As a result of injuries, infectious and viral diseases, previous operations, frequent use of contact lenses, clouding of the cornea of \u200b\u200bthe eye occurs. Pathology is characterized by a violation of the transparency of the cornea, which leads to reduced vision. In severe cases, the disease leads to blindness. To avoid complications, you should seek medical help at the first symptoms of the disease.
Causes and risk factors
In the absence of therapy, scars form on the cornea, and a white or white-gray spot appears, which impairs vision.
The following causes of the disease are distinguished:
- Injuries. Due to damage to the outer membrane, pathogenic microorganisms penetrate into the eye, corroding tissues and provoking the formation of wounds. Gradually, a scar appears at the site of the ulcer.
- Virus infection. The transparency of the cornea changes under the influence of conjunctivitis or herpes viruses if the cornea is inflamed.
- Surgical treatment. The inner layer of the cornea is made up of endothelial cells that do not heal when the lining of the eye is damaged. After surgery, corneal dystrophy and loss of transparency may develop.
 This disease is often diagnosed in welders.
This disease is often diagnosed in welders. Clouding of the cornea is caused by frequent exposure to bright light. This puts welders at risk. It is important for people who use contact lenses to follow the rules of hygiene, as there is a high probability of infection in the eye. In addition, the condition of the cornea is affected by:
- allergy;
- lack of vitamins;
- trigeminal nerve.
3 types of violation
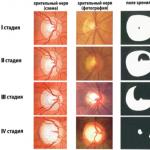
Corneal opacity has several forms, depending on the intensity of the disease and the area of \u200b\u200bthe lesion:
- Clouds. A gray cloudy spot is formed, similar to smoke or a cloud, with certain boundaries. It may appear that the person has cloudy eyes. If the spot is in the middle of the cornea, vision is impaired.
- Spots. Cicatricial opacities form in the middle or along the edges of the cornea. A persistent spot significantly impairs vision, in children it can provoke strabismus.
- Belmo. The opacity takes up most of the cornea and forms as a result of scarring. Belmo is like porcelain or frosted glass. It may be a congenital pathology after an intrauterine inflammatory process.
How does pathology manifest?
 Intense lacrimation is one of the frequent manifestations of the disease.
Intense lacrimation is one of the frequent manifestations of the disease. The decrease in the transparency of the cornea is visible without special equipment. The disease has the following symptoms:
- redness of the eyes;
- intense lacrimation;
- sensitivity to light;
- the feeling of the presence of a foreign object in the eye;
- opacity of the cornea;
- decreased visual acuity.
The affected area appears as a gray nebula, a white or white-gray dense spot, against which a vascular pattern is visible. If a thorn is formed on the pupil, the eye loses its functionality. If the wound that provoked damage to the cornea reaches the iris, a fused leucorrhoea is formed, as the cornea and iris grow together. In glaucoma, high pressure causes the scar to stretch. At the first sign of the disease, seek medical attention, otherwise you may lose your vision. To make a diagnosis, anamnesis and examination are carried out. As part of the preparation, the patient's eyes are buried with special drops that dilate the pupils. Amsler grating is used to confirm the diagnosis. The patient is asked to look at a specific point on the grating. When blurred, the lines surrounding the point appear curved. Fluorescein angiography is performed as needed.
- This is one of the most ancient and common eye diseases. Medieval doctors, including the legendary Avicenna, mentioned her in their works. In our time, people, unfortunately, suffer from the disease almost as often as in the Middle Ages. Only now this ailment is called differently. Its medical name is corneal opacity. Initially, this disease is not very dangerous and does not cause anything except discomfort and partial deterioration of vision. But if it is not cured in time, then complications can be very serious, up to a complete loss of vision in one eye.
What are the types of corneal opacities?

This disease is divided into 3 types depending on the size and intensity of the opacity. It is interesting that before all types were called thorns, but now - only one of them. So these are the categories.

Thorn in the human eye
- Cloud... This is the name for a small, limited grayish haze, which is not easy to see with the naked eye. Such clouds are most often located closer to the center of the cornea, but due to their small size, they do not significantly affect a person's ability to see.
- Spot... This is the name given to limited opacities of higher intensity than cloudy ones. They can be found both in the center and at the periphery of the eye. Due to its high intensity, this type of cloudiness seriously affects the ability to see.
- Belmo... This is the most serious type of ailment. Such persistent opacification usually appears with scarring and can occupy both part of the cornea and its entirety. Belmo is the only type of ailment that can cover the entire eye.

