Myocardial infarction: causes, first signs, help, therapy, rehabilitation
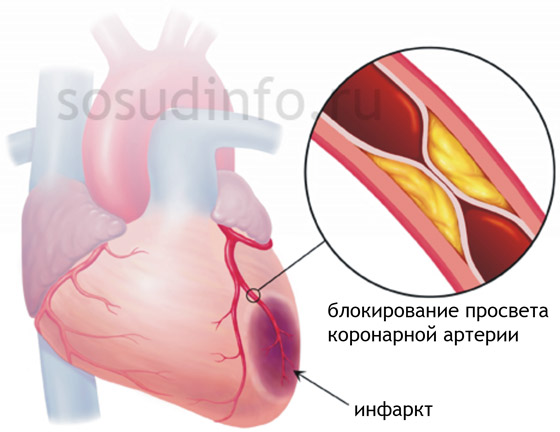
Myocardial infarction is one of the forms, which is necrosis of the heart muscle, caused by a sharp cessation of coronary blood flow due to damage to the coronary arteries.
Heart and vascular diseases continue to occupy the leading position in terms of the number of deaths worldwide. Every year, millions of people are faced with one or another manifestation of coronary heart disease - the most common form of myocardial damage, which has many types, invariably leading to disruption of the usual way of life, disability and taking the life of a large number of patients. One of the most common manifestations of IHD is myocardial infarction (MI), at the same time, it is the most common cause of death in such patients, and developed countries are no exception.
According to statistics, in the United States alone, about a million new cases of heart muscle infarction are registered per year, about a third of patients die, with about half of deaths occurring within the first hour after the development of necrosis in the myocardium. Increasingly, among the sick there are able-bodied people of young and mature age, and there are several times more men than women, although by the age of 70 this difference disappears. With age, the number of patients is steadily increasing, among them more and more women appear.
However, one cannot fail to note the positive trends associated with a gradual decrease in mortality due to the emergence of new diagnostic methods, modern methods of treatment, as well as increased attention to those risk factors for the development of the disease that we ourselves are able to prevent. Thus, the fight against smoking at the state level, the promotion of the basics of healthy behavior and lifestyle, the development of sports, the formation of public responsibility for their health significantly contribute to the prevention of acute forms of coronary artery disease, including myocardial infarction.
Causes and risk factors for myocardial infarction
Myocardial infarction is a necrosis (necrosis) of a section of the heart muscle due to the complete cessation of blood flow through the coronary arteries. The reasons for its development are well known and described. The result of various studies of the problem of coronary heart disease has been the identification of many risk factors, some of which do not depend on us, while others can be excluded from our lives.
As you know, hereditary predisposition plays an important role in the development of many diseases. Ischemic heart disease is no exception. Thus, the presence among blood relatives of patients with IHD or other manifestations of atherosclerosis significantly increases the risk of myocardial infarction. , various metabolic disorders, for example, are also a very unfavorable background.
There are also so-called modifiable factors contributing to acute coronary heart disease. In other words, these are the conditions that can either be completely eliminated or significantly reduce their influence. At present, thanks to a deep understanding of the mechanisms of the development of the disease, the emergence of modern methods of early diagnosis, as well as the development of new drugs, it has become possible to deal with lipid metabolism disorders, maintain normal blood pressure values and an indicator.
Do not forget that the exclusion of smoking, alcohol abuse, stress, as well as good physical shape and maintaining adequate body weight significantly reduce the risk of cardiovascular disease in general.
The causes of heart attack are conventionally divided into two groups:
- Significant atherosclerotic changes in the coronary arteries;
- Non-atherosclerotic changes in the coronary arteries of the heart.
Damage and inflammation of the endocardium is fraught with the occurrence of blood clots and thromboembolic syndrome, and pericarditis over time will lead to the growth of connective tissue in the cavity of the heart shirt. At the same time, the pericardial cavity overgrows and the so-called "shell heart" is formed, and this process underlies the formation in the future due to the restriction of its normal mobility.
With timely and adequate medical care, most of the patients who survived acute myocardial infarction remain alive, and a dense scar develops in their heart. However, no one is immune from repeated episodes of circulatory arrest in the arteries, even those patients in whom the patency of the heart vessels was restored surgically (). In those cases when, with an already formed scar, a new focus of necrosis occurs, they speak of a repeated myocardial infarction.
As a rule, the second heart attack becomes fatal, but the exact number that the patient is able to endure has not been determined. In rare cases, there are three transferred episodes of necrosis in the heart.
