At the present time, medicine has many methods of examining the liver to detect diseases. These methods include palpation of the liver, which is performed by feeling the lower edge of the organ. Percussion is also used, during the procedure, the doctor begins to tap the wall of the sternum in order to determine with the help of sound phenomena malfunctions in the liver.
At the initial stages of checking the health of the liver, doctors resort to examining the organ "manually" by probing.
Why do you need percussion?
Human organs have different densities and, if you tap the chest and abdominal cavity, sounds of a different nature are formed. With the help of their analysis during percussion, doctors determine the location of the liver and disturbances in its work. One of the significant indicators is renal dullness - a part of the organ zone that is not covered by lung tissues.
When there is a lack of hepatic dullness, this may indicate pneumoperitoneum (accumulation of gas in the peritoneum). The boundaries of hepatic dullness are set by changes in percussion sounds. The sound range often ranges from clear pulmonary to dull. The definition of the upper boundary during percussion is due to the 3 features of the costal arch:
- peri-sternal;
- mid-clavicular;
- anterior axillary.
The technique for determining the lower boundary of an organ is the same. After finding it, you can identify the presence of failures in the activity of the liver. In a patient who has normal and healthy internal organs, the lower limit is established using the anterior axillary line. Then it follows through the mid-clavicular line. Along the near-sternum line on the right, the border drops by 2 centimeters from the previous mark. Along the anterior median line, it does not reach the lower line of the xiphoid process of the sternum by several centimeters (from 3 to 6), and along the peristernal line on the left, the border crosses the costal left arch.
Individual characteristics of percussion
The lower part of the organ changes based on the constitution of the body of a particular patient, and often there is a disappearance of hepatic dullness due to flatulence and the passage of intestinal loops between the liver and the diaphragm. A thin person in a normal state has a rather low location of the organ. People in the body have a higher position of the lower part (2 centimeters higher than normal).
When analyzing the result of percussion, doctors take into account not only the structure of the body, but also the age of a particular patient. In childhood, the lower limit is located quite low. This is due to the fact that in adults, the mass of the liver is 3% of the total weight, and in children - about 6%. The younger the person, the more space in the peritoneum the liver covers.
Sizing according to Kurlov
The size of the liver according to Kurlov begins to be determined in children whose age has already reached the mark of 7 years. Percussion allows you to set 3 organ sizes:
- With the help of a line crossing the middle of the clavicle and the right side of the body, the 2nd borders of the liver are determined: the lower and upper. The space between them is the 1st liver size.
- Using the median line and the differences in the sound range, the 2nd dimension is determined.
- The third is set along the diagonal of the upper and lower boundaries. Calculate the length from the midline to the costal arch (left).
Table of normal organ sizes in children and adults
Table of healthy sizes in adults according to Kurlov with percussion:
What diseases does the change in boundaries indicate?
If, during percussion, the upper border of the organ is shifted upward, this indicates such diseases:
- neoplasms of a different nature;
- cystic formations provoked by echinococcus;
- accumulation of pus under the diaphragm (subphrenic abscess);
- inflammation of the pleural sheets (pleurisy);
- high position of the diaphragm.
Conditions when the upper border is moved down develop due to:
- increased airiness of the lung tissue (pulmonary emphysema);
- prolapse of the abdominal organs (visceroptosis);
- accumulation of air or gas in the pleural space (pneumothorax).
When the lower boundary is moved up, the patient develops:
- liver atrophy;
- excessive accumulation of gas in the intestines;
- accumulation of free fluid in the peritoneum (ascites).
If percussion showed a downward movement of the lower boundary, this means that the patient suffers:
- hepatitis;
- malignant neoplasms;
- stagnant liver;
- disturbances in the work of the heart.
Why palpation?
Palpation of the liver is carried out according to the Obraztsov-Strazhesko method, which is based on the fact that the specialist palpates the lower edge of the organ with his fingers while the patient takes a deep breath. Considering that the liver is the most mobile organ in the peritoneum during breathing due to its proximity to the diaphragm, the result of palpation depends entirely on the respiratory mobility of the organ, and not on the fingers that are manipulating.
Due to the peculiarities in the structure of the human body, palpation is performed in a standing or lying position. During the manipulations, the doctor adheres to the principles of palpation. First of all, the procedure is carried out to determine the front of the organ, its consistency, shape, contour and pain. In cases where a pronounced anterior part of the liver is palpated during manipulations, this indicates both an increase in the organ and its prolapse. Since the edge of the organ may differ based on the anatomical features of each patient, and it is not always possible to feel it, liver percussion is used before the palpation procedure, which allows you to establish the location of the lower part of the organ.
What allows you to determine the palpation according to Obraztsov?
With the help of palpation according to the Obraztsov-Strazhesko method, doctors reveal the following conditions:
- organ enlargement;
- soreness and tenderness of the lower edge;
- organ surface;
- consistency;
- shape;
- edge.
Technique of the Obraztsov method - Strazhesko and procedure
To feel the liver according to Obraztsov, the patient is placed on his back and his arms are folded on his chest. The light weight of the hands helps to restrain the entrainment of the chest. The doctor with his left hand grasps the hypochondrium area on the right so that the back of the lower sternum is located on the doctor's four fingers. The thumb of the same hand, which is located on the side of the chest, is used to exert pressure. The doctor seems to be trying to connect the fingers of his left hand. With the help of this manipulation, the posterior part of the sternum is squeezed, which makes it possible to prevent its enlargement with a deep breath. If the sternum expands, the lungs put pressure on the diaphragm, and it on the liver, which causes the organ to drop significantly when inhaled.
Then the doctor resorts to the other hand and connects 4 fingers so that the pads are at the same level. The doctor tries to penetrate as deeply as possible into the hypochondrium on the right, constructing a so-called pocket. The front wall is the bottom of the costal arch on the right, and the back is the fold of the peritoneum and the fingers, which press it inward. With the help of this, the border of the liver is in the area between the costal arch and the fold, obtained thanks to the fingers.
After that, the specialist begins to press on the lower sternum using his left hand, and the patient takes a deep breath, which allows the liver to move downward. Due to the dilated lungs, it no longer fits in the constructed "pocket". The organ comes out of the pocket and bumps into the fingertips of the specialist's right hand. It is at this time that the liver is palpated and a sensation appears, which allows one to obtain information about the lower edge of the organ, the consistency and the presence of pain.
Palpation of a healthy liver
A healthy organ is palpated exclusively in a standing position and only if the doctor has a chance to deepen his fingers into the hypochondrium and feel the organ. To determine this, the person will have to lean forward. The normal liver is sometimes palpable below the arch of the ribs when it is in a lowered state. In this case, the upper border of dullness also goes down, but the lower border of the organ along the arc of the ribs is standard. When probing, a healthy liver has a good density, its edges are pointed and even, the surface is smooth, and manipulations do not cause pain.
What diseases can be detected by palpation?
 Palpation allows you to diagnose pathologies in the shape and size of the liver.
Palpation allows you to diagnose pathologies in the shape and size of the liver. In situations where the patient has a low position of the edge of the liver, this indicates:
- The prolapse of the organ, which occurs due to visceroptosis, pulmonary emphysema and subphrenic abscess. During this state, the boundaries remain unchanged, but they are not often palpable, since the organ is lowered.
- Enlargement of the organ. There is both an increase in the entire liver, and partial. Full increase is diagnosed with blood stasis, acute hepatitis, obesity, infectious processes and leukemia (malignant disease of the hematopoietic system).
I fight overweight and obesity recommend tapping the liver channel. Heart failure can provoke an increase. In this case, when probing the patient, the cervical veins will swell (Plesha symptom). Partial increase occurs due to neoplasms, purulent inflammations and cystic formations provoked by echinococci.
If the organ decreases in size, most often this indicates liver cirrhosis. In such situations, doctors rarely manage to palpate. The liver normally has a soft consistency. When a mild induration is diagnosed, symptoms of acute hepatitis are to blame. If there is a strong seal - cirrhosis, neoplasms and amyloidosis (protein metabolism disorders). Obesity, infectious processes and blood stagnation contribute to an increase in the liver, but they do not cause induration.
The normal liver edge is soft, sharp and slightly rounded. Cases when it is sharpened indicate the development of cirrhosis. The blunt border of the organ is observed with amyloidosis. In malignant neoplasms, it becomes intermittent. The surface of the liver is determined when the organ is slightly dense. Normally, the surface should be smooth. When it is granular, the patient develops cirrhosis, but if it is lumpy, cancerous tumors.
When, on palpation, the patient feels pain in the edge of the organ, this indicates perihepatitis (inflammation of the liver capsule), acute cholangitis (inflammation of the intrarenal or extrarenal bile ducts), and blood congestion due to heart failure. Subtle soreness is felt with hepatitis. With the appearance of cirrhosis and amyloidosis, the border of the liver remains painless. Pulsation of the organ is observed during tricuspid valve insufficiency (heart defect in which the valve leaf loosely closes the right atrioventricular opening). During palpation, the doctor feels a pulsation on the entire surface of the liver.
infopechen.ru
Palpation of the liver and gallbladder with the patient lying down
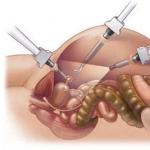
Palpation of the liver and gallbladder is carried out according to the principles of deep palpation of the abdominal organs (Fig. 432).
The patient is usually in a horizontal position, less often the study is carried out in an upright position, lying on the left side and sitting. Pay attention to the position of the doctor's hands. The left hand encloses and compresses the costal arch, limiting its movement during inhalation, which contributes to a greater displacement of the liver downward. The fingers of the right hand are set parallel to the edge of the liver, the hand lies on the stomach, obliquely, the palm is positioned above the navel.
A feature of probing the liver in the supine position is that the abdominal muscles should be relaxed as much as possible, the shoulders should be slightly pressed against the chest, the forearms and hands should be laid on the chest. The meaning of this position of the hands is to significantly limit the upper costal breathing and strengthen the diaphragmatic. This achieves the maximum downward displacement of the liver with a deep breath, its exit from the hypochondrium and greater accessibility to research.