Causes of corneal opacity
This disease has a whole list of possible causes. These include inflammatory and infectious eye diseases, trauma, and serious deficiencies in the hygiene of the visual organs. A complete list of possible reasons is as follows:
- (shown in the photo);


- infections (most often conjunctivitis);
- herpes that affects the surface of the eyes;
- eye injuries (chemical, mechanical, and also caused by various foreign objects);
- complications after eye surgery;
- complications of certain diseases (syphilis, measles, and tuberculosis);
- lack of vitamin A in the body;
- mistakes when working with lenses (sleeping in lenses, caring for them not according to instructions);
- getting dirt on the surface of the eyes and its long stay there.

Important! Turbidity can occur for no apparent reason. This is very rare, but it does happen sometimes. Therefore, even if there were no apparent reasons for the onset of the disease, if your vision deteriorates, you should immediately go to the doctor.
Symptoms

The disease can be easily identified by the following symptoms:
- a cloudy spot that interferes with the ability to see normally (however, a cloud may not be noticed during visual inspection - an example in the photo);
- significant deterioration in vision in the affected eye, and sometimes - its complete loss;
- reddened proteins;
- increased fear of light;
- tearing;
- an unpleasant feeling as if a foreign object had got into the eye;
- increasing discomfort when blinking.

Important! Ophthalmologists say that the presence of one symptom is already a sufficient reason for going to the clinic. If there are 2 or more symptoms, you need to see a doctor as soon as possible.
Possible complications
If you do not start the treatment of corneal opacity in time, then several complications may occur:
- increased discomfort in the eye;
- the appearance of pain, aggravated by blinking;
- severe visual impairment, much more significant than at the onset of the disease;
- complete loss of vision in the affected eye.

To avoid irreparable complications, treatment should be started in a timely manner - as soon as the disease has made itself felt.
How is the disease diagnosed?
There are several generally accepted ways to diagnose corneal opacity.


All diagnostic procedures are absolutely painless and do not cause discomfort. Therefore, there is absolutely no need to be afraid of diagnostics. Compared to the discomfort of cloudiness, the diagnosis may seem pleasant.
Treatment types
By contacting an ophthalmologist in a timely manner, the ailment can be effectively cured. The treatment process can be divided into 2 categories:
- the use of medicines;
- surgery.

This table compares both treatments. In short, the operation will be needed only in advanced cases, when the patient came to the doctor too late, or when medications did not help.
| Comparison criterion | Medication | Operation |
|---|---|---|
| Effectiveness in the early stages of the disease | very high | very high, but surgery is usually not required in the early stages |
| Effectiveness in the late stages of the disease | low | very high |
| The effectiveness of maintenance therapy (electrophoresis, phonophoresis, exercise) with the selected method of treatment | very high | very high, but only used as directed by a doctor |
| The possibility of self-medication | is absent | is absent |
| Contraindications | absent (except for allergies) | yes (advanced age, the presence of some other diseases) |
| Compatibility with traditional medicine | good | bad (only on the recommendation of a doctor, no amateur performance) |
If the patient needs an operation, then drug treatment should also not be abandoned. The drugs provide the organs of vision with the necessary support, promote rapid healing after surgery and reduce the risk of postoperative complications.

Important! You need to be very careful with your eyes, so self-medication with folk remedies is not a good idea. They can be used, but only in combination with traditional medicine, as a complementary therapy. You should also make sure that the selected recipes do not conflict with the drugs prescribed by the doctor.
Drug treatment
It is always possible to treat corneal opacity with medication (except in cases where there is an allergy to drugs). But such treatment is self-sufficient only in the early stages of the disease. At a later stage, medications must be combined with surgery, otherwise a complete cure cannot be achieved.
The most common and effective types of medical treatment are as follows.
- To eliminate the symptoms of the disease and relieve inflammation, use eye drops and ointments for the eyelids. The most effective drugs are those that contain corticosteroids. Examples of such drugs are Defislez, Korneregel.
- With leucorrhoea, scarring of the cornea is almost inevitable. To get rid of scars, the patient is given injections of potassium iodide, a little less often - ethylmorphine hydrochloride. Also, sometimes drugs with proteolytic enzymes are injected. Biogenic stimulants are often administered. All this is aimed at resorption of scars.
- Vasodilators are often used, as improved circulation promotes rapid recovery.
