An acute disorder of cerebral circulation due to blockage of cerebral blood vessels will quickly lead to impaired brain function. If this condition lasts more than a day, then they say that the patient had an ischemic stroke or cerebral infarction. This pathological situation most often develops in patients over 50 years of age with chronic diseases such as arterial hypertension, atherosclerotic disease and decompensated diabetes mellitus. In recent years, there has been a clear trend towards the rejuvenation of the contingent of patients.
The prevalence of pathology is quite high in all countries and ranges from 2 to 7 primary cases per year for every thousand inhabitants. In Russia, cerebral ischemic stroke ranks second among the causes of total mortality after coronary heart disease and first in the structure of primary disability in patients of working age. The urgency of the problem dictates the need to educate the population on this issue.
Etiology and pathogenesis
 The human brain is very sensitive to a lack of oxygen, therefore, the cessation of blood supply to its individual sections leads to the rapid death of nerve cells and the development of neurological disorders. This can happen when a blood vessel ruptures, as well as when its lumen is completely or partially closed.
The human brain is very sensitive to a lack of oxygen, therefore, the cessation of blood supply to its individual sections leads to the rapid death of nerve cells and the development of neurological disorders. This can happen when a blood vessel ruptures, as well as when its lumen is completely or partially closed.
The classification is based on this: hemorrhagic and ischemic stroke cerebral infarction. In the first case, we are talking about intracranial hemorrhage. In the second case, cerebral infarction occurs - this is the most common cause of acute cerebrovascular accident, especially in the elderly. This happens when the lumen of a blood vessel that feeds one or another part of the brain is completely or almost completely blocked, as a result, its blood supply stops or significantly worsens.
The pathogenesis of ischemic stroke is similar to. Most often, it is associated with the development of atherosclerotic growths in the mouths of the carotid arteries - these vessels supply blood to all vital structures of the brain. The uneven inner surface of such an artery and slow blood flow in it create all the conditions for thrombosis - the formation of a blood clot inside the vessel. Another cause of ischemic stroke can be an embolism - a thrombus or other formation formed anywhere in the circulatory system, for example, in the cavities of the heart, enters the cerebral artery. In addition to thrombosis and embolism, the following causes lead to cerebral infarction:
- a sharp spasm of the cerebral arteries is a rare phenomenon that occurs a few days after a subarachnoid hemorrhage;
- stenosis (narrowing) of blood vessels due to a sudden drop in pressure in the peripheral arteries (shock, collapse), the situation is aggravated in the presence of atherosclerotic changes in the cerebral basin.
Practical medicine shares concepts, for example, what is an ischemic type of stroke and short-term forms of cerebrovascular accident, which last less than a day and end with the complete disappearance of suddenly disturbed functions.
Transient disorders of cerebral circulation are called transient ischemic attacks, with frequent repetition they can be precursors of cerebral infarction.
In foreign countries, there is the concept of a small stroke. So designate a violation of the blood circulation of the brain, in which all neurological symptoms disappear gradually over a period of a day to three weeks maximum. It is considered as one of the types of ischemic stroke with complete restoration of lost functions or as a reversible neurological deficit of ischemic origin. Sometimes this form is mistaken for a transient attack, which can affect the treatment of a stroke.
Main types and their characteristics
Depending on the pathogenesis, several types of cerebral infarction are distinguished, each has its own characteristics:
- Atherothrombotic form of stroke - develops against the background of atherosclerosis of the cerebral arteries of large and medium diameter. In altered vessels, thrombosis often occurs, in addition, there is always a risk of embolism from other arteries. This type of ischemic stroke is characterized by a gradual gradual development with a debut during a night's rest and an increase in symptoms over several hours / days. Sometimes a transient ischemic attack is a precursor.
- Cardioembolic variant - can occur in people with various heart diseases against the background of the formation of blood clots in its chambers (valvular defects, atrial fibrillation, rheumatism, endocarditis, MK prolapse, etc.). The first signs of this type of ischemic stroke appear suddenly during the active actions of the patient. The lesion is medium or large in size. These patients have a history of thromboembolism of other localizations.
- Cerebral infarction of hemodynamic origin - usually occurs with a sharp decrease in blood pressure (shock, blood loss) and a decrease in cardiac output during myocardial ischemia. The onset of symptoms of a cerebral infarction may be sudden or gradual, during rest or physical activity. Most often it develops as a complication of vascular anomalies, atherosclerosis, stenosis of the cerebral arteries.