Additional involvement of the doctor's left hand in palpation of the liver. The left hand is placed on the right lumbar region from the level of the last two ribs perpendicular to the spine and plunges into it as much as possible, which leads to a significant forward displacement of the posterior abdominal wall. The thumb of the same hand is placed on the edge of the costal arch in front. Thus, conditions are created for a significant decrease in the posterior-lateral part of the lower part of the chest, which prevents its expansion with a deep breath and contributes to a greater displacement of the liver downward from the hypochondrium. The palm of the doctor's right hand is placed flat on his stomach in the right hypochondrium with four fingers extended and the middle finger slightly bent so that the ends of the fingers are in one line parallel to the supposed or already known percussion lower edge of the liver. The fingertips should be placed 1-2 cm below the edge of the liver (costal arch) along the mid-clavicular line and a small skin fold should be made, shifting the skin down. After placing the arms, the patient is invited to take inspirations and exhalations of medium depth, during each exhalation, the fingers gradually and carefully (not roughly) sink into the depth of the right hypochondrium (down and forward under the liver). It is necessary to pay attention to the fact that during inhalation, the fingers remain submerged, resisting the rising abdominal wall. Usually 2-3 breaths are sufficient. The depth of immersion of the fingers will depend on the resistance of the patient's abdominal wall and his sensations; when moderate pain appears, the study is stopped. It is necessary to make the first immersion of the fingers shallow (about 2 cm), given that the edge of the liver lies superficially immediately behind the abdominal wall. After entering the fingers into the abdominal cavity, the subject is invited to take a calm but deep breath in the stomach. In this case, the liver descends and the anterior-lower edge of the liver falls into an artificial pocket (duplicate of the abdominal wall), formed by pressing the abdominal wall with the doctor's fingers. At the height of inspiration, with shallow immersion of the fingers, the edge of the liver slips out of the pocket and bypasses the fingers. With deep immersion, the doctor makes a movement with the fingertips up to the costal arch, sliding along the lower surface of the liver, and then along its edge.
The palpation technique is repeated several times, the degree of immersion of the fingers into the depth of the hypochondrium gradually increases. In the future, a similar study is carried out with the displacement of the doctor's palpating hand to the right and left of the mid-clavicular line. If possible, it is necessary to examine the edge of the liver along the entire length from the right to the left costal arch. If palpation fails, the edge of the liver is not caught, it is necessary to change the position of the fingers, moving them slightly down or up. In the described way, the liver can be palpated in most healthy people (up to 88% in young people).
It is not possible to palpate it for the following reasons:
- powerful development of the muscles of the abdominal wall;
- the resistance of the investigated palpation;
- obesity;
- the turn of the liver back around the frontal axis (marginal position - the lower edge of the liver is moved up, and the upper - back and down);
- an accumulation of swollen bowel loops between the abdominal wall and the anterior surface of the liver, pushing the liver back.
Most often, the edge of a normal liver is palpated at the edge of the costal arch along the mid-clavicular line, and at the height of inspiration it drops 1-2 cm below the edge of the ribs. On other vertical lines, especially along the right parasternal and anterior median, the liver is often not palpable due to strained rectus muscles. On the right anterior axillary line, the normal liver is also not palpable, but due to the depth under the costal arch. If the abdominal wall does not offer strong resistance and there is no obesity, abdominal distention, and the liver is not palpable (this is usually combined with a significant decrease in hepatic dullness), the method of palpating the liver in an upright position or in the position of the subject on the left side can be used. The principle of palpation is the same. Palpation while standing is carried out with some inclination of the patient forward, which helps to relax the abdominal muscles and lower the liver by 1-2 cm.
dyagnoz.ru
Palpation of the liver
Superficial palpation in liver disease can reveal a zone of pain in the right hypochondrium and epigastric region. Particularly strong local soreness, even with a light touch to the anterior abdominal wall in the projection area of \u200b\u200bthe gallbladder, is observed in acute cholecystitis and biliary colic. In chronic cholecystitis, only mild or moderate soreness is usually determined at the so-called point of the gallbladder: it corresponds to the projection of its bottom onto the anterior abdominal wall and is normally localized in most cases directly under the right costal arch along the outer edge of the right rectus abdominis muscle.
Palpation of the liver is performed according to the Obraztsov-Strazhesko method. The principle of the method is that with a deep breath, the lower edge of the liver falls towards the palpating fingers and then, bumping into them and sliding off them, becomes palpable. It is known that the liver, due to its close proximity to the diaphragm, has the greatest respiratory mobility among the abdominal organs. Consequently, during palpation of the liver, an active role belongs to its own respiratory mobility, and not to palpating fingers, as during palpation of the intestines.
Palpation of the liver and gallbladder is performed in the position of the patient standing or lying on his back (however, in some cases, palpation of the liver is facilitated by the position of the patient on the left side; the liver, under the influence of gravity, leaves the hypochondrium and then it is easier to feel its lower front edge). The probing of the liver and gallbladder is carried out according to the general rules of palpation, and most of all, attention is paid to the antero-inferior edge of the liver, according to the properties of which (contours, shape, soreness, consistency) they judge the physical state of the liver itself, its position and shape. In many cases (especially when the organ is omitted or enlarged), in addition to the edge of the liver, which can often be traced by palpation from the left hypochondrium to the right, it is also possible to palpate the upper anterior surface of the liver.
The examiner sits on the right next to the bed on a chair or on a stool facing the subject, puts his palm and four fingers of his left hand on the right lumbar region, and with the thumb of his left hand presses from the side and in front on the costal arch, which contributes to bringing the liver closer to the palpating right hand and, hindering expansion of the chest during inhalation, helps to enhance excursions of the right dome of the diaphragm. The palm of the right hand is placed flat, slightly bent the fingers, on the patient's stomach directly under the costal arch along the mid-clavicular line and lightly pressed with the fingertips on the abdominal wall. After such an installation of the hands, the subject is asked to take a deep breath; the liver, going down, first comes to the fingers, then bypasses them and slips out from under the fingers, that is, it is felt. The examiner's hand remains motionless all the time, the technique is repeated several times.
The position of the liver edge can vary depending on a variety of circumstances, therefore, to know where to place the fingers of the right hand, it is useful to first determine the position of the lower edge of the liver by percussion.
According to V.P. Obraztsov, a normal liver is palpable in 88% of cases. Palpation, received from the lower edge of the liver, allows you to determine its physical properties (soft, dense, uneven, sharp, rounded, sensitive, etc.). The edge of the unchanged liver, palpable at the end of a deep inspiration, 1 2 cm below the costal arch, is soft, sharp, easily tucked and insensitive.
The lower edge of a normal liver is usually palpated along the right mid-clavicular line; to the right of it, the liver cannot be felt, since it is hidden by the hypochondrium, and on the left, palpation is often difficult due to the severity of the abdominal muscles. With an increase and hardening of the liver, it can be felt along all lines. Patients with abdominal distention should be examined on an empty stomach to facilitate palpation. When fluid accumulates in the abdominal cavity (ascites), it is not always possible to palpate the liver in a horizontal position of the patient. In these cases, use the specified technique, but palpation is performed in an upright position or in the position of the patient on the left side. When a very large amount of fluid accumulates, it is previously released using paracentesis. If there is a large accumulation of fluid in the abdominal cavity, the liver is also palpated with a jerky ballot palpation. To do this, the right hand with slightly bent II IV fingers is placed in the lower right half of the abdomen, perpendicular to the alleged lower edge of the liver. With closed fingers of the right hand, jerky blows are applied to the abdominal wall and moved in the direction from the bottom up until the feeling of a dense body of the liver, which, when struck by fingers, first moves into the depths of the abdominal cavity, and then hits them and becomes palpable (a symptom of a floating ice floe).
Soreness is characteristic of inflammatory liver damage with the transition of the inflammatory process to the liver capsule or for stretching it (for example, with stagnation of blood in the liver due to heart failure).
The liver of a healthy person, if it is palpable, has a soft consistency, with hepatitis, hepatosis, cardiac decompensation, it is denser. The liver is especially dense with cirrhosis (while its edge is sharp, and the surface is smooth or small-knobby), tumor lesion of multiple cancer metastases (in these cases, sometimes the surface of the liver is coarse-knobby, corresponding to superficially located metastases, and the lower edge is uneven), with amyloidosis. Sometimes it is possible to palpate a relatively small tumor or echinococcal cyst.
The standing of the lower edge of the enlarged liver is determined in relation to the costal arch along the right anterior axillary, right near the sternum and left near-sternal lines. Palpation data clarify ideas about the size of the liver, obtained by the method of percussion.
The gallbladder is normally not palpable, since it is soft and practically does not protrude from under the edge of the liver. But with an increase in the gallbladder (dropsy, filling with stones, cancer, etc.), it becomes palpable. The probing of the bladder is carried out in the same position of the patient as palpation of the ‘liver. The edge of the liver is found and directly below it, at the outer edge of the right rectus muscle, palpation of the gallbladder is performed according to the rules of probing the liver itself. It can be most easily detected by moving the fingers across the axis of the gallbladder. The gallbladder is palpably defined as a pear-shaped body of various sizes, density and soreness, depending on the nature of the pathological process in itself or in the surrounding organs (for example, an enlarged soft-elastic bladder with blockage of the common bile duct by a tumor - a sign of Courvoisier - Terrier; bumpy bladder with neoplasms in its wall, with overflowing stones, with wall inflammation, etc.). The enlarged bubble is mobile during breathing and makes pendulum-like movements. The mobility of the gallbladder is lost with inflammation of the peritoneum covering it, pericholecystitis. With cholecystitis and gallstone disease, sharp pain and reflex tension of the muscles of the anterior abdominal wall in the right hypochondrium make palpation difficult.
This method of palpation of the liver and gallbladder is the simplest, most convenient and gives the best results. The difficulty of palpation and, at the same time, the consciousness that only it allows one to obtain valuable data for diagnosis, forced the search for the best method of palpation. Various techniques are proposed, which are mainly reduced to various positions of the examiner's hands or changing the position of the examiner in relation to the patient. However, these methods have no advantages when examining the liver and gallbladder. The point is not in the variety of techniques, but in the experience of the researcher and the systematic implementation of a plan for the study of the abdominal cavity as a whole.