- Many ophthalmologists combine medications with hormonal preparations, as well as with natural products (for example, with aloe extract). The combination of such funds with physiotherapy - electrophoresis, phonophoresis is especially effective.
Important! Self-medication is strictly not recommended. The maximum that you can afford is an ointment with corticosteroids, and then only in case you can't immediately see a doctor.
Surgical intervention
If the doctor recommends surgery, you should not refuse. The procedure will be painless under general anesthesia and will take a little time. Of course, then you will have to lie in the hospital with a bandage over your eyes for some time, but the result of the difficulties endured will be a complete cure for the disease and good vision.
There are 2 types of surgical intervention:
- keratoplasty (pictured);
- operation using a laser.
Keratoplasty means tissue transplantation - donor cornea. This organ takes root well, since it does not have independent vessels. Antibodies that can reject foreign tissue (a common problem in transplants, say, kidneys) simply do not pass through the cornea. This allows surgical intervention to be successful in almost 100% of cases.
With regard to laser surgery, the surgeon uses a laser to remove the affected area from the cornea. This method is used for small lesions that can be repaired without an organ transplant. Accordingly, keratoplasty is necessary for large spots and lesions.
Important! Sometimes there are contraindications to surgery. They can be associated with the patient's age or with some special medical condition. In such cases, it remains only to wear contact lenses for cosmetic correction of opacity and to use medications to prevent the disease from progressing.
ethnoscience
In addition to traditional treatment, one should not forget about folk remedies. They can also be very effective, especially when combined with medication. Here are some good time-tested recipes.
Important! Any alternative methods of treatment should be discussed with an ophthalmologist before starting to use them. Self-medication can be fraught with aggravation of the disease, burns of the cornea of \u200b\u200bthe eye, allergies.
Treatment prognosis
The prognosis for the treatment of this ailment differs based on its stage, on the age and health of the patient, as well as on the reason for the disease.
- Small opacities somewhere in the periphery, which do not interfere with seeing, do not require serious treatment. All they need is therapy and regular medical supervision.
- Large thorns, provoked by various diseases (not "eye diseases), do not need surgical treatment if their root cause has been eliminated." If a person is cured of an illness, then ordinary medicines will help him to remove the thorn.
- Surgical intervention is required at advanced stages of the disease, as well as if the patient has an allergy or intolerance to medications. As mentioned above, the transplanted cornea is easily engrafted, and therefore the prognosis of such treatment is very positive.
- The least favorable prognosis is for leucorrhoea resulting from burns and serious injuries. If the eye was very badly affected, then it is unlikely that it will be possible to restore vision by 100%, and the treatment will be reduced to minimizing the consequences and symptoms.
Video - Corneal dystrophy. Eyesore
Important! In any situation, for any reason for turbidity, treatment will be much more successful if it is started immediately, without delaying a day after the disease was discovered.
How to take care of your eyes? Prevention of corneal opacity
Preventive measures aimed at avoiding corneal opacity will be a good prevention for other "eye" ailments. These measures include:
- protection from direct exposure to sunlight;
- protection from ultraviolet rays;
- protective equipment for professional activities (goggles, mask, etc.) - an indispensable tool for any chemist, woodcarver, welder and representatives of many other professions;
- exercises (especially necessary for those who spend a lot of time in front of a monitor or books);
- regular visits to the doctor (at least once every 6 months);
- eating foods that improve eyesight (well-known blueberries and carrots, as well as foods with vitamin A).
Products useful for vision
If a person wears contact lenses, then he should not forget to take off the lenses at night, change them at least as often as indicated in the instructions, and wash only with a special solution, without using improvised means.
Conclusion
Corneal opacity is a very serious visual pathology. It can be cured without consequences only with a timely visit to a doctor. If you let things take their course and turn to a doctor too late, visual impairment can remain with a person for life.
A careful attitude to one's own eyes, the use of protective equipment and personal hygiene is an effective prevention of corneal opacity. If you regularly visit a doctor and take good care of the visual organs, then there will be no talk of any clouding, as well as of other eye diseases.
Video - Treatment of leucorrhoea (clouding of the cornea of \u200b\u200bthe eye)
The human visual system is extremely sensitive to various adverse factors that are negatively reflected in its work. In the practice of ophthalmologists, a disease such as leukoma - opacity of the cornea - is often encountered. Pathology is accompanied by cicatricial changes in the retina, which leads to a decrease in visual acuity. This disease tends to progress in the absence of quality treatment, which can ultimately lead to complete blindness.