- Lacunar type of ischemic stroke - only experts know what it is. The development of pathology is associated with damage to small arteries. Begins cerebral infarction gradually, foci of ischemia are localized in areas located under the cerebral cortex. Characterized by the absence of cerebral symptoms, the course of the type of small stroke.
- Stroke on the background of hemorheological microocclusion - this pathology is associated with a violation of the blood coagulation system (hemostasis) and the process of dissolving intravascular clots (fibrinolysis). A pronounced dissociation between the symptoms of ischemic stroke and hemorheological disorders is characteristic. This means that with a small focus of brain damage and minor neurological disorders, there is a serious intravascular aggregation of blood cells. The way it goes and cerebral infarction, looks like a minor stroke.
There are other classifications of ischemic stroke that are necessary for the practical activities of specialists:
- According to the localization of the focus - the area of blood supply to various arteries, including the internal carotid, vertebral, cerebral branches.
- According to the severity of the stroke - mild (neurological symptoms disappear in 20 days, as with a small form ischemic cerebral infarction), medium (focal symptoms are more pronounced than cerebral, there is no disorder of consciousness), severe degree (cerebral symptoms predominate, depressed consciousness).
Clinical manifestations
Dysfunctions of the brain in acute disorders of cerebral circulation consist of two groups of symptoms:
- Cerebral signs - observed in severe cerebral infarction in the form of impaired consciousness by the type of stupor, drowsiness, agitated state, complete loss is rare. Headache is always present, as well as nausea, vomiting, dizziness, pain in the eyeballs. Less often, there may be convulsions, vegetative disorders - excessive sweating, dryness in the mouth, a feeling of heat, etc.
- Focal neurology in ischemic stroke is an individual set of symptoms for each patient, which depends on which part of the brain is specifically affected, how extensive the lesion is, and whether there are concomitant aggravating circumstances. The half of the body that is opposite to the affected hemisphere always suffers. Focal neurological symptoms include:
- complete violation of movements in the limbs (paralysis) or in partial volume (paresis);
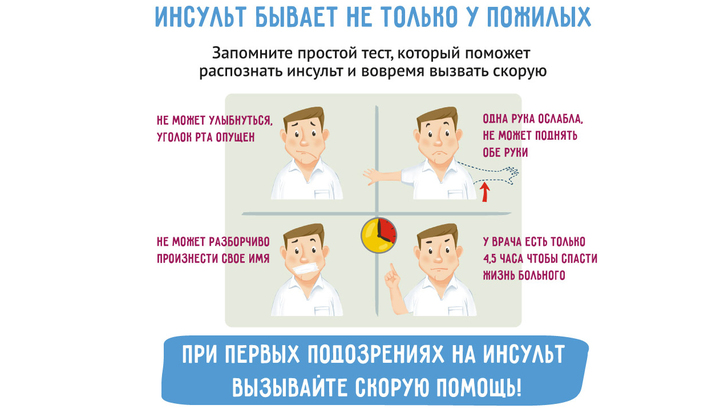
- paralysis and paresis of the facial nerves (drooping of the corner of the mouth or eye, alignment of the nasolabial fold on one side, "sail" cheek, asymmetrical smile);
- visual disturbances (dark or luminous dots before the eyes, decreased visual acuity, loss of fields, diplopia, etc., up to blindness);
- unsteadiness and instability of body position, uncertainty of gait;
- loss of speech to varying degrees, impaired oral and written skills;
- impossibility or difficulties in performing purposeful actions;
- loss of temporal and spatial orientation, memory, etc.
The most severe condition is observed in patients who have had a massive ischemic stroke with several brain lesions, for example, as a result of blockage of the left and right carotid arteries. At the same time, the person is in an unconscious state, he has paralysis of the limbs on the opposite side of the affected cerebral hemisphere. If the patient is not treated correctly for a stroke in the first hours, then there is a high probability of death or the development of serious complications. P The consequence of such a cerebral infarction would be that a person will need constant care from outside. Restoration of movement in the limbs is possible only in a very small percentage of cases. The main therapeutic measures are used to prevent recurrence of ischemic stroke.
