol.353p.1659-1672, 21. Recht A. Edge SB. Splin LJ. Robinson PSet al. Postmastectomy radiotherapy: "clinical practice guidelines of, the American Society of Clinical Oncology//. J Clin Oncology. - 2001 - Vol 19.p.1539-69 22. Regan MM, Viale G, Mastropasqua MG, et al. Re-evaluating adjuvant breast cancer trials: assessing hormone receptor status by immunohistochemical versus extraction assays. //JNCI Cancer Spectrum.-2006-Vol. 98 p.1571-1581 23. Romond EH, Perez EA, Bryant J et al. Trastuzumab plus Adjuvant Chemotherapy for Operable HER2-Positive Breast Cancer. // N Engl J Med.-2005.-Vol. 353 p.1673-1684 24. Semiglazov V.F., Semiglazov V.V. Dashyan G.A. et.al. Phase 2 Randomized trial of primary endocrine therapy versus chemotherapy in postmenopausal patients with estrogen receptor-positive breast cancer// Cancer. -2007-Vol 110.-p. 244-254 25. Slamon D, BCIRG 006 II interim analysis. San Antonio Breast Cancer Symposium, 2006. http://www.bcirg.org/Internet/BCIRG+at+SABCS+2006/default.htm 26. Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. // Proc Natl Acad Sci U S A .- 2003.- Vol.100p.8418-8423 27. Sorlie T., Perou CM, Tibshirani R et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. // Proc Natl Acad Sci U S A .-2001.- Vol. 98 p. 10869-10874 28. Sparano JA. TAILOR: trial assigning individualized options for treatment. // Clin Breast Cancer. - 2006. - Vol. 7: p347-350 29. Winer EP, Hudis C, Burstein HJ, et al. American Society of Clinical Oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. //J Clin Oncol.- 2005.- Vol 23: p.619-629. 30. Wolff AC, Hammond ME, Schwartz JN, et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer // Arch Pathol Lab Med.-2007.- Vol.131p.18.
Information
Mukhambetov S.M., Oncology Research Center
Attached files
Attention!
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications "MedElement", "Lekar Pro", "Dariger Pro", "Diseases: Therapist's Guide" cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications "MedElement", "Lekar Pro", "Dariger Pro", "Diseases: Therapist's Directory" are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
ICD-10 was introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
With changes and additions from WHO.
Benign breast conditions - description.
Short description
With benign conditions of the mammary gland, there are often complaints of pain, discomfort, and there may be some formation in the tissues of the gland or discharge from the nipple. The mammary gland is a physiologically dynamic structure with constant cyclical changes in the processes of proliferation and involution. The changes that occur can be so pronounced that they go beyond the concept of “norm”. Therefore, dishormonal diseases are often classified as aberrations of normal development and involution - ANDI (aberration of normal development and involution). The diseases themselves include the most pronounced forms of such deviations. The interpretation of the extent of these disorders depends on both the physician and the patient.
Mastodynia (mastalgia, Cooper's disease) - pain in the mammary gland. In premenopausal women, mastodynia can manifest itself as a feeling of discomfort that occurs before menstruation. The presumable cause is cyclic engorgement of the glands, caused by venous stagnation and swelling of the stroma before menstruation; at this time, the mammary gland increases in volume by more than 15%. Therapy is carried out simultaneously with the treatment of premenstrual syndrome. NSAIDs, diuretics, norethisterone, episterone or bromocriptine are prescribed.
Fibroadenoma is the most commonly detected tumor (a disorder of the development of breast lobules rather than a true tumor) of the breast, especially at a young age. Fibroadenoma consists of connective and proliferating epithelial tissue.
Diagnosis Fibroadenoma is a dense, well-circumscribed, mobile tumor with slow growth. During pregnancy, ultrasound scans often increase in size. Clear, smooth edges, height to width ratio less than 1, homogeneous structure. The mass is hypoechoic, with acoustic enhancement behind it. There may be a one- or two-sided lateral acoustic shadow. Compression does not affect the internal echo structure and can lead to a change in shape (flattening of the tumor image) Mammography. Because fibroadenomas most often occur in young women, routine mammography is not indicated. In older women, it is visible on photographs as a single, uniformly dense formation that does not disrupt the structure of the mammary gland. With age, fibroadenoma can calcify. Calcification usually begins from the center and can involve the entire fibroadenoma. The presence of large calcifications that have the appearance of “puffed corn” is characteristic. In the cytological material, there are usually few cells; bare nuclei are determined. Cellular proliferation may be pronounced, but this has no prognostic significance.
Treatment is usually surgical. For small tumors deep in the tissue (ultrasound or mammography data) or for multiple fibroadenomas - observation; if the diagnosis is questionable - excisional biopsy. The probability of fibroadenoma malignancy does not exceed 1%.
Leaf-shaped (phylloid) fibroadenoma is characterized by its large size, polycyclic contours, and rapid growth. It may degenerate into sarcoma (in about 10% of cases). Ultrasound: picture of fibroadenoma. Mammography: usually lobulated, dense formation with clear, smooth edges. Cytology: a large amount of cellular contents, cell atypia. Surgical treatment is required. If excision is incomplete, it recurs.
Hamartoma (fibroadenolipoma) is a malformation of breast tissue in the form of an isolated (outside the anatomical structure) island of normal tissue. More often they are asymptomatic. On palpation - a separate, often dense, mobile formation. Mammography: well-defined mass containing both fat and glandular tissue. A thin, X-ray negative line (pseudocapsule) is visible surrounding at least part of the mass. Diagnosis is usually made by characteristic x-ray findings. Surgical treatment is indicated for differential diagnosis or at the request of the patient (cosmetic defect).
Mastopathy (dishormonal diseases of the breast). Mastopathy is characterized by a wide range of proliferative and regressive changes in gland tissue with a violation of the ratio of epithelial and connective tissue components. The main link in pathogenesis is a violation of hormonal regulation. Proliferative changes include hyperplasia, proliferation of lobules, ducts, connective tissue, and regressive changes include atrophy, fibrosis, and cyst formation.
Frequency. Mastopathy occurs in 30–40% of women of childbearing age (most often at the age of 40 years, the frequency gradually decreases with age).