Sometimes you can find the so-called recurrent heart attack which occurs during a period of time when scar tissue forms in the heart at the site of the transferred acute. Since, as mentioned above, it takes an average of 6-8 weeks for the “maturation” of the scar, it is during such periods that a relapse is possible. This type of heart attack is very unfavorable and dangerous for the development of various fatal complications.
Sometimes an occurrence occurs, the causes of which will be thromboembolic syndrome with extensive transmural necrosis with involvement of the endocardium in the process. That is, blood clots formed in the cavity of the left ventricle when the inner lining of the heart is damaged, enter the aorta and its branches that carry blood to the brain. When the lumen of the cerebral vessels is blocked, necrosis (infarction) of the brain occurs. In such cases, these necrosis is not called a stroke, since they are a complication and consequence of myocardial infarction.
Varieties of myocardial infarction
To date, there is no single generally accepted classification of cardiac infarction. In the clinic, based on the amount of necessary assistance, the prognosis of the disease and the characteristics of the course, the following varieties are distinguished:
- macrofocal myocardial infarction - it can be transmural and not transmural;
- Small focal- intramural (in the thickness of the myocardium), subendocardial (under the endocardium), subepicardial (in the area of the heart muscle under the epicardium);
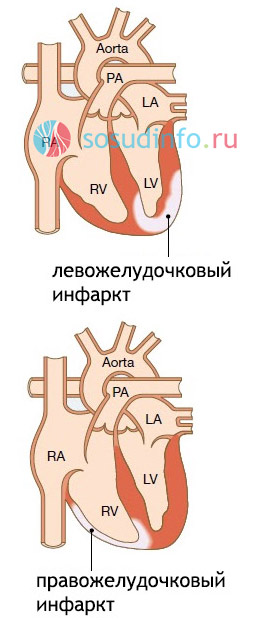
- Myocardial infarction of the left ventricle (anterior, apical, lateral, septal, etc.);
- right ventricular infarction;
- Atrial myocardial infarction;
- Complicated and uncomplicated;
- Typical and atypical;
- Protracted, recurrent, repeated heart attack.
In addition, allocate flow periods myocardial infarction:
- Sharpest;
- Spicy;
- Subacute;
- Postinfarction.
Symptoms of a heart attack
The symptoms of myocardial infarction are quite characteristic and, as a rule, make it possible to suspect it with a high degree of probability even in preinfarction period the development of the disease. So, patients experience more prolonged and intense retrosternal pain, which are less amenable to treatment with nitroglycerin, and sometimes do not go away at all. IN You may experience shortness of breath, sweating, various and even nausea. At the same time, patients are increasingly difficult to tolerate even minor physical exertion.
At the same time, characteristic electrocardiographic signs circulatory disorders in the myocardium, and constant monitoring for a day or more is especially effective for their detection ().
The most characteristic signs of a heart attack appear in acute period when a zone of necrosis appears and expands in the heart. This period lasts from half an hour to two hours, and sometimes longer. There are factors that provoke the development of an acute period in predisposed individuals with atherosclerotic lesions of the coronary arteries:
- Excessive physical activity;
- Strong stress;
- Operations, injuries;
- Hypothermia or overheating.
The main clinical manifestation of necrosis in the heart is pain, which is very intense. Patients can characterize it as burning, squeezing, pressing, "dagger". Soreness has retrosternal localization, can be felt to the right and left of the sternum, and sometimes covers the front of the chest. Characteristic is the spread (irradiation) of pain in the left arm, shoulder blade, neck, lower jaw.
In most patients, the pain syndrome is very pronounced, which also causes certain emotional manifestations: a feeling of fear of dying, marked anxiety or apathy, and sometimes excitement is accompanied by hallucinations.
Unlike other types of coronary artery disease, a painful attack during a heart attack lasts at least 20-30 minutes, and there is no analgesic effect of nitroglycerin.
Under favorable circumstances, at the site of the focus of necrosis, the so-called granulation tissue begins to form, rich in blood vessels and fibroblast cells that form collagen fibers. This period of myocardial infarction is called subacute and lasts up to 8 weeks. As a rule, it proceeds safely, the condition begins to stabilize, the pain weakens and disappears, and the patient gradually gets used to the fact that he suffered such a dangerous phenomenon.
In the future, a dense connective tissue scar is formed in the heart muscle at the site of necrosis, the heart adapts to new working conditions, and postinfarction marks the onset of the next period of the course of the disease, continuing for the rest of life after a heart attack. Those who have had a heart attack feel satisfactory, but there is a resumption of pain in the region of the heart and seizures.