Liver percussion
The percussion method allows you to determine the boundaries, size and configuration of the liver. The upper and lower boundaries of the liver are determined by percussion. Distinguish the upper boundaries of two types of hepatic dullness: relative dullness, which gives an idea of \u200b\u200bthe true upper border of the liver and absolute dullness, i.e. the upper border of the area of \u200b\u200bthe anterior surface of the liver, which is directly adjacent to the chest and is not covered by the lungs. In practice, they are limited to determining only the boundaries of the absolute dullness of the liver, since the position of the upper limit of the relative dullness of the liver is variable and depends on the size and shape of the chest, the height of the right dome of the diaphragm. In addition, the upper border of the liver is very deeply hidden under the lungs, and the upper border of the relative dullness of the liver is difficult to determine. Finally, in almost all cases, the enlargement of the liver occurs mainly from top to bottom, as judged by the position of its lower edge.
Percussion of the liver is carried out in compliance with the general rules of topographic percussion. To determine the upper limit of the absolute dullness of the liver, quiet percussion is used. Percussion from top to bottom along vertical lines, as in determining the lower boundaries of the right lung. The boundaries are found in contrast between a clear lung sound and a blunt sound from the liver. The found border is marked with dots on the skin along the upper edge of the plessimeter finger along each vertical line. Normally, the upper limit of the absolute dullness of the liver is located along the right peri-sternal line at the upper edge of the VI rib, along the right mid-clavicular line on the VI rib and along the right anterior axillary line on the VII rib, i.e., the upper limit of the absolute dullness of the liver corresponds to the position of the lower edge right lung. In the same way, it is possible to establish the position of the upper border of the liver and behind, but usually they are limited to determining only along the indicated three lines.
Determination of the lower limit of the absolute dullness of the liver presents some difficulty due to the proximity of the hollow organs (stomach, intestines), which give high tympanitis during percussion, concealing the hepatic sound. With this in mind, you should use the quietest percussion, or even better, use direct percussion with one finger according to the Obraztsov method. Percussion of the lower border of the absolute dullness of the liver according to Obraztsov Strazhesko begins in the region of the right half of the abdomen along the right anterior axillary line in the horizontal position of the patient. The finger plessimeter is placed parallel to the intended position of the lower edge of the liver and at such a distance from it that a tympanic sound is heard when striking (for example, at the level of the navel or below). Gradually moving the plessimeter finger upward, they reach the border of the transition of the tympanic sound into an absolutely stupid one. In this place, along each vertical line (right mid-clavicular line, right parasternal line, anterior midline), and with a significant increase in the liver and along the left parasternal line, a mark is made on the skin but the lower edge of the plessimeter finger
When determining the left border of the absolute dullness of the liver, the finger-plessimeter is set perpendicular to the edge of the left costal arch at the level of VIII IX ribs and percussed to the right directly under the edge of the costal arch to the point of transition of the tympanic sound (in the Traube space) into the blunt one.
Normally, the lower limit of the absolute dullness of the liver in the horizontal position of a patient with a normosthenic chest shape passes in the right anterior axillary line on the X rib, along the mid-clavicular line along the lower edge of the right costal arch, along the right circum-sternal line 2 cm below the lower edge of the right costal the arc, along the anterior median, line 3-6 cm from the lower edge of the xiphoid process (at the border of the upper third of the distance from the base of the xiphoid process to the navel), does not extend to the posterior midline on the left. The position of the lower edge of the liver and normally can be different depending on the shape of the chest, the constitution of a person, but this is mainly reflected only at the level of its position along the anterior midline. So, with a hypersthenic chest, the lower edge of the liver is located slightly above the specified level, and with an asthenic chest it is lower, approximately in the middle of the distance from the base of the xiphoid process to the navel. Displacement of the lower edge of the liver down by 1 - 1.5 cm is noted in the vertical position of the patient. With an increase in the liver, the border of the location of its lower edge is measured from the edge of the costal arch and the xiphoid process; the border of the left lobe of the liver is determined along the right periosternal line downward from the edge of the costal arch and to the left of this line (along the costal arch).
The obtained data of liver percussion allow to determine the height and size of hepatic dullness. For this, the vertical lines measure the distance between the two corresponding points of the upper and lower boundaries of the absolute dullness of the liver. This height is normally 10 - 12 cm along the right anterior axillary line. 9-11 cm along the right mid-clavicular line, and 8-11 cm along the right peri-sternal line.It is difficult to determine the percussion zone of liver dullness from behind (it merges with the zone of dull sound formed by a thick layer of lumbar muscles, kidneys and pancreas), but sometimes it is possible in the form of a strip 4-6cm wide. This avoids the erroneous conclusion about the enlargement of the liver in those cases when it is lowered and comes out from under the right costal arch, and also slightly turned anteriorly around its axis, then the band of dull sound becomes narrower behind.
Liver percussion according to Kurlov. With percussion of the liver according to Kurlov, the following three sizes are determined: the first size along the right mid-clavicular line from the upper to the lower border of the absolute dullness of the liver (normal 9 11 cm), the second size along the anterior midline from the upper border of the liver to the lower (normal 7 9 cm), the third dimension along the edge of the costal arch (normally 6 8 cm).
Determination of the percussion boundaries of the liver and its size is of diagnostic value. However, the displacement of the upper border (up or down) is more often associated with extrahepatic changes (high or low standing of the diaphragm), the presence of a subphrenic abscess, pneumothorax, exudative pleurisy). Only with echinococcosis and liver cancer, its upper border can move upward. The upward displacement of the lower border of the liver indicates a decrease in its size, but it can also be noted with flatulence and ascites, pushing the liver upward. Displacement of the lower border of the liver downward is observed, as a rule, with an increase in the organ as a result of various pathological processes (hepatitis, cirrhosis, cancer, echinococcus, blood stagnation in heart failure, etc.), but sometimes it is explained by the low standing of the diaphragm. Systematic observation of the percussion boundaries of the liver with a change in the height of hepatic dullness allows one to judge the increase or decrease of this organ during the course of the disease.
The gallbladder is usually not detected percussion, however, with a significant increase, it can be determined using very quiet percussion.
Percussion is used not only to determine the size of the liver and gallbladder (topographic percussion), but also to assess their condition: percussion (cautious) on the surface of the enlarged liver or over the area of \u200b\u200bthe gallbladder causes painful sensations in inflammatory processes (hepatitis, cholecystitis, pericholecystitis, etc. etc.). Beating (succusio) along the right costal arch also causes pain in diseases of the liver and biliary tract, especially in cholelithiasis (Ortner's symptom).
Palpation of the spleen
Palpation of the spleen is performed with the patient lying on his back or on his right side. In the first case, the patient lies on a bed with a low headboard, his arms are extended along the body, his legs are also extended. In the second case, the patient is placed on the right side, his head is slightly tilted forward to the chest, the left arm, bent at the elbow joint, lies freely on the front surface of the chest, the right leg is extended, the left is bent at the knee and hip joints. In this position, maximum relaxation of the abdominal press is achieved and the spleen is closer to the front. All this facilitates its determination by palpation, even with a slight increase. The doctor sits to the right of the patient, facing him. The doctor places his left hand on the left half of the patient's chest between the VII and X ribs along the axillary lines and squeezes it somewhat, limiting its movement during breathing. The doctor places his right hand with slightly bent fingers on the anterolateral surface of the patient's abdominal wall at the edge of the costal arch, at the junction of the end of the X rib with it, or, if the examination data and preliminary percussion suggest an enlargement of the spleen, at the alleged location of its anteroinferior edge. Then, as the patient exhales with his right hand, the doctor slightly presses the abdominal wall, forming a pocket; then the doctor invites the patient to take a deep breath. At the moment of inhalation, if the spleen is palpable and it is carried out correctly, the spleen, moving downward by the descending diaphragm, with its anteroposterior edge approaches the fingers of the doctor's right hand, rests against them and slips under them as it moves further. This technique is repeated several times, trying to explore the entire palpable edge of the spleen. At the same time, attention is paid to the size, soreness, density (consistency), shape, mobility of the spleen, determine the presence of cuttings on the anterior edge. One or more notches on the anterior margin, characteristic of the spleen, are determined at its high magnification. They distinguish the spleen from other enlarged abdominal organs, such as the left kidney. With a significant increase in the spleen, it is also possible to examine its anterior surface, emerging from under the edge of the costal arch.
Normally, the spleen cannot be felt. It becomes accessible to palpation only with significant omission (rarely with an extreme degree of enteroptosis), most often with an increase. An enlarged spleen is observed in some acute and chronic infectious diseases (typhoid fever and relapsing fever, Botkin's disease, sepsis, malaria, etc.), cirrhosis, thrombosis or compression of the splenic vein, as well as in many diseases of the hematopoietic system (hemolytic anemias, thrombocytopenic purpura, acute and chronic leukemia). A significant increase in the spleen is called splenomegaly (from the Greek. Splen - spleen, megas - large). The greatest increase in the spleen is observed in the final stage of chronic myeloid leukemia, in which it often occupies the entire left half of the abdomen, and with its lower pole goes into the small pelvis.
In acute infectious diseases, the density of the spleen is low; especially soft, doughy consistency of the spleen with sepsis. With chronic infectious diseases, liver cirrhosis and leukemia, the spleen becomes dense; it is very dense with amyloidosis.
In most diseases, palpation of the spleen is painless. It becomes painful with a splenic infarction, perisplenitis, and also in the case of a rapid increase due to stretching of the capsule, for example, with stagnation of venous blood in it during splenic vein thrombosis. The surface of the spleen is usually even, the unevenness of its edge and surface is determined with perisplenitis and old heart attacks (there are retractions), the tuberosity of its surface is observed with syphilitic gummas, echinococcal and other cysts and extremely rare tumors of the spleen.
The mobility of the spleen is usually quite significant; it is limited to perisplenitis. The sharply enlarged spleen remains immobile during breathing, but it is usually still possible to displace it by hand during palpation. Often, with leukemia, not only the spleen increases, but also the liver (due to metaplasia), which is also examined by palpation.