Pathogenesis. The main reason is a hormonal imbalance in a woman’s body, caused by various pathological conditions that need to be identified for adequate treatment. An increase in estrogen levels (absolute or relative) causes hyperplasia of the ductal part of the gland with the development of cystic changes. An increased content of progestins causes the development of adenous structures (glandular hyperplasia, involving acini of the lobules) with the occurrence of pain. An increase in prolactin levels leads to the development of galactorrhea and galactoophoritis, impaired LH secretion (insufficiency), resulting in amenorrhea caused by impaired progesterone production. An increase in the level of prolactin in the blood, as a rule, is accompanied by an increase in the level of estriol and estradiol. Equally important is a disruption of the biological rhythm of hormone secretion, which is inherent in a normally functioning neuroendocrine system. When the rhythm of hormone secretion and their ratios are disrupted, the effect of some hormones is longer and the effect of others is insufficient, which leads to a change in the normal cyclic processes in the mammary gland.
Classification Diffuse With a predominance of the glandular component (adenosis) With a predominance of the fibrous component With a predominance of the cystic component Mixed form Nodular fibroadenomatosis.
Clinical picture. The main complaint is a dull aching pain, giving a feeling of fullness and heaviness, which intensifies in the premenstrual period (in 85–90% of women). Painful areas of compaction in the breast tissue are identified (in all) Mastopathy with a predominance of the glandular component (hyperplasia of the gland lobules) is manifested by pain, engorgement and diffuse compaction of the entire gland or its section, often with the presence of pronounced “graininess” of the tissue. The boundaries of the compaction smoothly blend into the surrounding tissue. Manifestations intensify in the premenstrual period. More often observed at the end of puberty, as well as in women in the early stages of pregnancy (as a transient condition). The radiograph shows multiple shadows of irregular shape with unclear boundaries. Mastopathy with a predominance of fibrosis - fibrosis of the interlobular connective tissue, proliferation of intraductal tissue and narrowing of the lumen of the gland duct up to complete obliteration. It manifests itself as pain; upon palpation, dense, heavy areas are determined. Mastopathy with a predominance of the cystic component is manifested by pain, intensifying before menstruation, the presence of multiple elastic tumor-like formations (cysts are formed from atrophied lobules and dilated ducts of the mammary gland) with clear contours. Mammogram and ultrasound: multiple round formations with clear contours Mixed form - hyperplasia of the lobules, sclerosis of intralobular and interlobular connective tissue and atrophy of the alveoli with expansion of the ducts and their transformation into cystic formations Nodular form. Changes are local in nature (single or multiple nodes). Upon palpation, individual compactions are determined without clear boundaries, not fused to the skin, and may vary depending on the menstrual cycle.
The diagnosis is established on the basis of anamnesis, clinical picture, palpation of the mammary glands and is confirmed by the results of ultrasound, puncture biopsy or aspiration of the contents of the cysts. Mammography is used only as a method of differential diagnosis with tumors or as a screening examination. An isolated determination of hormone levels in the blood is ineffective; to clarify the nature of the disease, a colpocytological study is more justified.
Diet: food regimen excluding methylxanthines - tea, coffee, chocolate.
Treatment is conservative, taking into account the type of hormonal disorders and the causes that caused them, which poses certain difficulties in connection with the multifactorial regulation of the functional state of the mammary gland. Microdoses of iodine and vitamins are usually used; gestagens (derivatives of norethisterone and progesterone), antiprolactin drugs (bromocriptine), androgens (testosterone derivatives) Surgical treatment of focal forms is ineffective, since endogenous factors that contribute to relapse remain.
Observation is carried out until the formations completely disappear. Excisional biopsy is indicated for nodular fibroadenomatosis and suspected malignancy (after a full range of examinations: ultrasound, mammography, fine-needle aspiration biopsy).
Risk of malignancy. 70–90% of mastopathy (diffuse forms) are not accompanied by an increased risk of developing breast cancer. In cases of atypical epithelial hyperplasia (as determined by fine-needle aspiration biopsy), the risk of developing carcinoma is 3-6 times higher than in the general population. If atypical cells are detected and there is a family history of breast cancer, the risk is 10–15 times higher.
Intraductal papillomas are papillary epithelial growths that grow in the expanded spaces of the mammary gland ducts. This is one of the most common causes of nipple discharge. More often, abundant spontaneous serous discharge occurs, less often bloody discharge. Multiple papillomas are regarded as obligate precancer.
The diagnosis is made on the basis of the clinical picture, ductography (mammography with the introduction of a contrast agent into the affected duct of the gland), cytological examination (presence of papillary structures). Cytological examination and mammography are mandatory, since malignant neoplasms are also characterized by bloody discharge from the nipple (especially with intraductal growth). The presence of scattered microcalcifications in the papilloma area indicates a more likely presence of cancer. With ultrasound, papillomas can be detected due to the expansion and overflow of the affected duct.
Surgical treatment is excision of the affected duct. Before surgery, it is necessary to perform chromoductography.
Fat necrosis of the mammary gland (lipogranuloma) is aseptic necrosis of adipose tissue. Possible causes: injury, excessive exercise, surgery, injections.
Clinical picture. Palpation reveals a formation, sometimes fused to the skin (possible retraction of the nipple). The skin color is usually normal. The X-ray picture initially resembles that of malignant tumors. Later, the focus of necrosis calcifies (usually a spherical “eggshell” type calcification is formed), which makes it possible to confirm the non-cancerous nature of the process. Fine-needle aspiration biopsy is uninformative (no cellular material). Diagnosis is facilitated by a history of trauma, which however does not exclude the possibility of cancer.
Treatment (taking into account the difficulties in differential diagnosis) is surgical.
Mondor's disease (thoraco - epigastric thrombophlebitis) is a thrombosed vein, defined as a cord under the skin from the breast to the axillary region or to the navel. The main reason is injury, incl. and operating room. The diagnosis is easy to establish with a routine examination. Treatment. Local heat, analgesics (possibly using NSAIDs). Anticoagulants are not indicated.
A galactocele is a simple cyst filled with milk. Aspiration is a diagnostic and therapeutic measure. In case of recurrence, repeated punctures with aspiration are indicated; resection is rarely performed.