In the people, clouding of the cornea of \u200b\u200bthe eye is also called "thorn". According to statistics and medical observations, the disease occupies a leading position in the frequency of occurrence, is more often diagnosed in people of mature age. Thanks to the capabilities of modern ophthalmology, this pathology can be treated in several ways, the main thing is to consult a doctor in time, who can determine the cause, prescribe the necessary treatment.
Leukoma - clouding of the stratum corneum of the eye. There are several reasons for the development of pathology, but they are based on an infectious lesion of the vision system or the result of mechanical trauma. The trigger for cloudy eyes is often:
- (inflammation);
- complications after a number of infectious diseases: measles, syphilis, tuberculosis;
- , affects the cornea;
- mechanical or chemical injury;
- heredity;
- complication of previous eye surgery.
A lack of vitamin A, improper wearing of lenses or poor lens care can provoke the development of pathology. Based on the above reasons, it can be concluded that opacity of the cornea of \u200b\u200bthe eye is not an independent disease, but develops as a complication against the background of other diseases or conditions.
Human eye structure
Clinical signs
With the development of corneal opacity, its transparency decreases, pathological changes occur inside, which can be noticed with the naked eye. In addition, the shape of the cornea changes, the sensitivity and elasticity of tissues decrease. Such a defect is the final process of the inflammatory reaction with pronounced degenerative and dystrophic changes in tissues in the organ of vision.
Outwardly, cloudiness can be recognized by the presence of a gray spot on the surface, which resembles small smoke in the center of the protein. In addition, with this pathology, there are other signs:
- redness of proteins;
- photophobia;
- decrease in visual acuity up to its complete loss;
- increased tearing;
- sensation of a foreign object in the eye;
- discomfort in the eyes;
- vagueness.
The appearance of at least one of the above symptoms should be a reason for an immediate visit to an ophthalmologist. Modern diagnostic methods make it possible to recognize the disease at the earliest stage of development, to carry out the necessary treatment that will help preserve vision.

Eyesore
Kinds
In ophthalmology, corneal opacity is divided into 3 main types, each of which has its own size, opacity intensity:
- Cloud - a small grayish opacity on the cornea, which is more often present towards its center. It does not cause much discomfort to a person, does not affect vision.
- The spot is a limited high intensity haze. It can be located both in the center and at the periphery of the eye. It can affect most of the cornea, has severe symptoms, reduces vision, causes aesthetic and physical discomfort.
- Belmo is a severe type of disease with severe symptoms. It is accompanied by persistent opacity of the cornea, the formation of scars that affect most of the organ of vision. Sometimes the thorn is so large that it covers the entire eye.
In addition to the types of pathology, it is distinguished by the place of localization:
- peripheral - affects the edge of the cornea of \u200b\u200bthe eye, which causes a limitation of the field of vision (if present in the form of a cloud or spot, visual acuity is not impaired);
- central - located in the area of \u200b\u200bthe lens, often leads to blindness (at the initial stages it only causes a decrease in vision, but as it develops, it leads to complete blindness);
- total - accompanied by scarring of the central and peripheral region (refers to severe and rapidly progressing pathologies, which, in the absence of proper treatment, leads to loss of vision).
Belmo can be congenital or acquired. Congenital pathologies are quite rare, diagnosed in infancy. Acquired, appear much more often as a result of various exogenous factors on the cornea.
Video: Corneal opacity
Modern diagnostic methods
If you suspect the development of leukoma of the eye, the ophthalmologist conducts an external examination, collects an anamnesis, prescribes a number of studies, including:
- determination of visual acuity;
- Ultrasound of the organs of vision;
- biomicroscopy;
- research using the Amsler grid;
- coherence tomography.
The results of the study help the doctor get a complete picture of the disease, assess the degree of damage, make a final diagnosis, and determine the tactics of treatment.
One of the informative diagnostic methods is the Amsler grating study, which consists of the use of a special apparatus that helps to determine the degree of visual impairment. During the examination, the patient focuses on the point indicated by the doctor. If the lines inside the apparatus do not seem straight, but wavy, this is a serious sign of disorders and dystrophic changes.
What treatment does modern ophthalmology offer?
Leukoma therapy can be carried out both conservatively and surgically. In the first case, the doctor prescribes the use of eye drops, physiotherapy procedures, eye gymnastics, and gives recommendations on nutrition and lifestyle.