Spleen percussion
In the study of the system of hematopoietic organs, percussion is of limited importance: it is used only to roughly determine the size of the spleen. Due to the fact that the spleen is surrounded by hollow organs (stomach, intestines) that contain air and give a loud tympanic sound during percussion, this method cannot accurately determine its size and boundaries.
Percussion is performed with the patient standing or lying on the right side. You need to perkutate very quietly, from clear sound to dull; it is best to use the Obraztsov method. To determine the diameter of splenic dullness, percussion is performed along a line located 4 cm lateral to the left costal-articular line (this line connects the sternoclavicular junction with the free end of the XI rib). Normally, splenic dullness is defined between the IX and XI ribs: its size is 4-6 cm. The length of the spleen extends medial to the costal-articular line; percussion size of the dullness of the longitudinal spleen is 6-8 cm
www.studfiles.ru
Functions of the liver tissue
 The structures of this body carry out:
The structures of this body carry out:
- Bile production.
- Neutralization of toxic and foreign substances that have entered the body.
- Metabolism of nutrients (represented by vitamins, fats, proteins and carbohydrates).
- The accumulation of glycogen, which is the main form of glucose storage in the human body. Deposited in the cytoplasm of the liver cells, glycogen is an energy reserve, which, if necessary, can quickly resume an acute lack of glucose.
Painful sensations, as a rule, appear together with the enlargement of the organ and the stretching of the capsule provoked by it. In particular, the duration of the incubation period for hepatitis of viral etiology can be at least six months.
Clinical symptoms are still absent at this stage, but pathological changes in the structures of the liver are already taking place.
The first task of the doctor is a thorough collection of information, including the analysis of complaints and an assessment of the general condition of the patient. The next stage of diagnosis is a physical examination of the patient, which requires the mandatory performance of percussion and palpation of the liver.
These diagnostic techniques, which do not take much time and do not require any preliminary preparation of the patient, help to establish the true size of the affected organ, which is extremely important for the timely diagnosis and appointment of the correct treatment tactics.
Given the high prevalence of diseases leading to liver damage, the problem of their timely diagnosis continues to be relevant today. The most significant contribution to the development of methods for palpation and percussion studies of the liver was made by therapists Obraztsov, Kurlov and Strazhesko.
Percussion
The percussion method, which allows you to establish the location, condition and various kinds of disturbances in the functioning of internal organs, consists in tapping the abdominal cavity or chest. The varied nature of the sounds arising from this is due to the different density of internal organs.
A preliminary diagnosis depends on the doctor's ability to correctly analyze the information obtained during the performance of percussion.
There are two types of percussion:
- Direct, consisting in the implementation of tapping on the surface of the chest or the wall of the abdominal cavity.
- Mediocre, performed using a pessimeter, the role of which can be played by a special plate (metal or bone) or the fingers of the doctor himself. By constantly changing the amplitude of percussion manipulations, an experienced specialist is able to determine the functional abilities of internal organs lying at a depth of seven centimeters. The results of a percussion examination can be influenced by factors such as: the thickness of the anterior abdominal wall, the accumulation of gas or free fluid in the abdominal cavity.
In liver percussion, it is clinically important to determine the absolute dullness of those parts of it that are not covered by lung tissues. Determining the boundaries of the organ under study, the doctor is guided by a change in the nature of percussion sounds, the range of which can vary from clear (pulmonary) to dull.
To determine the upper and lower border of the liver, the specialist uses three vertical lines as a visual reference:
- anterior axillary;
- peri-sternal;
- median-clavicular.
In a person with a normosthenic physique and no external signs of damage to internal organs, a site of absolute dullness can be detected using the anterior axillary line: it will be localized on the right side, at about the level of the tenth rib.
The next landmark, the mid-clavicular line, will indicate that the liver border continues along the lower edge of the right costal arch. Having reached the next line (right peri-sternal), it will go down a couple of centimeters below the mark just mentioned.
At the point of intersection with the anterior midline, the border of the organ does not reach the end of the xiphoid process by a few centimeters. At the point of intersection with the peri-sternal line, the border of the liver, having moved to the left half of the body, reaches the level of the left costal arch.
When analyzing the results of percussion, it is imperative to take into account the patient's age, since in small patients, all boundaries are shifted downward.
So, in an adult patient, the liver accounts for no more than 3% of the total body weight, while in a newborn baby, this figure is at least 6%. Thus, the younger the child, the more place in his abdominal cavity is occupied by the organ of interest.
The video shows the method of liver percussion according to Kurlov:
Dimensions according to Kurlov
The essence of the Kurlov method, designed to determine the size of the liver, is as follows: the boundaries and dimensions of this organ are revealed using percussion - diagnostic manipulation, which boils down to tapping this organ and analyzing the sound phenomena that arise in this case.
Due to the high density of the liver and the lack of air in its tissues, dull sounds occur during percussion; when tapping a part of an organ covered by lung tissue, the percussion sound is significantly shortened.
Kurlov's technique, which is the most informative way to determine the boundaries of the liver, is based on identifying several points that allow us to indicate its true size:
- First point, denoting the upper border of hepatic dullness, should be at the lower edge of the fifth rib.
- The second the point corresponding to the lower border of hepatic dullness is localized either at the level or one centimeter above the costal arch (relative to the mid-clavicular line).
- Third point should correspond to the level of the first point (relative to the front midline).
- Fourth the point that marks the lower border of the liver is usually located at the border of the upper and middle third of the segment between the navel and the xiphoid segment.
- The fifth the point denoting the lower edge of the wedge-shaped tapering organ should be located at the level of the seventh to eighth rib.
Having outlined the boundaries of the location of the above points, they begin to determine the three sizes of the investigated organ (this technique is usually used in relation to adult patients and children over seven years old):
- The distance between the first and second points is the first dimension. Its normal value in adults ranges from nine to eleven, in preschool children - six to seven centimeters.
- The second dimension, determined by the difference in the nature of percussion sounds, gives the distance between the third and fourth points. In adults, it is eight to nine, in preschoolers, it is five to six centimeters.
- The third is oblique - the size is measured diagonallyconnecting the fourth and fifth points. In adult patients, it is normally seven to eight, in children - no more than five centimeters.
Norms in children and adults
 In modern clinics, the results obtained during palpation and liver percussion can be clarified using high-tech equipment used for ultrasound, magnetic resonance imaging and computed tomography.
In modern clinics, the results obtained during palpation and liver percussion can be clarified using high-tech equipment used for ultrasound, magnetic resonance imaging and computed tomography.
All these procedures provide comprehensive information about the boundaries, size, volume of the investigated organ and about possible violations in its work.
The measurement of the right and left lobes of the liver is carried out separately, focusing on three main indicators: oblique vertical size, height and thickness.
- Anteroposterior size (thickness) of the left lobe of the organ in a healthy adult should not exceed eight centimeters, the right - twelve.
- Craniocaudal size (height) of the right lobe can fluctuate between 8.5-12.5 cm, the left - 10 cm.
- Oblique vertical dimension value for the right lobe of the organ, it is normally fifteen centimeters, for the left - no more than thirteen.
The liver parameters of a child differ significantly from those of an adult. The size of both its lobes (together with the diameter of the portal vein) is constantly changing as his body grows.
For example, the length of the right lobe of the liver in a one-year-old child is six, the left lobe is three and a half centimeters, the diameter of the portal vein can be from three to five centimeters. By the age of fifteen (it is at this age that the growth of the gland ends), these parameters are respectively: twelve, five, and from seven to twelve centimeters.
Preparation for probing
In medical institutions in Russia, probing of the hepatic structures in adult patients and children is most often performed according to the classical Obraztsov-Strazhesko method. Called bimanual palpation, this technique is based on feeling the lower edge of the liver while taking a deep breath.
Before conducting this study, the doctor must properly prepare the patient (especially a small child) by convincing him to completely relax, relieving tension from the abdominal muscles. Given the high soreness of the affected organ, this is not at all easy to do.
Feeling of the liver can be performed both in the vertical and horizontal position of the patient, however, having taken a lying position, he will feel more comfortable. This statement is especially true of young children.
- Before performing palpation of the liver, the specialist should position himself on the right side of the patient, facing him.
- The patient is asked to lie on his back (on a couch with a slightly raised headboard). His forearms and hands should be on his chest; legs can be straightened or bent.
- The palpating specialist's left hand should fix the lower part of the patient's right half of the chest. Holding the costal arch and thereby limiting its excursion at the time of inhalation, the doctor provokes a greater downward displacement of the examined organ. The palpating (right) hand is laid flat at the level of the navel on the right half of the anterior abdominal wall, slightly to the side of the outer edge of the rectus muscle. The middle finger of the right hand should be slightly bent.
Technique for performing palpation of the liver
 Examining the patient's liver, the doctor uses deep palpation techniques applied to the abdominal organs.
Examining the patient's liver, the doctor uses deep palpation techniques applied to the abdominal organs.
For palpation, the patient most often takes a recumbent position, much less often it is performed with an upright body position.
Some specialists sit their patients or place them on their left side before palpation. Let's consider several palpation techniques in more detail.
- Palpation of the liver, carried out in the patient's lying position, is performed synchronously with the patient's breathing (a detailed description of the patient's posture and the position of the doctor's hands is given in the previous section of our article). In the phase of his exhalation, the doctor plunges the palpating hand into the patient's abdominal cavity, holding it perpendicular to the anterior abdominal wall and parallel to the edge of the liver.
Thanks to the correct preparation of the patient, the doctor manages to achieve the maximum displacement of the studied gland downward during a deep breath and its exit from the hypochondrium, which makes the organ more accessible for research.
During the inspiratory phase, the palpating hand moves forward and upward, forming a skin fold called an "artificial pocket". At the moment of a very careful and gradual immersion of the fingers deep into the abdominal cavity, the doctor asks the patient to take slow inhalation and exhalation of medium depth.
With each exhalation, the researcher's fingers steadily move down and slightly forward - under the gland under study. At the moment of inhalation, the doctor's fingers, resisting the rising abdominal wall, remain submerged in the right hypochondrium.
After two or three breathing cycles, contact is achieved with the edge of the organ being examined, thanks to which the specialist can obtain information about the outlines, boundaries, dimensions and quality of its surface.
- The edge of a healthy, painless gland with a smooth surface and a soft elastic consistency should be located at the level of the costal arch.