Subareolar abscess (plasmatic mastitis) most often occurs in adolescents in the post-pubertal period and in women 35–40 years old (more often in smokers). The main reason is inflammation of the additional glands located under the areola (tubercles of Morgagni). As a result of inflammation, an abscess is formed, which opens along the edge of the areola with the formation of a fistula. Subsequently, fibrosis develops between the nipple and the edge of the areola, and the nipple retracts.
Clinical picture. In adolescents, suddenly (usually after hypothermia) a painful compaction appears along the edge of the areola or under the nipple, the skin over it is hyperemic (in adults in the initial stages, often the only manifestation of the disease is discharge from the nipple), later multiple foci of abscess formation may occur with the formation of fistulas along the edge areola, nipple retraction (you must remember that sometimes cancer can occur this way).
Treatment. Acute stage - antibiotic therapy, dimethyl sulfoxide solution (1:5) locally, puncture of the abscess with aspiration of the contents (if the puncture is ineffective - surgical drainage of the abscess cavity). The remission stage is surgical treatment with excision of fistulas and all dilated ducts.
ICD-10 N60 Benign breast dysplasia
ICD code 10 fibroadenoma of the mammary gland
This component of hyperplastic syndrome includes a wide range of pathological changes in epithelial, stromal and other tissues (changes in adipocytes, vascular structures) in the mammary glands, united by the general concept of “fibroadenomatosis” or “mastopathy”. It should be noted that the classification and analysis of this type of HS (hyperplastic syndrome) is very difficult and contradictory due to the lack of clear clinical and morphological criteria to distinguish between physiological and pathological changes in the mammary glands. This leads to numerous conflicting conclusions about the possible connection between benign changes in the mammary glands and the subsequent development of malignant neoplasms in them.
The first attempts to classify hyperplastic changes in the mammary glands were based on purely clinical signs, when palpable formations were divided into diffuse forms (mastopathy) and nodular (nodose) - adenoma, fibroadenoma. According to the definition of GS in relation to the mammary glands, adopted by WHO (1984), mastopathy is a disease characterized by a wide range of proliferative and regressive changes in mammary gland tissue with an impaired ratio of epithelial and connective tissue components.
In accordance with the latest revision of the International Statistical Classification of Diseases (ICD-10), several variants of the disease have been identified, which are presented in Table. 4.3.
Classification of benign mammary dysplasia (according to ICD-10)
It should be noted that accurate statistical data on the incidence of FAM (fibroadenomatosis) are not available due to the lack of uniform diagnostic criteria and a clear pathogenetic classification of the disease. At the same time, a very rough estimate of the frequency of FAM (fibroadenomatosis) of the mammary glands indicates a significant spread of the disease. Thus, it is believed that in the premenopausal period, fibroadenomatosis occurs in about 70% of all benign breast diseases. Perhaps more accurate incidence rates are reflected in cohort studies, in which the cumulative incidence of FAM (biopsy-proven diagnoses) by age 65 years was 8.8%, and for fibroadenoma it was 2.2%.
Morphological changes observed in the mammary glands of patients with fibroadenomatosis are characterized by the following features (Semiglazov V.F. et al., 1992):
1) hyperplasia of the epithelial lining of the ducts and lobules of the mammary gland (adenosis or masoplasia). There is an increase in the number and size of the mammary gland lobules;
2) fibrosis of interlobular connective tissue. Manifested by an increase in the number of collagen fibers and a decrease in the number of connective tissue cells;
4) proliferation of epithelial cells, which can be observed in ducts, lobules and cysts.
All these changes can be determined in isolation or combined in different proportions, develop in limited areas of the mammary glands or have multifocal development.
Assessing the severity of proliferative changes in the epithelium in the ducts and lobules of the gland is of primary importance for determining the prognosis and the relative risk of developing breast cancer. In this regard, three forms of FAM are distinguished based on a morphological study of biopsy material:
1) non-proliferative form;
2) proliferative form, without atypia;
3) intraductal atypical proliferation.
Taking into account this classification, the greatest risk of developing breast cancer is observed in groups of women in whom signs of atypical proliferation were detected in the mammary gland.
The most common non-proliferative form of FAM is not characterized by proliferation of the epithelium of lobules and ducts. The relative risk of developing breast cancer for this group of women does not exceed that for the general population. The proliferative form of FAM and, especially, the proliferative form with atypical proliferation increases the risk of developing a malignant neoplasm by 3–5 times.
There is also a pattern in the age-related dynamics of changes in FAM. In girls during the period of formation of menstrual function, immature fibroadenomas are often encountered; in the mature reproductive period (25–39 years), bilateral diffuse FAM increasingly develops. During perimenopause and with the onset of postmenopause (40–49 years), the development of localized forms of FAM, cystic FAM, and sclerosing adenosis is characteristic. With the onset of deep postmenopause, the frequency of proliferative processes and various forms of mastopathy sharply decreases and non-proliferative processes (ductectasia, galactophoritis, fatty involution) come to the fore. But in the same period, the incidence of breast cancer increases sharply (Semiglazov V.F. et al., 1992).
The noted age-related evolution of benign changes in the mammary glands is undoubtedly determined by the age-related dynamics of the secretion of sex hormones. The peak secretion of sex hormones, which occurs throughout the reproductive period, stimulates the proliferation of target tissues, while the decline of ovarian function determines a decrease in hormonal (primarily estrogen) levels and the development of involutive changes in the entire reproductive system.
It is appropriate to note here that using the example of the mammary gland one can see a “concentrated” expression of the entire spectrum of diagnostic problems inherent in hyperplastic syndrome in the reproductive homeostat.
Indeed, the noted disorders are characterized by an extremely wide age range in which they can manifest themselves: from adolescence, in adulthood and in postmenopause.
A fairly wide morphological spectrum of changes in the glandular and ductal epithelium of the mammary glands is determined, which in various “whimsical” combinations form complexes of structures that are very difficult to accept an acceptable morphological classification (see Table 4.3). The situation is saved by simply identifying three main forms of mastopathy, according to morphological criteria: proliferative, without proliferation and with atypical proliferation of the ductal epithelium. According to clinical manifestations, diffuse and nodular forms are distinguished.
If you find an error, please select a piece of text and press Ctrl+Enter.
Fibroadenoma of the breast
Fibroadenoma – what is it?