Medication can include the following drugs:
- anti-inflammatory drops, ointments, which contain components containing corticosteroids;
- preparations for resorption of scar tissue - ethylmorphine hydrochloride and potassium iodide;
- agents that improve blood circulation to the retina with a vasodilating effect.
The choice of a specific drug, dose, frequency and duration of admission is determined by the doctor individually for each patient. Good efficacy from the treatment can be obtained with the help of physiotherapy: electrophoresis, phonophoresis in combination with hormonal drugs or natural ingredients.
Conservative therapy is used at the earliest stages of the disease, when there are no pronounced pathological changes inside the visual system. In the case when the disease is started or drug therapy has not brought the desired result, the doctor decides to carry out the operation.
Video: Treatment of a thorn
Surgical treatment of opacification is considered more effective, since it allows you to eliminate the pathology, stop its progression, reduce the risk of complications and restore vision. Modern ophthalmology has several ways to treat leukoma of the eye:
- keratoplasty - excision of the clouded part of the cornea, with the further use of drug therapy to restore the cornea;
- transplantation - corneal transplant from a donor (allows you to completely restore vision, but problems often appear when searching for a donor, which slows down the operation);
- cosmetic tattoos - eliminate the defect itself, but do not restore visual functions;
- implantation of an artificial lens - more often carried out when the cornea is injured (does not restore vision, but relieves of constant discomfort).
It is important to understand that a small spot on the periphery of the cornea is not an indication for surgery. Such procedures are carried out only strictly according to indications and the lack of effect from conservative treatment.
If the patient has contraindications to any operation or the person himself refuses such treatment, the doctor may advise the cosmetic correction of the pathology using contact lenses.
The prognosis after treatment depends on how badly the cornea of \u200b\u200bthe eye is damaged, so everything is individual here. Doctors make every effort to preserve the patient's eyesight, eliminate aesthetic discomfort.

How to cure an eyesore
Folk remedies to help
As an adjunct therapy to the main treatment, many patients resort to alternative methods. Such treatment is not a panacea, it cannot be the basis, but it still helps to slow down the progression of the disease, improve the general condition of the patient. Consider a few effective recipes:
- Recipe number 1
You will need 10 g of onion gruel, 100 ml of hot milk. Mix, set for 8 hours, filter. From the finished solution, make lotions on the sore eye or instill 1 drop 2 times a day.
- Recipe number 2
Fir resin is instilled 1 drop into the sore eye. After that, a slight burning sensation may be present, which is the norm.
- Recipe number 3
For cooking, you need to combine honey and grain 50: 1, stir. The finished drug is applied to the affected area 2 times a day.
- Recipe number 4
It is necessary to pour 30 g of dill seeds with boiling water, put on a low heat for 20 minutes, then cool, strain and instill 3-4 drops into the conjunctiva, or use for rinsing.
These are far from all the recipes that traditional medicine offers. However, ophthalmologists are quite skeptical about such treatment, they believe that it can do more harm than good. That is why if a person has decided to carry out treatment using folk methods, it is imperative to consult with the attending physician. Self-medication can cause irreversible damage to health.
Video: What to do if the cornea is damaged
Prevention
Here are some practical tips to help reduce the risk of cloudiness:
- timely and correct treatment of all infectious diseases;
- protect eyes from ultraviolet radiation;
- exclude any contact with harmful and toxic substances;
- proper and healthy nutrition;
- give your eyes time to rest;
- use and wear contact lenses correctly, keep them clean;
- regularly perform visual exercises;
- preventive examinations by an ophthalmologist, at least once a year.
By observing the basic rules of prevention, you can reduce the risk of any ophthalmic disease, including corneal opacity. At the first symptoms of pathology, it is important not to self-medicate or wait for everything to go away on its own. The sooner a person seeks medical help, the greater the chances of full recovery and preservation of vision.

Description:
After the transferred, corneal opacities of varying severity often remain. In magnitude and intensity, corneal opacities are in the form of a cloud, a spot and a leucorrhoea.
Causes of corneal opacity:
Corneal opacity occurs after acute inflammatory eye diseases (after keratitis). In addition, corneal opacity can result from eye injuries.
Corneal opacity symptoms:
When the cornea becomes clouded, vision is impaired. The degree depends on the degree of corneal opacity. Sometimes corneal opacity is noticeable with the naked eye.