- The prolapse of the liver entails a displacement and its upper border, determined during percussion. This phenomenon usually accompanies an enlargement of the gland that occurs in patients suffering from acute and chronic hepatitis, obstruction of the bile ducts, cirrhosis, cysts and neoplastic lesions of the liver.
- Congestive liver has a soft texture and a sharp or rounded edge.
- Patients with cirrhosis or chronic hepatitis have a gland with a denser, sharper, painful, and uneven edge.
- The presence of a tumor provokes the formation of a scalloped edge.
- In patients with rapidly developing hepatoma (primary malignant tumor of the examined organ) or the presence of metastases, palpation reveals the presence of an enlarged dense liver with large nodes on the surface.
- The presence of decompensated cirrhosis is evidenced by the small size of a significantly hardened organ with a tuberous surface. In this case, palpation is extremely painful.
- The granular surface of the affected organ is observed with the development of an abscess and in patients suffering from syphilis or atrophic cirrhosis.
- If the rapid decrease in the liver continues some time later, the doctor may make an assumption about the development of severe hepatitis or massive necrosis.
The above-described palpation technique is used several times, gradually increasing the depth of immersion of the fingers into the hypochondrium. If possible, it is advisable to explore the edge of the organ of interest to us along its entire length.
If, despite all efforts, it is not possible to find the edge of the gland, it is necessary to change the position of the fingers of the palpating hand, slightly moving them up or down. This method can be used to palpate the liver in almost 90% of perfectly healthy people.
After the completion of the palpation procedure, the patient should be held in a supine position for a while, and then gently and slowly help him to rise. Elderly patients who have undergone this procedure are recommended to take a sitting position for a while: this will prevent the occurrence of dizziness and other negative consequences.
- Palpation of the liver is also possible in a patient sitting in a sitting position. For maximum relaxation of the abdominal muscles, he should lean forward slightly, resting his hands on the edge of a hard chair or couch.
Having reached the back wall, the specialist asks the patient to inhale slowly and deeply. At this moment, the lower surface of the examined organ will lie on the doctor's palm, giving him the opportunity to carefully feel its surface. By slightly bending the fingers and making sliding movements with them, the specialist can assess the degree of elasticity of the organ, the sensitivity and nature of its edge and lower surface.
Palpation, carried out in a sitting position (unlike the above-described classical method, which makes it possible to touch the liver only with the very tips of the fingers), allows the doctor to feel the gland of interest to us with the entire surface of the terminal phalanges, endowed with maximum sensitivity for a person.
- In patients with severe ascites (a pathological condition accompanied by the accumulation of free fluid in the abdominal cavity), it is not always possible to palpate the liver by the methods described above. In such cases, specialists use the technique of jerky (or "ballot") palpation.
Squeezing together three fingers of the right hand (second, third and fourth), the doctor places them on the wall of the abdomen - above the site of the liver - and makes a series of short jerky movements directed into the abdominal cavity. In this case, the immersion depth of the fingers should be from three to five centimeters.
Having started the study from the lower third of the abdomen, the doctor gradually, adhering to special topographic lines, moves to the liver.
At the moment of hitting it, the researcher's fingers feel the presence of a dense body that easily plunges into the ascitic fluid and soon returns to its previous position (this phenomenon is called the “floating ice” symptom).
A jerky palpation can also be used in patients who do not have ascites, but have an enlarged liver and a very weak abdominal wall, in order to detect the edge of the affected organ.
Having tightly squeezed two or three fingers on the right hand, the doctor begins to perform light jerky or sliding movements downward from the end of the xiphoid process and from the edge of the costal arch. When colliding with the liver, the fingers will feel resistance, in the place where it ends, the fingers, without encountering resistance, will simply fall deep into the abdominal cavity.
The video shows the method of palpation of the liver according to Obraztsov-Strazhesko:
gidmed.com
Palpation according to the Obraztsov-Strazhesko method allows you to determine:
Increased liver size;
Sensitivity, soreness of the lower edge of the liver;
The surface of the liver (smooth, uneven, bumpy, with nodes);
Liver consistency (soft, dense, stony density);
The edge of the liver (even, uneven, pointed, rounded, soft, dense, painful)
EXHALATION

Normal the liver is not palpable or the edge of the liver is palpable, painless, soft consistency.
With hepatitis the liver is enlarged, painful, of a denser consistency.
With cirrhosis - the liver is dense, usually painless, the edge is sharp, the surface is smooth or small.
With congestive heart failure in a large circle of blood circulation - the liver is enlarged, soft consistency, the edge is rounded, painful on palpation, Plesha symptom may be detected
INHALATION

Jogging Ballot Palpation Method (used for large ascites): light jerky blows are applied to the abdominal wall from the bottom up; - the liver is felt as a "floating ice"
Palpation of the liver is made as follows. The patient lies on his back with outstretched legs and arms along the body, the head is low. The patient should breathe deeply through the open mouth (relaxation of the anterior abdominal wall is achieved). Palpation is performed with the right hand. The doctor places the palm and four fingers of his left hand on the right lumbar region, trying to move the posterior abdominal wall forward. With the thumb of the left hand, the doctor presses the lower ribs in front, preventing the expansion of the chest during inhalation. This brings the liver closer to the fingers of the right hand. The palm of the right hand is placed flat with the last four fingers extended with the third slightly bent (the ends of the fingers form a straight line) in the patient's right hypochondrium at the level of the previously found lower border of the liver along the mid-clavicular line. On exhalation, the hand sinks over the costal edge. On a deep breath, the lower edge of the liver, pressed downward by the diaphragm, enters the space between the costal arch and the doctor's hand and then goes around the doctor's fingers and slides down under them. At this point, the consistency, nature and soreness of the lower edge of the liver should be determined.
With ascites, severe flatulence, when the liver is pushed up in the supine position, it is advisable to palpate the lower edge of the liver with the patient upright. The patient should stand slightly leaning forward and breathe deeply. The palpation technique does not change.
Low location of the liver edge occurs when:
- omissionliver (hepatoptosis) occurs in visceroptosis, pulmonary emphysema, effusion pleurisy, subphrenic abscess, while the edge of the liver does not change, but it is not always possible to palpate it, because the liver deviates down and back;
- increasingits size, can affect both the entire liver (blood stagnation, acute hepatitis, obesity, infections, leukemia, amyloidosis) and individual parts (tumors, abscesses, echinococcus).
Downsizing liver is usually observed with cirrhosis. In this case, palpation is not always possible.
The liver normally has a soft consistency. Moderate compaction is observed in acute hepatitis, significant - in cirrhosis, neoplasms, amyloidosis. Blood stasis, obesity, infections, causing enlargement of the liver, do not lead to its hardening.
The nature of the edge of the liver:
- normally sharp or slightly rounded;
- with cirrhosis - sharpens;
- with stagnation of blood, non-alcoholic fatty liver disease, amyloidosis - dull, rounded;
- with cancer - uneven.
Surfacethe liver can be assessed when the liver is hardened. It is normally smooth. With cirrhosis, it becomes uneven, granular, with focal processes in the liver - bumpy.
Sorenessthe edges of the liver appears with perihepatitis, acute cholangitis, blood stasis against the background of decompensation of heart failure, to a lesser extent - with acute hepatitis. With cirrhosis, amyloidosis, the liver is painless.
Liver pulsation appears with insufficiency of the tricuspid valve of the heart. In this case, the pulsation is felt over the entire surface, in contrast to the transmitting pulsation of the abdominal aorta, when the pulsation is felt along the midline.
Palpation is a method used in medicine and consists in examining the patient using the fingers and palms. It consists in a tactile sensation that appears in the doctor during the pressure of the fingers or the entire palm on the examined organ. Using this diagnostic method, you can find out:
- location of organs;
- their size and shape;
- density and mobility;
- soreness;
- accumulation of gas in the intestines
Palpation is superficial and deep. The first one is carried out with one palm or two at once, which the doctor places flat on the area of \u200b\u200bthe skin, joints, heart. The second type is carried out using special techniques (for example, sliding palpation), examining the state of the stomach, spleen, liver and other organs.
Why is liver palpation performed?
With a prolapse or pathological enlargement of an organ with the help of palpation, the doctor determines the lower limit, the outlines of the edge of the liver, the presence of pain and pathological processes. Palpation of the liver is carried out according to the general rules for palpation of organs located in the abdominal cavity. First, a superficial palpation of the liver is performed, after which a deep, sliding one.
When performing this procedure, the doctor's attention is focused on the lower front part of the liver. The condition of the entire liver is also determined by its condition.
How is the liver palpated?
 The palpation procedure is carried out both with the patient lying down and standing. In the supine position, the lower part of the liver is under the ribs, and in the standing position the organ is shown 1.5 - 2 cm from under the ribs, which makes it possible to examine it. The liver is very well palpated in the patient's standing position, when organ pathology is observed. In this case, the liver is enlarged and compacted. However, the main examination is performed in the supine position. Palpation of the liver is performed with the patient lying on his back, the head should be slightly raised, and the legs should not be fully bent at the knees or straightened. In order to limit the mobility of the chest during inhalation, and also to relax the abdominal muscles, the patient must put his hands on his chest. After that, the doctor starts the procedure.
The palpation procedure is carried out both with the patient lying down and standing. In the supine position, the lower part of the liver is under the ribs, and in the standing position the organ is shown 1.5 - 2 cm from under the ribs, which makes it possible to examine it. The liver is very well palpated in the patient's standing position, when organ pathology is observed. In this case, the liver is enlarged and compacted. However, the main examination is performed in the supine position. Palpation of the liver is performed with the patient lying on his back, the head should be slightly raised, and the legs should not be fully bent at the knees or straightened. In order to limit the mobility of the chest during inhalation, and also to relax the abdominal muscles, the patient must put his hands on his chest. After that, the doctor starts the procedure.
It should be noted: if a large amount of fluid accumulates in the abdominal cavity, then palpation of the liver is either difficult, or the implementation of this procedure becomes completely impossible.
In such a situation, other examination methods are used to diagnose the disease.
What diseases can be detected?
If the liver is in normal condition, then it does not protrude from under the ribs and palpation cannot be performed. If the liver protrudes, then pathological processes occur in it or organ prolapse is observed.
Damage to the ligaments of the liver, which appeared due to the fact that a person fell to his feet from a height or performed parachute jumps, is the reason for the omission of the liver.
If there were no falls, then the protruding edge of the liver speaks not of the prolapse of the organ, but of its increased size. The reasons for this phenomenon can be the following diseases and conditions:
- liver diseases: jaundice, cirrhosis, oncological processes;
- the negative processes occurring, due to which it is difficult to remove bile;
- heart failure;
- various blood diseases;
- acute, as well as chronic infections and other diseases.
If palpation of the liver determines a sharp, wavy, compacted edge, but completely painless, then these symptoms indicate a possible cirrhosis of the liver. If the edge of the organ is thickened, hard, and the surface is uneven, and pain may also not be observed, then liver cancer is suspected. A very dense organ consistency is also found in amyloidosis.
The presence or absence of pain on palpation of the liver is explained by the rapid development of pathological changes in the organ.
The roughness of the surface, observed in the form of a local bulging, is observed with a focal disorder in the organ. Such symptoms are typical for the following diseases:
- echinococcosis;
- syphilitic gumma;
- abscess.
One last tip: if you have any suspicions about liver disease, do not postpone a visit to the doctor. Using not only the liver palpation method, but also other forms of examination, the doctor will make an accurate diagnosis and prescribe treatment.
We suggest that you familiarize yourself with the article on the topic: "The liver: location in the body, how to feel it" on our website dedicated to the treatment of the liver.
Where the human liver is located and why it is needed, not everyone knows. It is very important to know the location of this organ, because sooner or later, the liver will make itself felt and ask for help.
The liver is located under the diaphragm itself in the abdominal part in the right hypochondrium. However, to be a little more precise, it takes up so much space in the body that it would be more correct to note that most of the organ is located on the right side of the body (right lobe). The left lobe of the organ is much smaller than the right and is located on the left side. The lower borders of the organ are covered with ribs, and the upper edges are in line with the nipples.
As the largest and largest organ in the human body, the liver is responsible for many important functions and is associated with all organs of the gastrointestinal tract. The location of the liver, its mass and size already indicate that the body cannot exist without it. The organ filters the blood, controls all metabolic processes, is a powerful and only neutralizer of harmful substances that enter the body in different ways every day.
On any medical pictures you can see which side is
human liver
It is not only our protector against bacteria and viruses, it is also a voluminous reservoir of "reserve" blood. It is thanks to this reserve that a person has the opportunity not to die immediately from loss of blood in case of accidents; the body carefully monitors that the blood is enriched with useful enzymes that are carried further through the body.
The location of the liver in a person is such that another digestive organ can talk about its problems. This organ is the pancreas, which is very insidious and specific. The liver produces bile, which is stored in the gallbladder. When a signal is received that the process of digestion has begun, bile is directed along the ducts and tubules to the duodenum. There it meets with pancreatic juice produced by the pancreas. Normally, these two components, synchronously working in pairs, but if there are violations in the work of the organ, the natural outflow of bile is disturbed, this is reflected in the pancreas. Bile may not get to its destination due to poor patency of the ducts, or it can get into the gland itself.
Liver percussion is performed in a horizontal position of the patient. The finger plessimeter is placed parallel to the desired boundary.
The upper limit of absolute hepatic dullness can be determined along all lines that are used to determine the lower edge of the lungs, but percussion is usually performed along the right peri-sternal, mid-clavicular, and anterior axillary lines. This produces a quiet percussion. Percussion from top to bottom, from clear to dull sound. The found border is marked with dots on the skin along the upper edge of the plessimeter finger, that is, from the side of a clear sound. Normally, the upper limit of absolute dullness of the liver is located on the peristernal and mid-clavicular lines, respectively, on the upper and lower edges of the VI rib and on the anterior axillary line on the VII rib. The upper limit of relative dullness lies on the edge above. To determine it, use percussion of medium strength.
The lower limit of absolute hepatic dullness is determined by the anterior axillary, mid-clavicular and peri-sternal lines on the right side, along the anterior midline, and on the left along the peri-sternal lines. Percussion from bottom to top from tympanic sound to dull.
Kurlov method
The boundaries of the liver can also be determined according to Kurlov. For this purpose, along the mid-clavicular line on the right, the upper border of the absolute dullness of the liver, as well as its lower edge, is determined, and the lower border is revealed along the anterior midline. The upper border on this line is conditional (it is impossible to establish it, since here the liver borders on the heart, which also gives a dull sound when percussed). To determine this border through the point, the location of which is located on the mid-clavicular line and corresponding to the level of the upper border of absolute hepatic dullness, draw a horizontal line until it intersects with the anterior midline. The intersection will be the upper border of hepatic dullness along the anterior midline.
Further, according to Kurlov, the borders of the liver are determined along the left costal arch. To do this, the pessimeter finger is installed perpendicular to the lower edge of the left costal arch, somewhat inward from the anterior axillary line. Percussion is carried out along the costal arch until a dull sound occurs and a point is set. This will be the border of the liver in the region of the left costal arch.
Palpation
It is possible to determine the size of the liver only after palpation of its lower edge, which makes it possible to clarify its localization, as well as to get an idea of \u200b\u200bits outlines, shape, consistency, pain and features of the surface of the liver itself.
When palpating the liver, certain rules and technique should be followed. The patient should be in a horizontal position on his back with his head slightly raised and legs straightened or slightly bent at the knee joints. His hands should be on his chest (in order to limit the mobility of the chest on inhalation and relax the abdominal muscles). The examiner sits down to the right of the patient, facing him, the palm of his right hand with slightly bent fingers is placed flat on his stomach, in the area of \u200b\u200bthe right hypochondrium, 3 - 5 cm below the border of the liver, found percussion, and with his left hand covers the lower section of the right half of the chest, with 4 fingers positioning it behind, and the thumb on the costal arch. This limits the mobility of the person's chest during inhalation and increases the downward movement of the diaphragm. When the patient exhales, the examiner, with a superficial movement, pulls the skin down, plunges the fingertips of his right hand into the abdominal cavity and asks the person to take a deep breath. In this case, the lower part of the liver, going down, falls into an artificial pocket, bypasses the fingers and slips out from under them. The palpating hand remains motionless all the time.
If it was not possible to palpate the lower edge of the liver, the manipulation is repeated again by moving the fingertips 1 - 2 cm up. This is done until, rising higher and higher, until the lower edge of the liver is palpated or the right hand reaches the costal arch.
Note!
The presence of symptoms such as:
- smell from the mouth
- stomach ache
- heartburn
- diarrhea
- constipation
- nausea, vomiting
- belching
- increased gas production (flatulence)
If you have at least 2 of these symptoms, then this indicates a developing
gastritis or ulcers. These diseases are dangerous for the development of serious complications (penetration, gastric bleeding, etc.), many of which can lead to
LETAL
the outcome. Treatment should be started now.
Read an article on how a woman got rid of these symptoms by defeating their root cause. Read material ...
Where is the liver located and what are its functions? This question is interesting to many people. In comparison with other organs of the human body, it is the largest and most significant. It is about 20 times heavier than the pancreas (90 grams), and the pituitary gland (in size, but not in importance) is lost against its background. What functions does this almost two-kilogram vital organ of the human body perform, and what is it? On which side is it located, why does the liver hurt? You will receive answers to these and other questions below.
In terms of physical parameters, the human liver is a soft brown-red shiny substance that has the shape of an irregular cone. Shine is given to it by a membrane called serous. 
The upper part of the organ is called diaphragmatic, since it is adjacent to the diaphragm, and it is convex, while the concave lower part stores the imprints of adjacent internal organs and is called visceral.
Which side of the liver is in the body?
If a person has one kidney removed for any reason, then the remaining one takes over its functions. Without a liver, human existence is simply impossible. But at the same time, the gland has a wonderful property - it is able to recover from only 25% of the remaining part. In ancient times, it was already known about these amazing recovery processes taking place in it.
Confirmation is the legend of Prometheus, who was punished by Zeus for the fire given to people. A bird of prey with its sharp beak regularly tormented the liver of a chained prisoner. But the iron quickly recovered, and the hero's torment continued again and again.
As you know, the gland consists of a large right lobe and is significantly inferior in size to the left. In children, the left and right lobes are equivalent, but subsequently the growth of the left lobe slows down. In percentage terms, the size of the gland in the body of newborn children is much higher than that of adults.
Which side of the human liver is located? If we briefly describe its location in the human body, it will sound like this: on the right in the hypochondrium. For the sake of objectivity, it should be noted that the liver on the left still extends 5 centimeters beyond the left edge of the sternum, and only a thin diaphragm separates it from the heart located above it. But still the main part of the liver is located on the right.
How is this heavy digestive gland held in place in the body? In a simplified form, it looks like this: from above it is attached to the diaphragm, and from below the intestines and stomach serve as a soft support for it. The gland is held by the inferior vena cava due to its fixation in the diaphragm and strong connection with the spine. Both intra-abdominal pressure and the strength of the abdominal muscles play an important role.
If we take a close look at which side the liver is from, we will understand that it is so attached to the diaphragm that it follows its every movement. In the supine position, it shifts upward, with an upright position of the body it tends downward. Despite the seemingly strong fixation of the gland, it still does not have complete immobility. If its strong connection with the diaphragm is broken due to the lengthening of the sickle and coronary ligaments, it acquires the status of hepar mobile.
If you draw up a diagram of the location of the gland in the human body, then it will occupy the area from the 5th and 6th ribs from above to the 9th and 8th costal cartilage from below, and its upper edge lies 1 cm below the right nipple, 2 cm below the left, and the lower border runs in the middle between the xiphoid process and the navel.

What the liver is made of
In a healthy state, the gland never protrudes from under the rib frame, so it is not possible to palpate it. The location of the liver in the body provides for its reliable protection by the ribs both on the right and on the left.
The main functions of the liver
The liver is a multifunctional organ. It is rightfully compared to a chemical laboratory, since it controls more than 500 chemical reactions, it is called the "second heart" of a person. The liver produces one liter of bile per day, which, thanks to the ducts, is poured into the duodenum and gallbladder. The bile production process goes on continuously.
The gallbladder is located under the liver and is a small reservoir where bile becomes highly concentrated. For this property it is customary to call it “mature”. Bile is mainly water with bile acids, cholesterol, bilirubin, pigments present in it. Thanks to bile, fats are emulsified.
The liver performs, as it were, the role of a pantry, where glucose is deposited in the form of glycogen before the onset of any unfavorable moment, when glycogen is again converted into glucose.
The liver is the most powerful filter inside the human body. Filtration occurs through the membranes of liver cells - hepatocytes, with the help of which the liver actively fights poisons and toxins. For example, it converts ammonia into urea, which is less toxic, and also has the property of being well soluble in water, which contributes to its excretion in the urine.
The liver utilizes dead red blood cells, as well as bacteria. The liver stores a supply of blood, intended in case of large blood loss, as well as vitamins A, D, B. The liver cells are able to synthesize albumin, globulin, prothrombin and heparin. The liver also contributes to the regulation of human body temperature.
So, we figured out which side of the liver, and what functions it performs in the human body. But what if the liver hurts?
Organ diseases
When a person knows where the liver is located, what is next to it, what are its properties, why the liver hurts, it is easier for him to cope with malfunctions in the body. It is well known that addiction to alcohol, nicotine and drugs inflict a severe blow on the liver. No less dangerous are the viruses that cause hepatitis A, C and B. Medicines can also adversely affect the liver.
If a person has a headache, they say they have a headache. If the liver hurts, he will never say that it is his liver that hurts. She a priori cannot experience severe pain syndrome due to the small number of nerve endings located on it.
 To facilitate the liver's hard daily work, you need to try not to overeat and not burden the stomach with a large amount of fatty foods, do not abuse alcohol and smoking, do not go to bed on a full stomach, and move more.
To facilitate the liver's hard daily work, you need to try not to overeat and not burden the stomach with a large amount of fatty foods, do not abuse alcohol and smoking, do not go to bed on a full stomach, and move more.
The symptoms of viral hepatitis are pronounced. Yellow skin and sclera of the eyes - these symptoms are difficult to confuse with anything. Jaundice occurs due to the high content of bilirubin in the blood due to the fact that it is not processed by the liver.
Sometimes liver inflammation is disguised as a flu, and then the symptoms are as follows:
- heat,
- body aches,
- severe weakness accompanied by headache.
Hepatitis is not only viral, but also alcoholic. If a person constantly drinks for many years, then alcoholic hepatitis, and later cirrhosis of the liver, is provided for him.
Liver cells die off and are replaced by adipose tissue. Therefore, the concepts of "alcoholic hepatitis" and "fatty hepatitis" are synonyms. The liver of a patient with alcoholic hepatitis becomes frightening. What are the symptoms of alcoholic hepatitis?
- urine changes its color to a darker one, and feces, on the contrary, become discolored;
- itching occurs, as in diabetes mellitus;
- all the time nauseous and bitter belching appears;
- the increased body temperature is stable.
These symptoms are aggravated by sudden weight loss and extreme weakness. People who are addicted to alcohol should be aware of the symptoms of impending danger.
The liver is an important and rather unpretentious gland in our body. It performs many functions, is able to withstand heavy loads and recover in a short period. However, the moment comes when the problems in the gland make you think about its treatment. After all, the general well-being of the body largely depends on the work of the liver, therefore, taking care of the health of the organ is the task of anyone who wants to live a long and full life.
Liver location
For primary self-diagnosis, each person needs to imagine,
where is the liver
Let's divide the belly into 4 conditional squares. In this case, the iron in the bulk will be located in the upper square on the right and will completely hide under the ribs. Its upper border will touch the lower surface of the diaphragm and will pass under the nipples. Therefore, if pain is felt behind the right side of the sternum, it is highly likely that these are liver problems.
This organ consists of two lobes, and the right one is 5 times larger in volume than the left. The liver is tightly held in place by neighboring organs, therefore, it is not difficult to determine its boundaries.
Borders
Percussion (tapping) of the three right lines helps to establish the upper and lower edges of the iron:
- periosternal - the first border will pass by the upper edge of the VI rib, the second will recede from the arch of the ribs by 2 cm downward;
- parasitic - boundary lines will be located along the lower edge of the VI rib and touch the bottom of the arch of the ribs;
- axillary anterior - pass the lower edge of the VII and X ribs.
The lower border is set, also using the median (passing along the sternum) and the left parasternal (located in the center between the left areola and the edge of the sternum) lines.
In addition to recognizing the borders of the liver, the median, right peri-sternal and left midclavicular lines make it possible to determine the height of hepatic dullness (we are talking about the size of the gland), which normally corresponds to such indicators: 9-11 cm, 8-10 cm, 7-9 cm.
Self probing
A very good skill for a person with liver problems is the ability to palpate (feel) an organ on their own.
During this process, it is important for us to determine only the lower border of the gland on the right side. It is her location that makes it possible to judge the displacement or enlargement of the liver.
For palpation, you must sit on a flat surface. With your right hand we grab the ribs on the right side so that the thumb lies in front parallel to the ribs, and the others lie on the ribs of the back - in fact, you should grab the side.
This technique will help to fix the diaphragmatic and costal movements when probing the approach of the gland to the arch of the ribs. From the side of the navel, with the fingers of the left hand, we go under the costal arch on the right (while adhering to the areola axis). At the same time, we inhale deeply - the lungs, swelling, will push the liver down and make it more noticeable.
The organ is palpated along the right areola axis. To the left of the definition, the muscles of the peritoneum interfere, to the right - it hides under the ribs.
If the liver is healthy, you will either not feel anything, or the tips of the second and third fingers will slide along the border of the right lobe. It will be thin and soft.
If normal activity is impaired, the organ is easily palpated. The border may feel hard, uneven, and bumpy. When the gallbladder is inflamed, probing is impossible.
conclusions
Normal liver sizes are those when its lower border does not extend beyond the edge of the costal arch by more than a centimeter.
Knowing the location of the liver is very important because:
- They make it possible to independently diagnose an increase and receive timely medical assistance;
- Eliminate the presence of a rare pathology - congenital rotation of internal organs, in which the liver is located on the left, and the heart - on the opposite side.
The article is provided by the VseProPechen.ru project. More information
read here
Not everyone knows exactly where the liver is located in humans. Those who studied well at school remember that it is on the right, not on the left, but this is usually where the knowledge ends. Most people begin to think about the structure and location of the liver only when they feel incomprehensible discomfort. This gland is the largest human organ, weighing about 1/20 of the weight of an adult or 1/50 of the body weight of a newborn child, performing hundreds of functions and passing through itself almost 100 liters of blood every minute. Let's correct the injustice and find out all about the liver.

Liver location
The human liver is located in the hypochondrium, on the right, directly under the diaphragm. It is conventionally divided into right and left lobes. Most of the organ is located on the right side of the hypochondrium. In part, the liver continues to the left of the midline of the sternum. The upper edge is at the level of VI of the right intercostal space, and the top of the left side is slightly raised relative to the right and reaches up to the V intercostal space. The right inferior border extends to the last intercostal space, its topography coincides with the right costal arch. From right to left, the liver stretched diagonally, to the center line of the sternum, reaching the left costal arch at the level of the V intercostal space. Thus, in shape, this organ resembles a triangle, stretched out inside the chest. In its place, the liver is held by ligaments, attaching to the diaphragm, stomach, right kidney and duodenum 12.

The anterior (lower) edge of the liver should not extend beyond the edge of the costal arch. If this happens and the location of the organ has shifted, this condition requires clarification of the reasons.
However, it is not always possible to say with certainty which side the liver is on. In rare cases, it can be located on the left. This state of the body is called organ transposition (mirroring).
Appearance and structure
This organ has a diaphragmatic (external) and visceral (internal) surfaces. On the outer surface, dents from organs are visible - the heart, inferior vena cava, thoracic spine, aorta. And the inner surface of this gland is marked by impressions of the right kidney and adrenal gland, duodenum and ascending colon.
The falciform ligament divides the organ into large and small lobes, located on the right and left, respectively. The right lobe includes the square (right) and caudate (left) lobes. It is noteworthy that the right kidney is located approximately 1.5 cm below the left, since it is displaced by the right lobe of the liver. For the same reason, the right kidney is usually slightly smaller. Because of this proximity, these organs are interconnected, and kidney failure can develop following the onset of serious liver disease.
Organ from the inside
The outermost lining of the liver is the peritoneum (serous membrane). It covers the organ on three sides. Immediately below it is a glisson capsule - a fibrous membrane. The main task of this capsule is to maintain the shape of the gland.
The liver cells are hepatocytes. A large number of metabolic processes take place in them (for example, glycogen storage). In addition, hepatocytes are involved in the formation of the hepatic tubules - these are the future hepatic ducts. Gradually increasing their diameter, the tubules form interlobular, segmental and lobar ducts. Hepatocytes are arranged in radial rows around one of the central veins.
The main structural unit of the liver is the hepatic lobule. Its functions depend on the location in the organ and the anatomical elements that make up the composition. In a healthy adult, their number can be about half a million.
When entering the connective tissue surrounding the liver lobules, the tubules turn into interlobular, then they merge, passing into larger ducts. The right and left channels of the liver consist of interlobular tubules. Sometimes there are more channels - up to five, although this is rare. They form a common hepatic duct 4–6 cm long, which flows into the cystic duct. The common bile duct formed in this way is located in the duodenum.
The transverse groove contains the hepatic gate, through which the blood and lymph vessels, as well as the nerves and the common bile duct, open.
The concept of segments and sectors of the liver
With the development of hepatology and abdominal surgery, more precise determination of the location of abnormalities in the liver was required. Therefore, in the 50s of the XX century. the doctrine of segmental anatomy of the liver was created. According to this teaching, the liver consists of the right and left lobes, which are formed from eight segments. The latter are grouped radially around the gate of the liver and constitute five sectors (zones).
A segment is a section of tissue adjacent to the liver triad, which includes the branches of the portal vein, hepatic artery and bile duct.
Blood supply
The uniqueness of the liver consists in receiving not only arterial blood from the hepatic artery, but also venous blood from the portal vein. Through this vein, blood flows through it from almost the entire body. And the main artery of the liver feeds the organ, supplying it with oxygen and other important substances. The outflow of venous blood occurs through the hepatic veins leading to the inferior vena cava. The fetus also has umbilical veins, but after birth they overgrow.
Liver innervation
There are no nerve endings in the liver itself, so we do not experience pain in case of problems with it. It is mainly innervated by the branches of the vagus nerve. Painful sensations are also possible due to stretching of the capsule, if it is stretched by an enlarged or deformed organ.
Gall bladder
Where the liver is located, there is the gallbladder, namely on its visceral surface. It is a pear-shaped hollow organ with a volume of about 50 ml. The structure of the gallbladder is the body, neck and cystic duct.
The cystic duct merging with the common hepatic duct forms a common bile duct. It opens through the sphincter of Oddi into the lumen of the duodenum. The base of the gallbladder protrudes from under the antero-inferior edge of the liver by a few centimeters, and contacts the peritoneum, and the body - with the stomach, sections of the large and small intestines.
The liver produces bile around the clock, but it enters the intestine only during the digestion of food. Therefore, in the body there is a need for a bile storage, the function of which is performed by the gallbladder.
In response to a certain reflex, the gallbladder contracts, the sphincter of Oddi relaxes, and bile ends up in the duodenum. The concentration of gallbladder bile differs from hepatic bile due to the reverse absorption of water by the gallbladder wall. Concentrated bile in the gallbladder takes on an oily green, olive tint. With stagnation of bile, stones can form, leading to pain and colic in the gallbladder.
This body. The liver is probed according to all the rules of deep sliding palpation according to Obraztsov. The doctor is located on the right side of the patient lying on his back with his arms extended along the body. A prerequisite is the maximum relaxation of the muscles of the abdominal wall of the patient during his deep breathing. It is recommended for a larger excursion of the liver to use the pressure of the palm of the doctor's left hand, located on the anterior chest wall at the bottom right. The palpating right hand lies flat on the anterior abdominal wall below the edge of the liver, determined by percussion, while the fingertips are located along the intended lower edge, sink inward synchronously with the patient's breathing and, with the next deep breath, meet with the descending edge of the liver, from under which they slide out.
When palpating the liver, first of all, its lower edge is assessed - shape, density, presence of irregularities, sensitivity. These properties can be extended to the entire mass of the liver. The edge of the normal liver on palpation is of a soft consistency, smooth, thin, painless.
The displacement of the lower edge of the liver may be associated with the prolapse of the organ without increasing it: in this case, the upper border of hepatic dullness will also be omitted. Of greater importance, naturally, is the statement of an enlarged liver (hepatomegaly), which is most often observed in congestive heart failure, in acute and chronic hepatitis, and cirrhosis of the liver. Usually, the edge of the congestive liver is more rounded and painful on palpation, the edge of the cirrhotic organ is more dense, uneven. Pressing on an enlarged congestive liver causes swelling of the right jugular vein - a simple but very important sign of detecting blood congestion in a large circle (reflux symptom, or hepatojugular reflux).
It should be noted that with large ascites, the usual percussion and palpation of the liver is difficult, therefore, the method of ballot palpation (a symptom of "floating ice") is used, with which you can get an idea of \u200b\u200bthe features of the liver edge and its surface.
The dynamics of changes in the size of the liver is very important. A rapid increase is usually observed in liver cancer, a rapid decrease in liver cirrhosis and acute fulminant hepatitis, as well as in the successful treatment of congestive heart failure.
Hepatomegaly (enlargement of the liver) is a significant sign of liver damage (hepatitis, liver cirrhosis, as well as primary cancer or cirrhosis - liver cancer). Other causes of hepatomegaly are congestive heart failure, metastases of various tumors, polycystic, lymphomas (primarily lymphogranulomatosis).
Causes of hepatomegaly
Venous congestion in the liver:
- Congestive heart failure.
- Constrictive pericarditis.
- Insufficiency of the tricuspid valve.
- Hepatic vein obstruction (Budd-Chiari syndrome).
Infection:
- Viral hepatitis (A, B, C, D,E) and liver cirrhosis (B, C, D).
- Leptospirosis.
- Liver abscess:
- amebic;
- pyogenic.
- Other infections (tuberculosis, brucellosis schistosomiasis, syphilis, echinococcosis, actinomycosis, etc.).
Hepatomegaly not associated with infection:
- Hepatitis and cirrhosis of the liver of non-viral etiology:
- alcohol;
- medications:
- toxins;
- autoimmune disorders;
- nonspecific reactive hepatitis.
- Infiltrative processes:
- fatty liver, lipoidosis (Gaucher disease);
- amyloidosis;
- hemochromatosis;
- wilson-Konovalov disease;
- a1-antitrypsin deficiency;
- glycogenosis;
- granulomatosis (sarcoidosis).
Bile duct obstruction:
- Stones.
- Common bile duct strictures.
- Tumors of the pancreas, ampulla of Vater's nipple, bile duct pancreatitis.
- Compression of ducts by enlarged lymph nodes.
- Sclerosing cholangitis (primary, secondary).
- Hepatocellular carcinoma, cholangiocarcinoma.
- Tumor metastases to the liver.
- Leukemia, lymphoma.
Cysts (polycystic).
In addition to these reasons, an increase in the liver is observed with fatty degeneration (more often alcoholic or diabetic genesis), amyloidosis (especially secondary), liver alveococcosis, with large cysts and abscess located close to the anterior surface of the organ.
Since an enlargement of the spleen (splenomegaly) is often observed simultaneously with hepatomegaly, it is advisable to use the term "hepatolienal syndrome".
, , , , , ,
Causes of hepatolienal syndrome
|
Diseases |
|
|
Cirrhosis of the liver. |
Viral infection; autoimmune disorders; primary sclerosing cholangitis, impaired metabolism of copper, iron; less often - alcoholic, primary biliary cirrhosis. |
|
Granulomatosis. |
Sarcoidosis; beryllium disease; histoplasmosis; schistosomiasis. |
|
Hemoblastosis: |
|
|
myeloproliferative diseases. |
Polycythemia vera (erythremia); myelofibrosis; chronic myeloid leukemia; |
|
lymphoproliferative diseases. |
Chronic lymphocytic leukemia; lymphoma; lymphogranulomatosis; |
|
Amyloidosis. |
waldenstrom's macroglobulinemia. |
|
Gaucher disease. |
|
The gallbladder becomes available for palpation with a significant increase: with empyema (purulent inflammation), dropsy, chronic cholecystitis, cancer. In these cases, it can be felt in the form of a saccular body of dense or elastic consistency in the area between the lower edge of the liver and the edge of the right rectus abdominis muscle. A symptom of Courvoisier is distinguished - a distended bile bladder with normal elastic walls (when the common bile duct is blocked by a tumor in the head of the pancreas). Very rarely, it is possible with the help of palpation to get a feeling of vibration, which is transmitted to the adjacent spaced fingers of the left hand when one of them is tapped.
The liver is an important element in the human body, which is the first to take the hit of toxic substances and bad habits. But many do not even know where the liver is located in a person, from which side the liver hurts, and even more so they do not even suspect how to look after it.
Chronic diseases often take a latent course, nothing hurts a person, and when probing the liver, and the results of laboratory tests, significant changes are found.
Liver location
Most people do not know which side of the liver to look for in the human body - to the right or to the left, so we will analyze this issue in more detail.
If the abdomen is conventionally divided into 4 squares, then its bulk is located in the upper square on the right side and is completely hidden under the ribs, with an increase it will occupy the right side of the upper, possibly the middle third of the abdomen. The upper border is located under the nipples of a person, i.e. it touches the bottom surface of the diaphragm. Therefore, if it hurts behind the sternum on the right side, then most likely it hurts the liver.
Location of human organs
In the organ, two lobes are distinguished - right and left, the right one is 5 times larger. The left one is small, so it is not probed, only percussed to determine the true hepatic size.
The liver is easily held in place, as it is very tightly in contact with neighboring internal organs, which leave depressions on it, from below it is the duodenum, left kidney and left adrenal gland, the transverse part of the large intestine and the heart touches its top from above.

Liver structure
To make it easier to remember which side the liver is on, remember that it is on the opposite side of the heart.
Borders
The location of the upper border is determined by three lines and only on the right:
- On the right side of the sternum - the edge of the VI rib from above.
- Along the right parasitic - the edge of the VI rib from below.
- On the anterior axillary - the edge of the VII rib from below.
The location of the lower border is determined along the same lines and additionally along the median (chest line, which is the axis of the sternum passage) and the left parasternal (which is equally distant from the edge of the sternum and the left parasolateral line):

In addition to defining the boundaries along the left midclavicular, median and right peri-sternal lines, the height of hepatic dullness (liver size) is determined, which normally corresponds to the following figures: 9-11 cm, 8-10 cm and 7-9 cm.
Can you feel it yourself
It is very good if a person who suspects he has liver disease can palpate (feel) it on his own.
When probing, we are only interested in the lower edge of the liver on the right side, since it is he who, when shifting, shows a real displacement or enlargement of the organ.
To do this, you need to lie on a flat surface, with your right hand grab yourself by the right side of the ribs so that the thumb lies in front parallel to the course of the ribs, and the other four on the ribs from the back, as if you are holding your side.
This is necessary to fix the movement of the ribs and diaphragm during palpation, the approach of the liver to the costal arch. We start four fingers of the left hand from the side of the navel under the right costal arch, adhering to the areola axis, while taking a deep breath, while inhaling, the lungs inflate and push the liver downward, which makes it more noticeable.
 You can feel it along the right areola line, to the right it is hidden under the ribs, to the left of it it is difficult to determine the abdominal muscles.
You can feel it along the right areola line, to the right it is hidden under the ribs, to the left of it it is difficult to determine the abdominal muscles.
Normally, you will either not feel anything, or slide the tips of your second and third fingers along the thin and soft edge of the right lobe of the liver.
In case of diseases, it will be increased and it can be easily palpated. Its edge can be hard or soft, possibly irregular and bumpy. The inflamed gallbladder hurts a lot, and then palpation is impossible.