As long as the heart is able to compensate for its activity due to hypertrophy (increase) of the remaining healthy cardiomyocytes, there are no signs of its insufficiency. Over time, the adaptive capacity of the myocardium is depleted and heart failure develops.
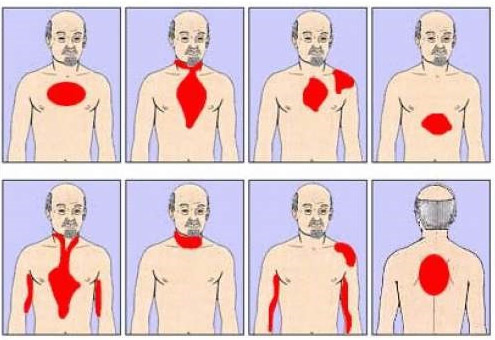
projections of pain in myocardial infarction
It happens that the diagnosis of myocardial infarction is significantly complicated by its unusual course. This characterizes its atypical forms:
- Abdominal (gastralgic) - characterized by pain in the epigastrium and even throughout the abdomen, nausea, vomiting. Sometimes it can be accompanied by gastrointestinal bleeding associated with the development of acute erosions and ulcers. This form of infarction must be distinguished from peptic ulcer of the stomach and duodenum, cholecystitis, pancreatitis;
- Asthmatic form - occurs with asthma attacks, cold sweat;
- Edematous form - characteristic of massive necrosis with total heart failure, accompanied by edematous syndrome, shortness of breath;
- Arrhythmic form, in which rhythm disturbances become the main clinical manifestation of MI;
- Cerebral form - accompanied by the phenomena of cerebral ischemia and is typical for patients with severe atherosclerosis of blood vessels supplying the brain;
- Erased and asymptomatic forms;
- Peripheral form with atypical localization of pain (mandibular, left-handed, etc.).
Video: non-standard signs of a heart attack
Diagnosis of myocardial infarction
Usually the diagnosis of a heart attack does not cause significant difficulties. First of all, it is necessary to carefully clarify the patient's complaints, ask him about the nature of pain, clarify the circumstances of the attack and the effect of nitroglycerin.

On examination the patient is noticeable pallor of the skin, signs of sweating, cyanosis (cyanosis) is possible.
A lot of information will be given by such methods of objective research as palpation(feel) and auscultation(listening). So, at can be identified:
- Pulsation in the region of the cardiac apex, precordial zone;
- Increased heart rate up to 90 - 100 beats per minute;
On auscultation hearts will be characteristic:
- Muting the first tone;
- Quiet systolic murmur at the apex of the heart;
- A gallop rhythm is possible (the appearance of a third tone due to left ventricular dysfunction);
- Sometimes IV tone is heard, which is associated with stretching of the muscle of the affected ventricle or with a violation of the impulse from the atria;
- Perhaps systolic "cat's purr" due to the return of blood from the left ventricle to the atrium with pathology of the papillary muscles or stretching of the ventricular cavity.
In the vast majority of patients suffering from a macrofocal form of myocardial infarction, there is a tendency to lower blood pressure, which, under favorable conditions, can normalize in the next 2-3 weeks.
A characteristic symptom of necrosis in the heart is also an increase in body temperature. As a rule, its values do not exceed 38 ºС, and the fever lasts for about a week. It is noteworthy that in younger patients and in patients with extensive myocardial infarction, the increase in body temperature is longer and more significant than in small foci of infarction and in elderly patients.
In addition to physical, important laboratory methods diagnosis of MI. So, in the blood test, the following changes are possible:
- An increase in the level of leukocytes () is associated with the appearance of reactive inflammation in the focus of myocardial necrosis, persists for about a week;
- - associated with an increase in the concentration in the blood of proteins such as fibrinogen, immunoglobulins, etc .; the maximum falls on the 8-12th day from the onset of the disease, and the ESR numbers return to normal after 3-4 weeks;
- The appearance of the so-called "biochemical signs of inflammation" - an increase in the concentration of fibrinogen, seromucoid, etc.;
- The appearance of biochemical markers of necrosis (death) of cardiomyocytes - cellular components that enter the bloodstream when they are destroyed (, troponins, and others).
It is difficult to overestimate the importance of (ECG) in the diagnosis of myocardial infarction. Perhaps this method remains one of the most important. An ECG is available, easy to perform, can be recorded even at home, and at the same time it provides a large amount of information: it indicates the location, depth, prevalence of a heart attack, the presence of complications (for example, arrhythmias). With the development of ischemia, it is advisable to record the ECG repeatedly with comparison and dynamic observation.