Corneal opacity treatment:
For treatment are prescribed:
Despite the age of the process, in the presence of residual inflammatory infiltration in or around the leucorrhoea, local anti-inflammatory and resorbing treatment is performed. From nonspecific anti-inflammatory drugs, corticosteroids are used in the form of eye drops: 1% cortisone suspension, 1% hydrocortisone suspension, 0.3% prednisolone solution, 0.1% dexamethasone solution 3-4 times a day. For the same purpose, instillation of a 2% solution of amidopyrine is prescribed. They also use ointments containing corticosteroids - 0.5% hydrocortisone, 0.5% prednisolone 2-3 times a day. From absorbable agents, instillations of 1-2% solutions of ethylmorphine hydrochloride are used. Every 2-3 weeks, the concentration of solutions is gradually increased to 6-8%. Apply 1-2% ethylmorphine hydrochloride ointment. Treatment courses are usually repeated. Priskol (Switzerland), divascol (Czechoslovakia), pri-dazol (Poland), tolazoline (GDR) are also prescribed in the form of instillations of a 10% solution and 10% eye ointment. Priskol is a topical vasodilator that improves blood circulation in the anterior part of the eye.
Ethylmorphine hydrochloride is also used in the form of subconjunctival injections: a 2% solution is injected at 0.2-0.3-0.4-0.5 ml at intervals every other day. Locally, instillations of a 3% solution of potassium iodide or sodium iodide, a 0.1% solution of lidase, administration of 1-2% yellow mercury ointment into the conjunctival sac are prescribed. For resorption of corneal opacities, collalisin (a proteolytic enzyme) is also used, which is injected under the conjunctiva of the eyeball at a dose of 10 KU in 0.2 ml of a 0.5% solution of novocaine. The course of treatment is 7-10 injections. Before treatment with collalizin, it is necessary to check the patient's sensitivity to the drug, for which first 1 KE is injected under the conjunctiva. In the absence of an allergic reaction within 48 hours, treatment is carried out with the above doses.
When corneal opacities are formed, for more gentle scarring, electrophoresis with hydrocortisone (0.1% solution) is prescribed for 15 minutes or phonophoresis with 0.5% hydrocortisone solution (5 minutes each) daily, 15 procedures per course. For resorption of corneal opacities, ultrasound is used at an intensity of 0.1-0.2 W / cm2 daily or every other day, a total of 15 procedures; electrophoresis with lidase through a bath electrode (32 units per procedure) every other day, per course - 15 procedures; electrophoresis with a vitreous body (ampoule solution), 3% potassium iodide solution, aloe (ampoule solution). Collalisin electrophoresis and phonophoresis are also used (50 KU per 10 ml of distilled water). Duration of electrophoresis - 10 minutes, phonophoresis - 5 minutes. The course of treatment is 10 procedures. The courses of treatment are repeated after 1.5-2 months. With repeated courses of electrophoresis, it is advisable to change the drugs.
As a resorption agent, 1-2 ml of oxygen is injected under the conjunctiva of the lower transitional fold. The procedure is repeated in 1-2 days, 10-20 injections per course. Of the general agents that promote the resorption of corneal opacities, biogenic stimulants are used (liquid aloe extract, FiBS, peloidodistillate for injection, vitreous body, peat, etc.) in the form of subcutaneous injections of 1 ml, 30 injections per course. Peat is also injected under the conjunctiva, 0.2 ml every other day, only 15-20 injections. Intramuscularly prescribed injections of lidase, 1 ml (64 AU) every other day, 10-15 injections per course. The courses of treatment are repeated 2-3 times a year. In the case of corneal opacity due to a specific process (tuberculosis,
Content of the article: classList.toggle () "\u003e expand
Clouding of the cornea or, in a popular way, leukoma (leukoma) is an ophthalmic disease characterized by scarring of the cornea. Clouding occurs due to inflammatory diseases of the eyes or mechanical damage to the mucous membrane.
The formation looks like an intense opacity of a porcelain-white hue in the form of a spot or cloud on the cornea. If untreated, the leucorrhoea darkens due to the fact that capillaries grow in it.
This is a serious disease that gradually impairs vision, until it is completely lost. Therefore, it is necessary to identify turbidity as early as possible and carry out competent treatment.
In the article you will learn everything about the opacity of the cornea of \u200b\u200bthe human eye, as well as about the treatment of leukoma (thorns).
Causes of leukoma
When clouded, the cornea loses its main property - transparency. The formation of a pearl hue over time acquires a yellow color, this is due to the fact that blood vessels grow in it and adipose tissue is formed.