Fibroadenoma is a benign neoplasm of glandular and connective tissue. The pathology can affect various parts of the female body: skin, tendons, breasts, internal organs, in particular the uterus, ovaries. In the vast majority of cases, this pathology is diagnosed for the mammary glands.
It is this form of neoplasms, the non-cancerous variant, that occurs most often than all others. Fibroadenoma accounts for more than 8% of all diagnoses. At the same time, pathology can be detected at almost any age, but separately there are specific “risk groups” for which the chance of a neoplasm occurring is very high.
- age period from 12 to 20 years (juvenile adenomas and immature neoplasms);
What is this neoplasm?
The development of pathology is impossible to predict. In one case, the tumor will not progress, but very rarely breast fibroadenoma can resolve on its own. In another variant, tumor growth occurs catastrophically quickly. And such a case especially requires medical intervention.
Types of breast fibroadenoma
Pathological neoplasms can be divided into both types and forms.
- immature form - characteristic of “juvenile fibroadenomas” that arise in adolescence and young adulthood; a distinctive feature is the absence of an external capsule of the tumor; it is precisely this difference that in some cases suggests the possibility of eliminating the formation without surgical intervention;
By type, pathology is divided into:
Nodular options include:
- pericanacular fibroadenoma of the mammary gland (deformation of connective tissue next to the glandular ducts);
Leaf-shaped fibroadenoma is a neoplasm that can grow in size at a high rate, and there is a risk of developing sarcoma. The structure of the tumor consists of several layers, similar to leaves. This form of breast adenoma is rare, but requires very rapid medical intervention. And it is characterized by only one form of treatment - surgical correction.
Symptoms of the disease
Breast fibroadenoma can be classified as an insidious pathology due to the fact that it has no external manifestations. As it develops, it does not leave an imprint on your well-being in the form of fever or pain. Often, a neoplasm is discovered in women by chance: either by self-palpation, or during a routine examination by a doctor, or in a situation where a woman goes to the clinic for another reason.
- the appearance of ulcers, cracks on the nipple and near it;
When a benign tumor changes to malignant (sarcoma), the following symptoms may be added:
- the skin above and near the tumor does not change its temperature, but may become reddish or pale bluish;
- The seal is round or oval.
Causes of formation of a benign tumor
The insidiousness of the disease lies in determining the cause. Doctors have not yet identified a clear root cause of the pathology. However, there are hypothetical reasons that provoke the development of fibroadenoma. They can be divided conditionally into external and internal.
- Hormonal imbalance, in which the amount of estrogen significantly exceeds the permissible norm. This can also occur during pregnancy and puberty.
Reasons that can provoke the occurrence of pathology also include:
Disease diagnosis process
Diagnosis occurs in several stages.
- Visual examination by a doctor, palpation process, general collection of information (history taking).
Based on the data obtained from all procedures and studies performed, the doctor draws up a plan for treatment and correction of the condition. The need for surgical intervention is assessed individually.
To remove or not: reasons for different treatment options
The patient cannot make an independent decision regarding the removal of fibroadenoma. This decision is made after discussion with the doctor.
Secondly, at the time of menopause. In this case, the adenoma slows down or completely stops its growth. Without leaving a negative impact on the patient’s health, it does not require surgical correction.
- with its rapid growth, suspicion of transformation into sarcoma, especially when there is a heredity to the development of cancer;
Treatment: surgical and conditionally non-surgical
These forms of condition correction are carried out in clinics. Often either local or general anesthesia is used.
- Sectoral resection. This type of operation is necessary for leaf-shaped fibroadenoma. With this surgical intervention, not only the neoplasm itself is removed, but nearby tissues are also captured (2-3 cm).
- Cryodestruction (tumor freezing).
Recovery postoperative period
Carrying out surgery on the mammary gland due to the occurrence of fibroadenoma is considered the simplest among other surgical interventions.
Additional treatment options for breast fibroadenoma
In a situation where the patient does not want to undergo surgery, and there is no risk to health, replacement therapy can be selected. A treatment plan is drawn up individually, based on the condition and medical history. Therefore, self-medication is contraindicated.
Traditional medicine and diet for breast fibroadenoma
Within the framework of herbal medicine and traditional medicine, treatment of adenoma can be carried out using:
There is no strict diet for such a diagnosis. But it is worth highlighting the basic nutritional rules that you should rely on:
- giving up alcohol and cigarettes; It is better to reduce the amount of tea and coffee consumed per day;
ICD-10, (No. 60-No. 64) breast diseases
The mammary glands are a “mirror” that indirectly reflects the entire state of a woman’s body. The morphology of this organ is a close object of attention for doctors, because in many diseases it is in the chest that the first changes appear. The International Classification of Diseases, 10th revision - ICD 10 combines diseases of the mammary glands under code No. 60-64. This is a group of pathologies with different causes and mechanisms of development, encrypted by doctors with special numbers. What do they mean, and how not to get confused in medical encryption in order to have complete information about your health?
ICD 10 statistics
ICD 10 (No. 60-64) diseases of the mammary glands are subject to careful statistical analysis. This is one of the reasons why a unified classification was introduced. According to the latest data from the World Health Organization, among the female population of the world, up to 40% of women suffer from mastopathy, and more than half of all cases (up to 58%) are combined with gynecological disorders. Of particular interest is the fact that many breast diseases are also precancerous conditions. The incidence and mortality rate from breast cancer is increasing every year, even despite the enormous advances in medicine in the field of early diagnosis and effective treatment. The lion's share of cases occur in developed countries.
Classification approaches ICD No. 10
The internationally accepted classification ICD No. 10 is also used in our country. Based on it, the following are distinguished:
· N 60 – Benign growths of the mammary gland. Mastopathy belongs to this group.
· N 61 - Inflammatory processes. These include carbuncle, mastitis, and abscess.
· N 62 – Breast enlargement.
· N 63 – Unspecified volumetric processes in the chest (nodules and nodules).
Each of these diseases has its own causes, characteristic clinical picture, methods of diagnosis and treatment. Let's talk about this now.
Benign breast dysplasia (N 60)
Clinical picture
The disease can manifest itself with various signs. But the leading main symptoms can be identified:
· Dull pain in the mammary glands, which often tends to intensify before the onset of menstruation. After menstrual bleeding has passed, the pain usually subsides.