Survey
It should be noted that the suspicion of acute cerebrovascular accident is the reason for the immediate hospitalization of the patient in the neurological department of the hospital.
What is it - a diagnosis of a heart attack brain or other similar disease, as well as the establishment of its pathogenetic variety should be carried out as soon as possible after the patient's admission to the hospital.
Clinical diagnosis of ischemic stroke is based on the following criteria:
- in the anamnesis the patient has indications of repeated transient attacks;
- angina pectoris or signs of ischemic processes in the lower extremities were previously detected;
- have heart disease (atrial fibrillation, rheumatic valvular disease, bacterial endocarditis, coronary artery disease, etc.);
- the onset of the disease during a night's sleep, after taking a bath with hot water, physical work, or during (after) an attack of arrhythmia or angina pectoris, after blood loss, etc .;
- the progression of the pathological process is gradual or stepwise;
- patient age category 50+;
- the predominance of focal signs over cerebral neurological manifestations.
In the emergency room of the hospital, an assessment of the general and neurological status of the patient is carried out, general clinical blood and urine tests are performed, additional laboratory tests are prescribed at the discretion of the doctor. A maximum of 40 minutes after admission to the emergency room of the hospital, the patient should be transferred to a specialized department, and stroke treatment should be started.
Among the instrumental methods of examination, the main ones are:
- Dynamic electrocardiogram recording.
- CT scan of the brain - to exclude possible intracerebral hemorrhage.
- MRI in T1 and T2 modes - to assess the extent of the lesion, to confirm the severity of the process and differentiate the diagnosis.
- Doppler ultrasonography of blood vessels located inside and outside the skull.
Additionally, in each specific case, other types of studies may be assigned:
- Ultrasound of the heart;
- ECG monitoring per day according to Holter;
- echoencephalography;
- Ultrasound of the kidneys, abdominal organs, etc., according to indications.
Principles of therapy
 Treatment of ischemic stroke in the acute period is carried out mainly by conservative methods. The basis is thrombolytic (clot-dissolving) intravenous therapy. A special preparation of a protein nature is used, which converts plasminogen into its active form (plasmin enzyme), which has fibrinolytic activity. It effectively dissolves blood clots in the cerebral vessel when used early (during the first 3-4 hours from the onset of the disease) and can significantly alleviate the patient's condition.
Treatment of ischemic stroke in the acute period is carried out mainly by conservative methods. The basis is thrombolytic (clot-dissolving) intravenous therapy. A special preparation of a protein nature is used, which converts plasminogen into its active form (plasmin enzyme), which has fibrinolytic activity. It effectively dissolves blood clots in the cerebral vessel when used early (during the first 3-4 hours from the onset of the disease) and can significantly alleviate the patient's condition.
This method of therapy is carried out only after agreement with the patient or his close relatives, while the diagnosis must be confirmed by CT and the exact time of onset of the disease must be known. Patients with severe ischemic infarction who are unconscious, thrombolysis is contraindicated.
How to treat ischemic stroke when it is impossible to carry out thrombolysis or after its completion - no later than two days after the onset of the disease, antiplatelet drugs are prescribed that prevent the formation of dense blood clots. For example, Acetylsalicylic acid, Dipyridamole MB or Clopidogrel. Subsequently, Warfarin or drugs based on Aspirin are administered orally for at least six months. Such therapy is especially indicated in patients suffering from angina attacks or who have had a myocardial infarction.
Treatment of ischemic stroke after a hospital is carried out under the supervision of a neurologist. The goal is to prevent relapses and complications. Drug therapy should be carried out in combination with means of psychotherapeutic support and adaptation of a person to new living conditions, including the restoration of lost functions (exercise therapy, massage, physiotherapy, etc.).
There is hope for a new direction in the use of stem cells to restore lost neurons, work in this vein is actively being carried out in a number of countries, including ours. Primary prevention of ischemic stroke consists in actively identifying risk groups and taking measures in accordance with the existing pathology, for example:
- struggle with extra pounds of body weight;
- treatment of diabetes and hypertension;
- taking antithrombotic drugs for atrial fibrillation, aspirin and statins in patients with coronary artery disease, etc.
The prognosis depends on the volume and localization of the focus of ischemia in the brain, the age and characteristics of the patient's body.