The deep layers of the cornea are affected for the following reasons:
- ... Inflammatory lesion of the cornea occurs against the background of severe infectious diseases (tuberculosis, syphilis). The disease affects the superficial or deep balls of the cornea. As a rule, a thorn occurs with incorrect treatment of deep keratitis;
- Trachoma is a chronic eye disease caused by chlamydia. Over time, the likelihood of corneal infection and scarring increases;
- Eye injuries. Functional tissue is replaced by connective tissue due to mechanical trauma, burns (thermal, ultraviolet, chemical). The most dangerous are damage to the cornea by acid and alkali;
- Surgical treatment of the eyes. After surgery (for example, removal of a cataract), the likelihood of complications and cicatricial changes increases, as a result, a thorn appears in the eye. This is possible with incorrect or untimely therapy, weakened immunity;
- Genetics. Leukoma can form even during the period of intrauterine development. This happens when the fetus is exposed to chemicals or viruses that disrupt collagen production and provoke the formation of cloudiness.
Any infectious systemic disease can provoke leukemia in the absence of proper therapy.
Symptoms of the disease
Corneal opacity is manifested by characteristic signs:
- Clouding of the whites of the eyes, the damaged area turns milky or yellowish;
- Lumpy opacity with a pronounced vascular network occurs due to an infectious eye disease;
- If the thorn is smooth, matte or glossy, then it occurs for other reasons.
A person who suffers from leukoma experiences the following symptoms:
- Decreased visual acuity, which is manifested by clouding or haze in the eyes;
- ... The patient feels a burning sensation on the mucous membrane and the presence of a foreign body. This is due to increased intraocular pressure and bulging of the cornea. That is, glaucoma and thorns appear at the same time;
- Involuntary discharge of tears, painful sensations in response to light (photophobia);
- Redness of the mucous membrane of the eyes.
Depending on the form and degree of turbidity, the following types of leukoma are distinguished: spot, thorn and cloud. A spot is a formation with clear or blurred boundaries of a porcelain-white hue.
Belmo is formed after the destruction of the epithelial layer and further proliferation of connective tissue (scarring).
Peripheral spots do not affect vision, as they are located outside the pupil. The central thorn occludes the pupil, reduces visual acuity, or limits the field of view.
The total leucorrhoea completely covers the cornea, therefore, a severe decrease in vision, up to light perception, is diagnosed.
Drug treatment
To clarify the diagnosis, biomicroscopy is performed (examination of the structures of the eye using a slit lamp). This diagnostic method allows you to examine the affected area of \u200b\u200ba whitish color. Biomicroscopy allows you to assess the size and depth of the corneal lesion in order to select the appropriate treatment tactics.
In addition, the optometrist examines the patient using an ophthalmoscope. This method allows you to verify the presence or absence of pathological changes in other structures of the eye.
The main goal of therapy is to eliminate the root cause of the pathology that triggered the opacity of the cornea.
Such a plan is justified if the disease is detected at an early stage, when the speck has just appeared. In this case, the following medicines are used for treatment:
- Corticosteroids: Hydrocortisone ointment, Dexamethasone eye drops;
- For resorption of corneal opacities, electrophoresis with Lidase, aloe extract or vitreous body is used;
- To eliminate trophic ulcers, Solcoseryl is used in the form of a gel;
- Pilocarpine hydrochloride is used to stop the development of glaucoma.
When the thorn is already fully formed, the following medications are used for treatment:
- Blarapan, containing components similar to those that make up the cornea. The drug restores damaged areas;
- Lidase in the form of drops accelerates the resorption of scars. Potassium iodide has a similar effect;
- Actovegin triggers metabolic processes in the tissues of the cornea, thanks to which it regenerates faster;
- Korneregel stimulates regenerative processes in the cornea;
- Hypromellose protects the epithelial layer of the cornea, which protects and softens it;
- As part of the complex treatment of leucorrhoea, vitamins A and B2 are used.
Thus, regardless of the time of the formation of a leucorrhoea and how long the process develops, drops with glucocorticoids (Prednisolone, Cortisone, Hydrocortisone, Dexamethasone) or ointments based on hydrocortisone or prednisolone are used for treatment.
To accelerate the resorption of scars, instillations with a solution of ethylmorphine or lidase are prescribed. In addition, drops based on potassium iodide are used for treatment.
Mercury ointment is placed in the conjunctival cavity... For resorption of opacities, proteases are used, which are injected under the conjunctiva by injection.