· Irradiation – spread of pain beyond the breast. Patients often complain that pain radiates to the shoulder, shoulder blade or arm.
· The presence of a formation in the breast or thickening of its structure. This sign can be identified by patients who are attentive to their health and regularly palpate.
Diagnostics
The doctor begins the examination with a thorough collection of anamnestic data. The doctor asks the patient about the onset of menstruation, its nature, cyclicity, pain, and abundance. Gynecological history is also important, which includes the age at which sexual activity began, the number of pregnancies, miscarriages, abortions, and childbirth. Genealogical data will help to understand whether blood relatives on the female line had similar diseases. All this information helps to establish the correct preliminary diagnosis.
An objective examination will help the doctor identify asymmetry of the mammary glands, and by palpation, determine the presence or absence of neoplasms. Mammologists pay special attention not only to the consistency and structure of the mammary gland, but also to the color, size and condition of the nipples.
Instrumental methods confirm the correctness of the alleged diagnosis or, conversely, refute it and return the doctor to the beginning of the diagnostic search. Most often they resort to mammography and ultrasound of the mammary glands. Additionally, the patient’s blood and urine are studied.
Therapy
Treatment of diseases of the mammary glands No. 60 ICD10 is possible in 2 options. The first is medicinal, which is used for diffuse growths. Hormonal drugs, including oral contraceptives, can achieve good results.
The second method is surgical, which is indicated for the nodular form. The removed lesion is subject to mandatory histological examination to exclude the presence of atypical cancer cells. The prognosis after treatment is favorable.
Inflammatory diseases of the breast (N 61)
ICD-10 No. 61 breast diseases include: abscess, carbuncle and mastitis, which is considered the most common pathology in this group.
Mastitis is an inflammatory disease. Breast involvement is often unilateral, and only in rare cases (no more than 10%) spreads to both mammary glands. The cause of the disease is two main factors that overlap one another:
· The first is a violation of the outflow of milk;
· The second is the addition of pathogenic or conditionally pathogenic microflora.
Initially, the disease occurs as an aseptic (sterile) inflammation. However, very quickly, literally within a day, under conditions of stagnation of milk secretions and favorable temperatures, the microflora is activated. Thus, the stage of bacterial inflammation begins.
Main symptoms
The clinical picture is almost the same in all women. The first symptom is a sharp increase in temperature to high values (38 – 39 °C). Next comes redness of the skin of one of the mammary glands, and then severe pain. Over time they only intensify. With severe inflammation and lack of timely treatment, sepsis develops very quickly - a deadly complication.
Diagnostics
The diagnosis is established on the basis of anamnestic, objective and laboratory data. The medical history reveals that the woman is breastfeeding. As a rule, the risks increase if you constantly attach the baby in the same position. In this case, incomplete emptying of the gland occurs. An objective examination reveals hyperemia of the inflamed gland, its slight enlargement, as well as sharp pain on palpation. A laboratory test in the blood reveals leukocytosis with high values.
Treatment
In the early stages, conservative (medicinal) treatment is also effective. The main condition is careful expression of milk. For these purposes, a breast pump is not the best solution; it is best to do it with your hands. The patient can perform the procedure independently, but often due to severe pain it is necessary to contact specially trained people. Among the drugs, broad-spectrum antibiotics are used. Usually these measures are enough for a complete recovery and further restoration of breastfeeding.
In severe forms of the disease, before prescribing surgical treatment, attempts are made to temporarily stop lactation with the help of special medications. If this method was ineffective, then surgeons take over the treatment.
Other inflammatory diseases of the breast
Carbuncles and abscesses of the mammary gland also occur in clinical practice, but are now becoming less and less common. A carbuncle of the mammary gland, as in any other area of the skin, is a purulent inflammation of the hair follicle and sebaceous gland. An abscess is a purulent melting of the mammary gland limited from healthy tissue.
The cause of the disease with carbuncle is a blockage of the sebaceous gland, against the background of which pathogenic microflora has joined. An abscess can develop as a result of hematogenous or lymphogenous spread of infection from other foci.
Both diseases occur with an increase in temperature and an increase in pain in one of the mammary glands.
Treatment is most often performed surgically. The abscess is opened, freed from purulent contents, treated with an antiseptic solution, and then drainage is installed for a while. The patient is prescribed a course of broad-spectrum antibiotics. With timely treatment, the prognosis is always favorable.
ICD 10 No. 62 – diseases of the mammary glands. Hypertrophy
In this group, it is customary to distinguish gynecomastia, which occurs only in men. It is characterized by the proliferation of breast tissue and, accordingly, its enlargement. In women, this process is called mammary hypertrophy, and also belongs to this group.
The risk of hypertrophy increases the consumption of beer, because this drink contains plant estrogens. They stimulate active cell division.
ICD 10 - N 63 – diseases of the mammary glands. Education unspecified
It is worth noting that this diagnosis is established not only in women, but also in men, but their ratio to each other is 1:18. Mostly women aged 20 to 85 years are affected, but it is more common between 40 and 45 years old. The mortality rate from the disease is 0%.
Causes
The etiology of the disease is not fully understood.
Clinical picture
At first, the disease has no symptoms at all; this is the so-called latent phase of the disease. The duration of this period varies from person to person and can vary from several months to a year or more. The first symptom is periodic pain in the mammary gland, which may intensify before the onset of menstruation. The pain usually subsides immediately after the end of menstruation.
The biggest mistake patients make is that they do not pay attention to changes in their own body and do not turn to doctors, attributing ailments to hormonal imbalances, the beginning of a new cycle, or the proximity of menopause. Over time, the pain takes on a constant aching character. With careful independent palpation, the patient may detect a formation in the chest, which often serves as a reason to consult a doctor.
Diagnostics
Basic research methods:
· assessment of anamnestic data;
· laboratory research methods (general clinical blood test, general urinalysis, biochemical blood test or test for tumor markers);
· instrumental methods (ultrasound, mammography, biopsy).
Treatment
All breast tumors are subject to surgical treatment. After removal, the biological material in 100% of cases is sent for histological examination, thereby establishing an accurate diagnosis and the need for further treatment.