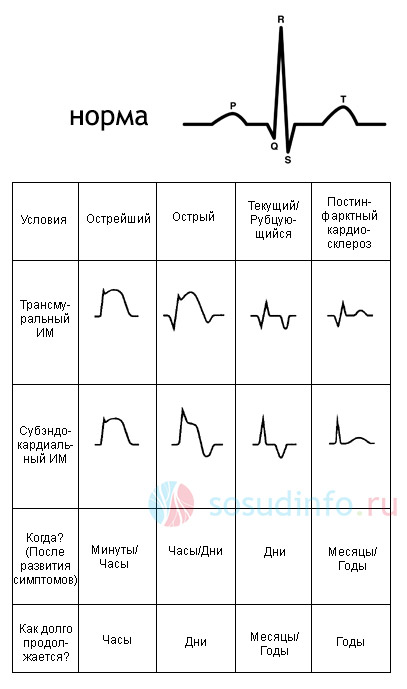
table: private forms of infarction on the ECG
ECG signs of an acute phase of necrosis in the heart:
- the presence of a pathological Q wave, which is the main sign of necrosis of muscle tissue;
- a decrease in the size of the R wave due to a decrease in the contractile function of the ventricles and the conduction of impulses along the nerve fibers;
- dome-shaped displacement of the ST interval upwards from the isoline due to the spread of the infarction focus from the subendocardial zone to the subepicardial zone (transmural lesion);
- T wave formation.
By typical changes in the cardiogram, it is possible to establish the stage of development of necrosis in the heart and accurately determine its localization. Of course, it is unlikely that it will be possible to independently decipher the cardiogram data without having a medical education, but the doctors of the ambulance teams, cardiologists and therapists can easily establish not only the presence of a heart attack, but also other disorders of the heart muscle and.
In addition to these methods, for the diagnosis of myocardial infarction are used (allows you to determine the local contractility of the heart muscle), , magnetic resonance and (helps to assess the size of the heart, its cavities, to identify intracardiac blood clots).
Video: lecture on the diagnosis and classification of heart attacks
Complications of myocardial infarction
Myocardial infarction in itself poses a threat to life, and through its complications. The majority of those who have undergone it have certain disturbances in the activity of the heart, associated primarily with changes in conduction and rhythm. So, in the first day after the onset of the disease, up to 95% of patients face arrhythmias. Severe arrhythmias in massive heart attacks can quickly lead to heart failure. Possibility, thromboembolic syndrome also cause many problems for both doctors and their patients. Timely assistance in these situations will help the patient to prevent them.

The most common and dangerous complications of myocardial infarction:
- Heart rhythm disturbances (, tachycardia, etc.);
- Acute heart failure (with massive heart attacks, atrioventricular blockades) - it is possible to develop acute left ventricular failure with symptoms and alveolar pulmonary edema that threaten the patient's life;
- - extreme degree of heart failure with a sharp drop in blood pressure and impaired blood supply to all organs and tissues, including vital ones;
- Rupture of the heart is the most severe and fatal complication, accompanied by the release of blood into the pericardial cavity and a sharp cessation of cardiac activity and hemodynamics;
- (protrusion of the myocardium in the focus of necrosis);
- Pericarditis - inflammation of the outer layer of the heart wall in transmural, subepicardial infarcts, accompanied by constant pain in the region of the heart;
- Thromboembolic syndrome - in the presence of a thrombus in the infarction zone, in the aneurysm of the left ventricle, with prolonged bed rest,.
Most deadly complications occur in the early post-infarction period, so careful and constant monitoring of the patient in a hospital setting is very important. The consequences of extensive heart infarction are macrofocal post-infarction cardiosclerosis (a massive scar that replaced the site of dead myocardium) and various arrhythmias.
Over time, when the ability of the heart to maintain adequate blood flow in organs and tissues is depleted, it appears congestive (chronic) heart failure. Such patients will suffer from edema, complain of weakness, shortness of breath, pain and interruptions in the work of the heart. Increasing chronic circulatory failure is accompanied by irreversible dysfunction of internal organs, accumulation of fluid in the abdominal, pleural and pericardial cavities. Such decompensation of cardiac activity will eventually lead to the death of patients.
Principles of treatment of myocardial infarction
Emergency care for patients with myocardial infarction should be provided as soon as possible from the moment of its development., since delay can lead to the development of irreversible changes in hemodynamics and sudden death. It is important that there is someone nearby who can at least call an ambulance. If you are lucky and there is a doctor nearby, his qualified participation can help to avoid serious complications.

The principles of helping patients with a heart attack are reduced to the phased provision of therapeutic measures:
- Pre-hospital stage - provides for the transportation of the patient and the provision of necessary measures by the ambulance team;
- At the hospital stage, maintenance of the basic functions of the body, prevention and control of thrombosis, cardiac arrhythmias and other complications in the intensive care units of the hospital continue;
- The stage of rehabilitation measures - in specialized sanatoriums for cardiological patients;
- The stage of dispensary observation and outpatient treatment is carried out in polyclinics and cardio centers.
First aid can be provided under time pressure and outside the hospital. It is good if it is possible to call a specialized ambulance cardio brigade, which is equipped with the necessary for such patients - medicines, a pacemaker, equipment for resuscitation. Otherwise, it is necessary to call a linear ambulance brigade. Now almost all of them have portable ECG devices, which make it possible to make a fairly accurate diagnosis and start treatment in a short time.
The main principles of care before coming to the hospital are adequate pain relief and prevention of thrombosis. In this case, apply:
- under the tongue;
- The introduction of analgesics (promedol, morphine);
- aspirin or heparin;
- Antiarrhythmic drugs as needed.
Video: first aid for myocardial infarction
At the stage of inpatient treatment ongoing measures to maintain the function of the cardiovascular system. Eliminating pain is the most important of them. Narcotic analgesics (morphine, promedol, omnopon) are used as analgesics; if necessary (pronounced excitement, fear), tranquilizers (relanium) are also prescribed.
It matters a lot. With its help, lysis (dissolution) of a thrombus in the coronary and small arteries of the myocardium is carried out with the restoration of blood flow. This also limits the size of the focus of necrosis, which improves the subsequent prognosis and reduces mortality. Of the drugs with thrombolytic activity, fibrinolysin, streptokinase, alteplase, etc. are most commonly used. An additional antithrombotic agent is heparin, which prevents thrombosis in the future and prevents thromboembolic complications.
It is important that thrombolytic therapy be started as early as possible, preferably within the first 6 hours after the development of a heart attack, this significantly increases the likelihood of a favorable outcome due to the restoration of coronary blood flow.
With the development of arrhythmias, are assigned antiarrhythmic drugs, to limit the zone of necrosis, unload the heart, as well as for cardioprotective purposes, are prescribed (propranolol, atenolol), nitrates (nitroglycerin intravenously), vitamins (vitamin E, xanthinol nicotinate). 
Supportive care after a heart attack can continue for the rest of your life, its directions:
- Maintaining a normal level of blood pressure;
- Fight against arrhythmias;
- Prevention of thrombosis.
It is important to remember that only timely and adequate drug treatment can save the patient's life, and therefore herbal treatment will by no means replace the possibilities of modern pharmacotherapy. At the stage of rehabilitation in combination with supportive treatment, it is quite it is possible to take various herbal decoctions as a supplement. So, in the post-infarction period, it is possible to use motherwort, hawthorn, aloe, calendula, which have a tonic and calming effect.
Diet and rehabilitation
An important role is given to the nutrition of patients with myocardial infarction. So, in the intensive care unit in the acute period of the course of the disease, it is necessary to provide such food that will not be burdensome for the heart and blood vessels. Easily digestible, non-rough food is allowed, taken 5-6 times a day in small portions. Various cereals, kefir, juices, dried fruits are recommended. As the patient's condition improves, the diet can be expanded, but it is worth remembering that fatty, fried and high-calorie foods that contribute to the disruption of fat and carbohydrate metabolism with the development of atherosclerosis are contraindicated.
In the diet after a heart attack, it is necessary to include products that promote bowel movement (prunes, dried apricots, beets).
Rehabilitation includes a gradual expansion of the patient's activity, and, in accordance with modern concepts, the sooner it comes, the more favorable the further forecast. Early activity is the prevention of congestion in the lungs, muscle atrophy, osteoporosis and other complications. Physical rehabilitation after a heart attack is also important, which involves physical therapy, walking.
With a satisfactory condition of the patient and the absence of contraindications, further recovery is possible in cardiological sanatoriums.
The terms of disability after a heart attack are determined individually, depending on the severity of the course and the presence of complications. Disability reaches significant numbers, and it is all the more sad that more and more young and able-bodied population suffers. Patients will be able to work if their work is not associated with strong physical or psycho-emotional stress, and the general condition is satisfactory.