For formed scars, electrophoresis with hydrocortisone, vitreous humor, lidase, potassium iodide, aloe extract is used. The therapeutic course is carried out with an interval of 2 months. It is recommended to change preparations for electrophoresis each time.
Surgery
With coarse leucorrhoea, drug therapy will be ineffective. In this case, it is recommended to carry out the operation. There are 2 main methods of surgical treatment for corneal opacity:
- Keratoplasty... The damaged part of the cornea is removed using microsurgical instruments and an electron microscope. The thinnest layer of the cornea is cut from the surface, which is subject to cicatricial changes. After the procedure, medications are applied;
- Donor corneal transplant... The operation is carried out using modern equipment, for example, an excimer laser. The essence of the procedure is that the damaged cornea is removed, and healthy corneal tissue of the donor is transplanted in its place.
If the thorn is outside the pupil or partially covers it, then a special cosmetic tattoo can be applied to the formation. It changes the appearance of the eye and slightly restores visual acuity.
Opacities that have formed after mechanical or mechanical impact require special attention. If the corneal tissue is damaged to such an extent that the nerve endings are damaged, then a special lens is put on the eye. It helps to eliminate pain (painful sensitivity of the eyes to light), excess tear fluid, etc. However, this device will not restore normal vision.
Folk remedies for the treatment of corneal opacities
The following recipes are used to treat a thorn at home:
- Take 70 g of eyebright, pour 1 liter of boiled water, cover and leave for 2 hours. Then filter the broth through cheesecloth and use 50 ml every half hour. Also, lotions are made from the infusion;
- Pike bile (fresh fish) is mixed with refined sunflower oil in a 2: 1 ratio. The eyes are treated with the resulting liquid twice in 24 hours;
- For instillation of eyes, water saturated with silver or copper ions is used;
- Fresh milk whey is mixed with liquid honey in a 1: 1 ratio. The agent is instilled into the eyes, 3 drops each, twice;
- Take in equal amounts cornflower, arnica, eyebright, black elderberry, fill with boiled water, leave for 2 hours. Strain the broth and apply in the form of eye drops. Also, the infusion is used for washing the eyes and applying compresses;
- Mix 4 g of liquid honey, 3 ml of fresh dandelion juice and 2 ml of onion. Pour the liquid into a glass container and store for 4 days. The finished mixture is used in the form of an ointment, which is placed into the conjunctival cavity 3 times a day;
- Take 40 g of fresh chopped dill, pour two glasses of boiling water, put in a water bath for another 5 minutes. Then strain the solution and apply in the form of drops (3 drops in each eye) twice a day.
These recipes are allowed to be used only after consultation with the doctor, as some plants and foods can cause allergies. Alternative treatment is used as part of a comprehensive treatment along with medicines.
Complications and prognosis
If the treatment was carried out late or it was illiterate, then the probability of dangerous complications increases:
- Secondary. Intraocular pressure increases, as a result, the optic nerve atrophies and visual acuity decreases;
- Strong (myopia) - the image is formed not on the retina, but in front of it due to the fact that the eyeball has an elongated shape or the rays are more focused;
- Asthenopia - eye fatigue, which quickly occurs as a result of visual work;
- - oscillatory eye movements with a high frequency, which the patient cannot control;
- - this is a pathology characterized by an imbalance of the visual axes, as a result of which the eye pupils are directed in different directions.
In most cases, complications develop if the thorn is formed as a result of traumatic damage to the cornea. In any case, all these pathologies significantly reduce visual acuity up to blindness.
The prognosis for corneal opacity depends on the severity of the scar changes, general health and the reasons that provoked the pathology.
With peripheral spots (outside the pupil), supportive therapy and observation by an ophthalmologist are necessary. Progressive thorns, which have arisen as a result of a severe infectious disease, are treated with a conservative method after the root cause has been eliminated. After a donor corneal transplant with severe opacity, the functionality of the eye is usually quickly restored.
The hardest to treat is thorns that have arisen due to injury or burns. Then everything depends on the scale of the damaged area. With extensive damage to the cornea, only symptoms can be stopped (photophobia, excess tear fluid), it is not possible to restore visual acuity.
Thus, leukoma is a serious disease that requires timely treatment. Otherwise, the likelihood of complete corneal dysfunction and loss of vision increases. That is why it is necessary to turn to an ophthalmologist in time, who will find out the cause of the pathology and prescribe competent treatment.