Other diseases of the breast (N64) ICD10
This group includes:
galactocele - a cyst in the thickness of the mammary gland, filled with milk;
· involutive change after breastfeeding;
· secretion from the nipple outside the lactation period;
· Mastodynia is a condition that is perceived subjectively. It is characterized by discomfort in the chest. They may be present constantly or periodically.
Prevention of breast diseases
Propaganda for the prevention of breast diseases occupies a priority place in working tactics among gynecologists and oncologists. This should include social advertising, various medical brochures, preventive conversations with patients at appointments, increasing the popularity of a healthy lifestyle, as well as the approval of World Breast Cancer Day.
To minimize the risk of developing the disease, and not to miss it at an early stage, you should adhere to the following rules:
· refusal of smoking and drinking alcohol;
· treatment of acute diseases, as well as prolongation of the remission phase of chronic ones;
· undergoing preventive examinations, especially over the age of 35;
· performing independent palpation of the mammary glands at home at least once every 4-6 months.
Benign breast dysplasia according to ICD-10 or mastopathy
ICD-10, (No. 60-No. 64) breast diseases. Benign mammary dysplasia according to ICD-10 or mastopathy is a disease of the mammary glands (benign tumor). It appears as a result of tissue proliferation due to various hormonal disorders and there are 2 types: nodular (single compaction) and diffuse mastopathy (with multiple nodes). Mastopathy occurs mainly in women of reproductive age. This phenomenon is easy to explain. Every month, periodic changes occur in a young body under the influence of the hormones estrogen and progesterone, which affect not only the menstrual cycle, but also the tissue of the mammary glands (stimulation and inhibition of cell division, respectively). Hormonal imbalance causing excess estrogen leads to tissue proliferation, i.e. to mastopathy. ICD-10, (No. 60-No. 64) breast diseases. The disease can also be caused by untimely production of prolactin, the lactation hormone (normally it appears during pregnancy and breastfeeding). The development of mastopathy can be provoked by vitamin deficiency, trauma, abortion, hereditary predisposition, chronic diseases, etc. You can feel the appearance of mastopathy yourself. It causes pain in the mammary gland, accompanied by breast enlargement, swelling and hardening. Sometimes there may be discharge from the nipples. If such signs are detected, you should immediately contact a specialist.
ICD-10, (No. 60-No. 64) diseases of the mammary glands according to the International Classification of Diseases
Mastopathy is treated medicinally with the help of hormonal (gestagens, estrogen inhibitors, antiestrogens, androgens, used according to the International Classification of Diseases, ICD-10) and non-hormonal drugs Mabusten. Surgical intervention is used for nodular mastopathy and is diagnosed in two types: sectoral resection (in which the tumor is removed along with the breast area) and enucleation (only the tumor is removed). The operation is indicated if there is a suspicion of breast cancer, the tumor is rapidly growing or there is a single cyst. Lifestyle affects a speedy recovery. During the treatment period, it is better to limit the consumption of tea and coffee, include more vegetables and fruits containing vitamins in the diet, give up bad habits, thermal procedures (for example, in a bathhouse or sauna), and wear comfortable underwear. Diagnosis (by a mammologist) consists of several stages: palpation of the mammary glands in a lying and standing position, examination of the nipples, palpation of the lymph nodes and thyroid gland;
Mammography – x-ray of the mammary glands;
Ultrasound to accurately determine the structure and location of the tumor in the breast;
Biopsy - examination of tissue for oncogenes;
Hormonal studies, liver examination and consultation with specialists (gynecologist, oncologist).
MABUSTEN - MABUSTEN trademark (TM), (R), copyright holder BRADNER DEWORD GmbH, registered in the State Register of the Russian Federation by the Federal Service for Intellectual Property
NEWSLETTER FOR WOMEN MABUSTEN from BRADNER DEWORD GmbH ALL ABOUT FIBROADENOMATOSIS AND BREAST MASTOPATHY
MABUSTIN PREVENTION COMPLEX THERAPY OF FIBROCYSTIC MASTOPATHY-FIBROADENOMATOSIS
Today, breast diseases are becoming more and more common.
This forces doctors to sound the alarm and once again urge women to undergo regular preventive examinations with a mammologist in order to identify ailments in the early stages of development.
Despite the fact that fibroadenoma is a benign pathology, it must be diagnosed on time and treated correctly, since the tumor can provoke health and life-threatening consequences.
Some types of fibroadenoma can degenerate into malignant pathologies, and although this happens infrequently, we cannot forget about this danger.
What it is?
Fibroadenoma is a benign tumor that is localized in the mammary gland and is considered one of the variants of nodular mastopathy.
Under the influence of provoking factors, the connective tissue of the mammary gland proliferates, which leads to the formation of compactions and nodular tumors.
At the same time, the cellular structures do not change their characteristics (remain benign), and do not germinate or metastasize into neighboring organs.
By palpation, fibroadenoma is defined as an oval or round tumor.
The growth of a tumor is determined by the level of hormonal levels; with significant imbalances in the balance of hormones, the tumor can grow, and in some cases quite rapidly.
The consistency of the tumor may vary - soft (immature) fibroadenoma is diagnosed mainly in young women, dense (mature), surrounded by a capsule, more common in women after 40 years.
The size of the tumor can vary from a few mm to several cm.
This depends on the number of tumors - if the form of fibroadenoma is multiple, the size of the tumors is usually small.
Single tumors can be not just large, but gigantic - 15 cm or more.
The tumor can be located on the right or left, and simultaneous damage to both glands can also be observed.
As for the term “fibroadenoma” - it consists of three words - fiber, glandular layer and tumor.
This phrase characterizes the disease in great detail - a tumor of the gland with the proliferation of connective tissue.
Fibroadenoma most often develops asymptomatically, which leads to the fact that the diagnosis of the disease occurs late, when the neoplasm is covered with a dense membrane. Mature forms of the pathology cannot resolve on their own; moreover, drug treatment is also unable to eliminate the tumor. The only effective treatment method remains surgery. Therefore, doctors strongly recommend that women regularly conduct self-examinations and visit a mammologist. If an immature form of fibroadenoma is diagnosed, it can be treated conservatively.
Symptomatic manifestations
The clinical picture of the disease is most often absent.
But in some cases, a woman may feel pain and discomfort in the mammary gland; as a rule, this phenomenon is observed with concomitant mastopathy, which responds to hormonal fluctuations.
A sign of fibroadenoma is the palpation of a dense spherical formation in the upper outer square of the mammary gland, which is not attached to the surrounding tissues and rolls freely under the skin.
The skin over the tumor does not change.

Reasons for appearance
Scientists have not yet established the exact reasons for the formation of fibroadenoma, however, provoking factors are known that can influence the onset of the tumor.
Hormone imbalance is the most common reason that gives impetus to the development of a benign tumor.
In most cases, hormone imbalance occurs due to problems with the liver or ovaries.
In addition, the causes of fibroadenoma may be the following::
- chest injuries;
- abortions;
- pregnancy;
- improper breastfeeding;
- gynecological diseases;
- stress;
- excessive prolonged physical stress;
- diseases of the endocrine system;
- puberty;
- tanning abuse;
- hereditary factor.
CAREFULLY!
Do not assume that fibroadenoma can only occur in women. The stronger sex may also encounter this pathology.
The reasons for the development of fibroadenoma in men are insufficient production of male sex hormones.
Age groups at risk
Fibroadenoma is a disease that is not directly related to age, however, several age groups are more susceptible to the formation and active growth of pathology:
- Teenagers and young girls – 12-20 years old. This is the age when immature forms of fibroadenoma are diagnosed.
- Women under 30 years old. At this age, the most common causes of pathology are nervous strain, abortion, and gynecological and endocrine problems.
- After 40 years, a woman is diagnosed with tumors that have already existed in the mammary gland for several years. The fibroadenoma is already covered with a dense capsule, deposition of calcifications is possible, and the woman can easily feel the tumor under the skin.
In women over 40 years of age, a leaf-shaped form of fibroadenoma is often diagnosed, which has an increased risk of transformation into a malignant neoplasm.
Types of fibroadenoma
Modern medicine classifies fibroadenomas as follows::
- Intracanalicular– fibrous and connective tissue grows in the lumen of the mammary gland ducts.
- Pericanalicular– tissue proliferation is observed around the ducts.
- Mixed– the most common pathology in which there are signs of the previous two types.
- Phylloid (leaf-shaped)– a fast-growing neoplasm that can reach large sizes and also has a risk of transformation into a malignant tumor. This is a borderline state between benign pathology and cancer.
The first three types of fibroadenomas grow quickly, and then can remain inactive for many years.
But in the presence of a provoking factor, for example, pregnancy, tumor growth can become rapid.
In addition, the growth of any fibroadenoma can begin with frequent hot baths, severe stress, inept breast massage, or prolonged exposure to the sun.

Why is it dangerous?
As soon as a woman is diagnosed with fibroadenoma, she has a question about the dangers of this disease.
Small tumors pose virtually no health hazard and do not degenerate into malignant tumors, with the exception of leaf-type tumors.
However, small tumors can begin to grow quickly and, increasing in diameter, can deform the mammary gland, which causes psychological discomfort and pain.
Diagnostic measures
The initial diagnosis of fibroadenoma begins in the mammologist's office - the doctor examines the breast and palpates it.
At the same time, he evaluates:
- presence of pain;
- size of the tumor;
- consistency of the node;
- changes in tissue around the tumor;
- reaction of regional lymph nodes.
- Ultrasound (the procedure is shown in the photo);
- Doppler - study of vascular blood flow;
- mammography;
- biopsy.
Ultrasound is prescribed for young women; older patients should undergo mammography.

Drug treatment
As already mentioned, effective drug treatment is possible only for immature forms of the pathology; in the future, this therapy can only slow down the growth of the tumor.
However, with an accurate determination of the benignity of a tumor whose size does not exceed 8 mm, it is possible to do without surgery.
The doctor will prescribe hormonal drugs based on progesterone, the use of which will slow down or even completely stop the growth of the tumor.
A woman must undergo diagnostics every three months and monitor the condition of the tumor.
If this treatment does not lead to positive results within six months, it is canceled and surgery is prescribed.
Traditional therapy methods
Alternative treatment cannot rid a woman of pathology, but it can improve the condition of the mammary gland, stabilize hormonal levels, stop tumor growth and relieve unpleasant symptoms.
In order to normalize hormonal levels, it is recommended to take half a glass of potato juice three times a day, as well as the following collection of plants:
- fennel;
- chamomile;
- liquorice root;
- wheatgrass;
- marshmallow
All herbs are taken in equal proportions, and a spoonful of the mixture is poured with a glass of boiling water. The product should be taken in three doses per day.
To slow down the growth of the tumor, you can brew and take the following mixture in a similar way::
- chamomile;
- sweet clover;
- plantain;
- nut leaf;
- wheatgrass root.
Used as an anti-inflammatory agent:
- pomegranate peels;
- viburnum branches;
- Oak bark.
The ingredients are mixed, a tablespoon of the mixture is poured with boiling water and cooked for 5 minutes.. Then the decoction should infuse for an hour, after which it can be taken three times a day.

Surgical intervention
Surgical treatment is prescribed in the following cases:
- rapid growth of the tumor;
- transformation into a malignant tumor;
- large size, which led to breast deformation;
- pregnancy planning.
The operation is performed in one of two ways:
- Enucleation– only the tumor is removed, healthy tissue is not affected. This method is used for 100% benign tumors.
- Sectoral resection– the neoplasm is removed along with adjacent tissues.
The surgical intervention is performed under general or local anesthesia and lasts no more than an hour.
The tumor can be removed using minimally invasive or non-invasive methods:
- cryodestruction;
- mammotomy;
- ultrasonic removal;
- high frequency ablation;
- ablation using laser.
Effect on pregnancy
The neoplasm does not prevent conception, and does not in any way affect the course of pregnancy and subsequent childbirth. But pregnancy can have a negative effect on the tumor.
When hormonal levels change, a sharp and active growth of the tumor is possible.
While carrying a child, they try not to remove the tumor, but if there is an urgent need for this, the woman should understand that the surgical intervention will not affect the course of the pregnancy.
Of course, the best option is to plan a pregnancy, and if there are tumors in the mammary gland, remove them before conception.

Preventive measures
Prevention is as follows:
- do not overheat or overcool the mammary gland;
- do not overuse tanning;
- avoid stressful situations;
- promptly treat pathologies that can cause hormonal imbalance;
- do not take hormonal medications without a doctor’s prescription;
- regularly examine the mammary gland - independently and with a mammologist.
Consequences and complications
If fibroadenoma is not treated in a timely manner, it can lead to deformation of the mammary gland, inflammatory processes in the breast, as well as deterioration of the condition of the mammary gland tissue.
But of course, the most dangerous consequence of fibroadenoma is its possible transformation into a malignant tumor, especially for the leaf-shaped form of the disease.
It is imperative to eliminate the causes that led to the formation of fibroadenoma; even after removal of the tumor, a guarantee that relapses of the pathology will not occur can only be obtained when the provoking factors are eliminated.
A benign tumor neoplasm, called in medicine breast fibroadenoma according to the ICD, has code No. 60.2.
The pathology is more common in young women. In adulthood, this problem occurs much less frequently. This disease promotes hyperplasia of connective and glandular tissue.
Signs of fibroadenoma
This lump in the breast is referred to as fibrocystic disease - nodular mastopathy.
Another type of fibroadenoma is leaf-shaped, which has a high growth rate and in 10% of cases develops into sarcoma. This pathology is quite easy to detect upon examination. By palpating the soft tissue of the breast, you can detect a dense formation, having distinct boundaries. If the tumor has reached a significant size, it can be detected with the naked eye. When diagnosing, the doctor prescribes an ultrasound of the mammary glands. In addition to ultrasound, women over 40 are also prescribed mammography. To analyze hormone levels, blood is drawn. A targeted biopsy may be necessary.
Treatment
A patient with lumps in the breast should contact a surgeon or mammologist for consultation without fail. Traditionally, breast fibroadenoma is treated with surgery, since other treatment methods do not demonstrate significant effectiveness and are inappropriate in most cases.
Surgery is resorted to if:
- fibroadenoma is leaf-shaped;
- the size of the formation is more than 1 cm;
- rapid tumor growth;
- pregnancy is planned.
The disease belongs to the class of benign dysplasia along with breast cyst in the international classification of diseases.
After removal of the tumor, the appearance of a new formation cannot be ruled out. Usually this is unlikely; the risk of a neoplasm is no more than 1%.
But this opinion is erroneous, since it can appear in women who have never given birth to children, as well as in men and even in newborn babies.
What is mastitis (ICD code 10), what it is like and what are the reasons for the development of the disease - let's talk about it.
In contact with
Signs
 This disease is characterized by inflammation of one, and in some cases both, mammary glands.
This disease is characterized by inflammation of one, and in some cases both, mammary glands.
In this case, the person experiences pain, the breast becomes heterogeneous, lumps appear in it, it becomes rough, the skin turns red, body temperature rises, and sometimes unusual discharge (pus) appears.
When the first signs of this disease appear, you should consult a specialist, especially if we are talking about a nursing mother .
It is important to know: You cannot continue breastfeeding if you have a purulent form of mastitis, as this can harm the health of the newborn baby.
 Based on the clinical course of the disease, mastitis can be:
Based on the clinical course of the disease, mastitis can be:
- Acute is a form of the disease in which the inflammatory process affects the breast tissue. In most cases, it affects women who have become mothers for the first time, whose children are breastfed;
- Chronic is a form of disease observed over a long period of time, and sometimes throughout life. One of its varieties is plasmacytic mastitis, which occurs mainly in older women.
Causes of lactation mastitis:
- Insufficient expression of milk, resulting in stagnation. This can be combated by careful hand expression or a breast pump. Otherwise, such stagnation can lead to the formation of mastitis;
- Damage to the mammary glands by infections through wounds and cracks that arose as a result of improper attachment of the child to the breast. A striking example is Staphylococcus aureus.
Doctor's comment: various diseases of the thyroid gland, hypertension also contribute to the development of mastitis.
Causes of non-lactation mastitis:
- Damage to the mammary glands by infection;
- Poor health in adults or the perinatal period in newborns.
What is the main purpose of classification
 There is an international classification of absolutely all diseases, the main purpose of which is to assign a class and code to each specific human condition.
There is an international classification of absolutely all diseases, the main purpose of which is to assign a class and code to each specific human condition.
Knowing him, another doctor, scientist or relative can find out what kind of disease the patient has and draw appropriate conclusions about his health. This document is periodically updated, supplemented and each time given a revision number.
The number 10 is the number of the latest revision, and this is what specialists should be guided by in their practice.
Disease code
 Breast diseases are characterized by a disease class from N60 - N64, mastitis corresponds to N 61. Next comes a block of codes from 085 to 092, which describes the main complications that arose after standard childbirth.
Breast diseases are characterized by a disease class from N60 - N64, mastitis corresponds to N 61. Next comes a block of codes from 085 to 092, which describes the main complications that arose after standard childbirth.
In accordance with the International Classification of Diseases, 10th revision (ICD 10), mastitis corresponds to the following codes 091-092:
- Mastitis, the appearance of which is caused by the birth of a child – 091;
- Purulent – 091.1;
- Non-purulent – 091.2.
- The causes of the disease can be determined by the following code:
- Wound or crack of the nipple – 092.1;
- Violation of an unspecified nature 092.2;
- Disorders resulting in initially little or no milk 092.3;
- Decreased breast milk production 092.4;
- The absence of milk or its production in insufficient quantities after normal feeding is sometimes associated with the mother’s health 092.5;
- Disorders associated with excess milk production, and sometimes the development of lactostasis. Codes 092.6 and 092.7 respectively.
Disease code in children
 The block of codes P00-P96 characterizes the condition of newborn children. Mastitis in newborns is classified by code P39.0.
The block of codes P00-P96 characterizes the condition of newborn children. Mastitis in newborns is classified by code P39.0.
Occurs in infants as a result of increased levels of hormones passed to them through the mother’s blood. Treatment in this case is not required, since the disease goes away within a few weeks from the moment the child is born without the intervention of specialists.
Take note: a child who has been diagnosed with this disease is the most vulnerable, so it is necessary to make special demands on the cleanliness of the house, as well as ensure compliance with hygiene rules for all family members.
Using the codes of this classification of diseases, doctors summarize information from all over the world about the number of sick people, the most effective ways and methods of providing care, as well as an analysis of the patient’s condition.
Watch the following video about the features of a disease such as mastitis: