Breaks down another protein in the blood angiotensinogen (ATG) with the formation of protein angiotensin 1 (AT1), consisting of 10 amino acids (decapeptide).
Another blood enzyme APF(Angiotensin converting enzyme, Angiotensin converting enzyme (ACE), Lung converting factor E) cleaves the two tail amino acids from AT1 to form an 8 amino acid protein (octapeptide) called angiotensin 2 (AT2). Other enzymes, chymases, cathepsin G, tonin and other serine proteases, also have the ability to form angiotensin 2 from AT1, but to a lesser extent. The pineal gland of the brain contains a large number of chymase, which converts AT1 to AT2. Angiotensin 2 is mainly formed from angiotensin 1 under the influence of ACE. The formation of AT2 from AT1 by chymases, cathepsin G, tonin and other serine proteases is called the alternative pathway for AT2 formation. ACE is present in the blood and in all tissues of the body, but ACE is most synthesized in the lungs. ACE is a kininase, so it breaks down kinins, which have a vasodilating effect in the body.
Potassium replacement and potassium-sparing diuretics
Sections “Contraindications” and “Warnings and Precautions”. Based on experience with other drugs that modify the renin-angiotensin system, increases in serum potassium are predictable when coadministration of a potassium-sparing diuretic, potassium supplements, potassium-containing foods, electrolytes, or other medicines, which may increase serum potassium levels and are therefore not recommended.
Effects of olmesartan medoxomil on other substances
At the beginning of treatment, regular monitoring of renal function and proper hydration of the patient is recommended. Concomitant administration of warfarin and digoxin did not affect the pharmacokinetics of olmesartan. About the risk of lithium toxicity. Specific clinical studies were conducted in healthy volunteers with warfarin, digoxin, antacid, hydrochlorothiazide and pravastatin. No clinically significant interactions were observed.
Angiotensin 2 exerts its effect on the body's cells through proteins on the surface of cells called angiotensin receptors (AT receptors). AT receptors are different types: AT1 receptors, AT2 receptors, AT3 receptors, AT4 receptors and others. AT2 has the greatest affinity for AT1 receptors. Therefore, first of all, AT2 interacts with AT1 receptors. As a result of this connection, processes occur that lead to an increase in blood pressure (BP). If the level of AT2 is high, and there are no free AT1 receptors (not associated with AT2), then AT2 binds to AT2 receptors, for which it has less affinity. The connection of AT2 with AT2 receptors triggers opposite processes that lead to a decrease in blood pressure.
Effect on the ability to drive and use machines
It is preferable to use other treatments with a well-established safety profile during breastfeeding, especially in newborns or premature infants. Patients taking antihypertensive medications may sometimes experience dizziness and fatigue, which may reduce their ability to respond. In placebo-controlled monotherapy studies, dizziness was the only adverse event that was clearly related to treatment.
Angiotensin 2 (AT2) connecting to AT1 receptors:
- has a very strong and prolonged vasoconstrictor effect on the vessels (up to several hours), thereby increasing vascular resistance, and, therefore, arterial pressure(HELL). As a result of the connection of AT2 with AT1 cell receptors blood vessels, chemical processes are launched, as a result of which the smooth muscle cells of the tunica media contract, the vessels narrow (vasospasm occurs), the internal diameter of the vessel (the lumen of the vessel) decreases, and the resistance of the vessel increases. At a dose of only 0.001 mg, AT2 can increase blood pressure by more than 50 mmHg.
- initiates the retention of sodium and water in the body, which increases the volume of circulating blood, and, therefore, blood pressure. Angiotensin 2 acts on cells of the zona glomerulosa of the adrenal gland. As a result of this action, the cells of the zona glomerulosa of the adrenal glands begin to synthesize and release the hormone aldosterone (mineralocorticoid) into the blood. AT2 promotes the formation of aldosterone from corticosterone through its action on aldosterone synthetase. Aldosterone enhances the reabsorption (absorption) of sodium, and therefore water, from the renal tubules into the blood. This results:
- to water retention in the body, and, therefore, to an increase in the volume of circulating blood and to the resulting increase in blood pressure;
- Sodium retention in the body causes sodium to leak into the endothelial cells that line the inside of blood vessels. An increase in sodium concentration in a cell leads to an increase in the amount of water in the cell. Endothelial cells increase in volume (swell, “swell”). This leads to a narrowing of the lumen of the vessel. Reducing the lumen of the vessel increases its resistance. An increase in vascular resistance increases the strength of heart contractions. In addition, sodium retention increases the sensitivity of AT1 receptors to AT2. This accelerates and enhances the vasoconstrictor effect of AT2. All this leads to an increase in blood pressure
- stimulates the cells of the hypothalamus to synthesize and release into the blood the antidiuretic hormone vasopressin and the cells of the adenohypophysis (anterior pituitary gland) of adrenocorticotropic hormone (ACTH). Vasopressin has:
- vasoconstrictor effect;
- retains water in the body, increasing the reabsorption (absorption) of water from the renal tubules into the blood as a result of the expansion of intercellular pores. This leads to an increase in the volume of circulating blood;
- enhances the vasoconstrictor effect of catecholamines (adrenaline, norepinephrine) and angiotensin 2.
- is a kininase, therefore it breaks down kinins, which have a vasodilating effect in the body.
With an increase in the level of angiotensin 2 in the blood, a feeling of thirst and dry mouth may appear.
Additional information for elderly patients: In elderly patients, the incidence of hypotension increased to "infrequent". Information about overdose in humans is limited. The most likely effect of overdose is hypotension. In case of overdose, the patient will be closely monitored and symptomatic and supportive treatment will be provided.
There is no data on the elimination of olmesartan medoxomil by dialysis. It plays an important role in the pathophysiology of hypertension by acting on type 1 receptors. There is no evidence of hypotension after the first administration or tachyphylaxis with prolonged administration or hypertension after cessation of therapy. With an equivalent total daily dose, administration in 1 or 2 doses leads to a similar reduction in blood pressure. With continuous treatment, the maximum reduction in blood pressure is achieved 8 weeks after the start of treatment, with a significant reduction in blood pressure observed after 2 weeks of treatment.
With a prolonged increase in AT2 blood and tissues:
- smooth muscle cells of blood vessels are in a state of contraction (compression) for a long time. As a result, hypertrophy (thickening) of smooth muscle cells and excessive formation of collagen fibers develop - the walls of the vessels thicken, the internal diameter of the vessels decreases. Thus, hypertrophy of the muscular layer of blood vessels, which developed under the prolonged influence of an excessive amount of AT2 in the blood on the vessels, increases the peripheral vascular resistance, and, therefore, blood pressure;
- the heart is forced to contract with greater force for a long time in order to pump a larger volume of blood and overcome greater resistance from spasmodic vessels. This leads first to the development of hypertrophy of the heart muscle, to an increase in its size, to an increase in the size of the heart (larger than the left ventricle), and then there is depletion of heart muscle cells (myocardiocytes), their dystrophy (myocardial dystrophy), ending with their death and replacement connective tissue(cardiosclerosis), which ultimately leads to heart failure;
- prolonged spasm of blood vessels in combination with hypertrophy of the muscular layer of blood vessels leads to a deterioration in the blood supply to organs and tissues. Insufficient blood supply primarily affects the kidneys, brain, vision, and heart. Insufficient blood supply to the kidneys over a long period of time leads kidney cells to a state of dystrophy (exhaustion), death and replacement with connective tissue (nephrosclerosis, kidney shrinkage), deterioration of kidney function ( renal failure). Insufficient blood supply to the brain leads to deterioration of intellectual capabilities, memory, communication skills, performance, and emotional disorders, sleep disorders, headaches, dizziness, tinnitus, sensory disorders and other disorders. Insufficient blood supply to the heart leads to coronary heart disease (angina pectoris, myocardial infarction). Insufficient blood supply to the retina of the eye leads to progressive impairment of visual acuity;
- the sensitivity of body cells to insulin decreases (cell insulin resistance) – initiation and progression diabetes mellitus 2 types. Insulin resistance leads to an increase in insulin in the blood (hyperinsulinemia). Prolonged hyperinsulinemia causes a persistent increase in blood pressure - arterial hypertension, since it leads to:
- to the retention of sodium and water in the body - an increase in the volume of circulating blood, an increase in vascular resistance, an increase in the force of heart contractions - an increase in blood pressure;
- to hypertrophy of vascular smooth muscle cells - - increased blood pressure;
- to an increased content of calcium ions inside the cell - - increased blood pressure;
- to an increase in tone - an increase in the volume of circulating blood, an increase in the strength of heart contractions - an increase in blood pressure;
Angiotensin 2 undergoes further enzymatic cleavage by glutamyl aminopeptidase to form Angiotensin 3, consisting of 7 amino acids. Angiotensin 3 has a weaker vasoconstrictor effect than angiotensin 2, but its ability to stimulate aldosterone synthesis is stronger. Angiotensin 3 is broken down by the enzyme arginine aminopeptidase to angiotensin 4, consisting of 6 amino acids.
When combined with hydrochlorothiazide for an additive blood pressure lowering effect, this concomitant administration is well tolerated. After adjusting for differences in blood pressure, this risk reduction was no longer statistically significant, with 2% of patients in the olmesartan group and 8% in the placebo group developing microalbuminuria. For secondary endpoints, cardiovascular events occurred in 96 patients with olmesartan and in 94 patients with placebo.
The composite secondary cardiovascular endpoint was assessed in 40 patients receiving olmesartan and 53 patients receiving placebo. This study was stopped prematurely due to increased risk adverse events. The mean peak plasma concentration of olmesartan is achieved within 2 hours after oral administration of olmesartan medoxomil. After oral administration of a single dose, the plasma concentration of olmesartan increases in a dose-dependent manner to 80 mg.
Angiotensin II receptor blockers are one of the new classes of drugs for normalizing blood pressure. The names of drugs in this group end in “-artan”. Their first representatives synthesized in the early 90s of the twentieth century. Angiotensin II receptor blockers inhibit the activity of the renin-angiotensin-aldosterone system, thereby promoting a number of beneficial effects. Not inferior in effectiveness to other classes of drugs for the treatment of hypertension, they have a minimum side effects, actually protect the heart, kidneys and brain from damage and improve the prognosis of patients with hypertension.
After intravenous administration the average volume of distribution is low. Based on a systemic availability of 6%, it can be estimated that absorbed olmesartan is eliminated by both the renal and hepato-biliary routes. No other metabolites were detected. Since most olmesartan is eliminated bile duct, its use is contraindicated in patients with obstruction biliary tract. After repeated oral administration, the half-life of olimesartan varies from 10 to 15 hours. A state of equilibrium is achieved from the first doses and no accumulation is observed after 14 days of repeated doses.

We list synonyms for these drugs:
- angiotensin II receptor blockers;
- angiotensin receptor antagonists;
- sartans.
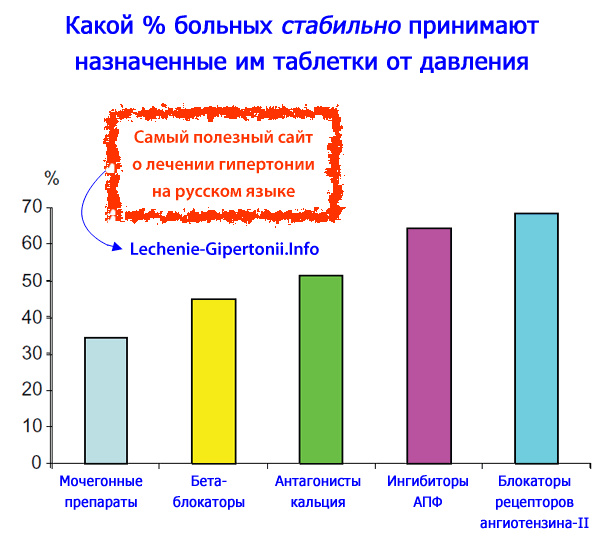
Angiotensin II receptor blockers have the best adherence to treatment among all classes of blood pressure pills. It has been established that the proportion of patients who stably continue to take medications for hypertension for 2 years is the highest among those patients who are prescribed sartans. The reason is that these drugs have the lowest incidence of side effects, comparable to the use of placebo. The main thing is that patients practically do not experience a dry cough, which is a common problem when prescribing ACE inhibitors.
Kinetics in selected patient groups
This may be partly due to a general decline in renal function in this group of patients.
Impaired liver function
Two hours after administration, the free fraction of olmesartan was 26% in healthy volunteers, 34% in patients with mild hepatic impairment, and 41% in those with moderate hepatic impairment.The medicinal product should not be used beyond the date indicated after the words “Use By” on the package. Film-coated tablets with valsartan 40 mg. Film-coated tablets with valsartan 80 mg. Round, pink, biconvex film tablets with groove fragmentation on both sides.
Treatment of hypertension with angiotensin II receptor blockers
Sartans were originally developed as medications for hypertension. Numerous studies have shown that they lower blood pressure about as powerfully as other major classes of hypertension pills. Angiotensin II receptor blockers, when taken once a day, uniformly lower blood pressure over 24 hours. This is confirmed by daily monitoring data, which was carried out as part of clinical studies. Since it is enough to take the tablets once a day, this dramatically increases patient compliance with hypertension treatment.
Film-coated tablets with valsartan 160 mg. Oval, yellow, bicuspid film tablet with a fragmentation groove on one side. Mild treatment and moderate hypertension in adults. Long-term prophylactic treatment in adult patients stabilized after myocardial infarction with respect to left ventricular dysfunction and ejection fraction ≤40%.
Usual dosage recommendations. Significant arterial hypertension. The antihypertensive effect is noticeable within 2 weeks, maximum 4 weeks after the start of treatment, and if the reduction in blood pressure is not sufficient, daily dose may be increased to 160 mg Or a diuretic may be added.
Read about the treatment of diseases associated with hypertension:
The effectiveness of lowering blood pressure with drugs from this group depends on the initial activity of the renin-angiotensin system. They act most strongly on patients with high renin activity in the blood plasma. You can check it by taking a blood test. All angiotensin II receptor blockers have a long-term effect of lowering blood pressure, which lasts for 24 hours. This effect appears after 2-4 weeks of therapy and intensifies by the 6-8th week of treatment. Most drugs cause a dose-dependent decrease in blood pressure. It is important that they do not disrupt his normal daily rhythm.
The recommended starting dose is 2 x 40 mg valsartan per day as a film-coated tablet. Depending on tolerance, the dose will be increased in increments to 80 mg valsartan 2 times a day, and then 160 mg valsartan 2 times a day in the form of a film-coated tablet. When administering a diuretic simultaneously, consider reducing the dose of the diuretic. Maximum dose valsartan in clinical studies was 320 mg per day.
Continuous monitoring of renal function is necessary when monitoring patients with heart failure. Condition after acute myocardial infarction. After an initial dose of 20 mg twice daily, the dose will be increased in stages, usually over several weeks, to 40 mg twice daily and then to 80 mg twice daily or 160 mg twice daily as a film-coated tablet .
Available clinical observations indicate that with long-term use of angiotensin receptor blockers (for two years or more), addiction to their action does not occur. Canceling treatment does not lead to a rebound increase in blood pressure. Angiotensin II receptor blockers do not reduce blood pressure levels if they are within normal values. When compared with tablets of other classes, it was noted that sartans, while providing a similar powerful effect in lowering blood pressure, cause less side effects and are better tolerated by patients.
The starting dose is possible with 40 mg film-coated tablets. The maximum target dose is 160 mg twice daily. While individual tolerance is allowed during dose titration, it is generally recommended that patients receive a dose of 80 mg twice daily after 2 weeks of treatment and the maximum target dose after 3 months.
Dosage reduction will be considered for symptomatic hypotension or renal failure. Monitoring of patients after acute myocardial infarction should always include monitoring of renal function. Liver and kidney failure. There is no experience with the use of valsartan in children and adolescents.
Angiotensin receptor antagonists not only lower blood pressure, but also improve renal function in diabetic nephropathy, cause regression of left ventricular hypertrophy, and improve heart failure. IN last years There has been a debate in the literature regarding the ability of these tablets to increase the risk of fatal myocardial infarction. Several studies suggest negative impact sartans on the incidence of myocardial infarction were not carried out correctly enough. It is currently believed that the ability of angiotensin II receptor blockers to increase the risk of fatal myocardial infarction is not proven.
It should be taken with water. Pregnancy and breast-feeding. For hypotension, place the patient in the supine position and add saline intravenously. Treatment can be resumed as soon as blood pressure returns to normal.
Administration of Valsartan Axapharm to 12 short-term patients with renovascular hypertension due to unilateral renal artery stenosis did not show any significant hemodynamic changes in the kidneys and no significant changes in serum creatinine or blood urea nitrogen. Therefore, as a precautionary measure, careful monitoring of these two parameters is recommended in such cases. No dose adjustment is required for mild to moderate renal impairment.
If patients are prescribed only one medicine from the sartan group, the effectiveness will be 56-70%, and if combined with other drugs, most often with diuretics dichlorothiazide (hydrochlothiazide, hypothiazide) or indapamide, then the effectiveness increases to 80-85%. We point out that thiazide diuretics not only enhance, but also prolong the effect of angiotensin-II receptor blockers in lowering blood pressure. Fixed combination drugs of sartans and thiazide diuretics are listed in the table below. They are widely available in pharmacies and are convenient for doctors and patients.
In patients who had myocardial infarction, a doubling of serum creatinine was observed in 2% of patients receiving valsartan, 8% of patients with a combination of valsartan and captopril, and in 4% of patients receiving captopril. Valsartan is practically excluded as unchanged bile. Elimination of valsartan is lower in patients with biliary obstruction. Valsartan should be administered with extreme caution in patients with biliary obstruction.
Administration of valsartanen Axapharm may generally lead to a decrease in blood pressure in patients with heart failure or after acute myocardial infarction. Interruption of valsartan Axapharm following persistent symptomatic hypotension is usually not necessary, provided this caution is recommended in patients with heart failure or acute myocardial infarction, especially at the beginning of treatment.
Angiotensin receptor antagonists, which are registered and used in Russia(April 2010)
| A drug | Tradename | Manufacturer | Tablet dosage, mg |
|---|---|---|---|
| Losartan | Kozaar | Merck | 50, 100 |
| Losartan + hypothiazide | Gizaar | 50 + 12,5 | |
| Losartan + hypothiazide | Gizaar forte | 100 + 12,5 | |
| Losartan | Lorista | KRKA | 12,5, 25, 50, 100 |
| Losartan + hypothiazide | Lorista N | 50 + 12,5 | |
| Losartan + hypothiazide | Lorista ND | 100 + 12,5 | |
| Losartan | Lozap | Zentiva | 12,5, 50 |
| Losartan + hypothiazide | Lozap plus | 50 + 12,5 | |
| Losartan | Presartan | IPCA | 25, 50 |
| Losartan | Vasotens | Actavis | 50, 100 |
| Valsartan | Diovan | Novartis | 40, 80, 160, 320 |
| Valsartan + hypothiazide | Co Diovan | 80 + 12,5, 160 + 12,5, | |
| Amlodipine + valsartan | Exforge | 5(10) + 80(160) | |
| Amlodipine + valsartan + hydrochlorothiazide | Co-Exforge | 5 + 160 + 12,5, 10 + 160 + 12,5 | |
| Valsartan | Valsacor | KRKA | 40, 80, 160 |
| Candesartan | Atakand | AstraZeneca | 8, 16, 32 |
| Candesartan + hypothiazide | Atacand plus | 16 + 12,5 | |
| Eprosartan | Teveten | Solvay Pharmaceuticals | 400, 600 |
| Eprosartan + hypothiazide | Teveten plus | 600 + 12,5 | |
| Irbersartan | Aprovel | Sanofi | 150, 300 |
| Irbesartan + hypothiazide | Coaprovel | 150 + 12,5, 300 + 12,5 | |
| Telmisartan | Mikardis | Boehringer Ingelheim | 40, 80 |
| Telmisarnate + hypothiazide | Mikardis plus | 40 + 12,5, 80 + 12,5 |
Sartans differ in their chemical structure and their effect on the patient’s body. Depending on the presence of the active metabolite, they are divided into prodrugs (losartan, candesartan) and active substances(valsartan, irbesartan, telmisartan, eprosartan).
Following inhibition of the renin-angiotensin-aldosterone system, changes in renal function are expected in patients predisposed. Monitoring of patients with heart failure or acute myocardial infarction should always include monitoring of renal function.
This association clearly increases the risk of adverse events and is therefore not recommended. Such combinations should only be used under specialist supervision and with careful monitoring of renal function, electrolytes and blood pressure. The effectiveness and safety of valsartan-olan-lefenant have not been studied.
| Food influence | Excretion from the body by kidneys/liver, % | Dosage, mg per tablet | Starting dose, mg | Maintenance dose, mg | |
|---|---|---|---|---|---|
| Valsartan | 40-50% | 30/70 | 80-160 | 80 | 80-160 |
| Irbesartan | No | 25/75 | 75, 150, 300 | 75-150 | 150-300 |
| Candesartan | No | 60/40 | 4, 8, 16, 32 | 16 | 8-16 |
| Losartan | minimally | 35/65 | 25, 50, 100 | 25-50 | 50-100 |
| Telmisartan | No | 1/99 | 40, 80 | 40 | 40-80 |
| Eprosartan | No | 30/70 | 200, 300, 400 | 60 | 600-800 |
- heart failure;
- previous myocardial infarction;
- diabetic nephropathy;
- proteinuria/microalbuminuria;
- hypertrophy of the left ventricle of the heart;
- atrial fibrillation;
- metabolic syndrome;
- intolerance to ACE inhibitors.
The difference between sartans and ACE inhibitors is also that their use in the blood does not increase the level of proteins associated with inflammatory reactions. This allows you to avoid such unwanted adverse reactions, such as cough and angioedema.
Double blockade of the renin-angiotensin-aldosterone system. There is no data on the effect of valsartan on human fertility. Studies in rats have shown no effect of valsartan on fertility. Careful monitoring of serum lithium is recommended when the risk of toxicity is associated. Lithium may be further increased when diuretics and valsartan Axapharm are administered concomitantly. Potassium: "Concomitant administration of potassium-sparing diuretics, potassium supplements, salt substitutes containing potassium, or other drugs that may increase potassium levels may result in an increase in serum potassium, and an increase in serum creatinine in patients with heart failure.
In the 2000s, serious studies were completed that confirmed the presence of angiotensin receptor antagonists powerful action to protect internal organs from damage due to hypertension. Accordingly, patients have an improved cardiovascular prognosis. In patients who are at high risk of heart attack and stroke, the likelihood of a cardiovascular accident is reduced. With diabetic neuropathy, the development of the last stage of renal failure is inhibited, the transition from microalbuminuria to pronounced proteinuria is slowed down, i.e., protein excretion in daily urine is reduced.
Caution should be exercised during coadministration. Therefore, caution is advised in such patients and renal function should be regularly monitored during association with these drugs. No clinically significant interactions were observed with cimetidine, warfarin, furosemide, digoxin, atenolol, indomethacin, hydrochlorothiazide, amlodipine and glibenclamide.
For medicines, acting directly on the renin-angiotensin-aldosterone system, fetal injury and death have been described following administration during the second and third trimesters of pregnancy. Cases of spontaneous abortion, oligoamnios, and neonatal renal function have been reported when pregnant women inadvertently took valsartan. All neonates exposed in utero should be carefully screened for adequate urinary excretion, hyperkalemia, and normal blood pressure.
From 2001 to 2008, the indications for the use of angiotensin II receptor blockers were constantly expanded in European countries. clinical guidelines for the treatment of arterial hypertension. Dry cough and intolerance to ACE inhibitors are no longer the only indication for their use. The LIFE, SCOPE and VALUE studies confirmed the advisability of prescribing sartans for cardiovascular diseases, and the IDNT and RENAAL studies - for problems with kidney function.
How do angiotensin II receptor blockers protect? internal organs patients with hypertension:
- Reduce hypertrophy of the mass of the left ventricle of the heart.
- Improves diastolic function.
- Reduce ventricular arrhythmias.
- Reduces protein excretion in urine (microalbuminuria).
- They increase renal blood flow without significantly reducing the glomerular filtration rate.
- They do not provide negative influence on the exchange of purines, cholesterol and blood sugar.
- Increases tissue sensitivity to insulin, i.e. reduces insulin resistance.
To date, much evidence has accumulated regarding the good effectiveness of sartans in hypertension, including dozens of large-scale studies examining their benefits compared to other blood pressure medications, in particular ACE inhibitors. Long-term studies have been conducted in which patients with various cardiovascular diseases participated. Thanks to this, we were able to expand and clarify the indications for the use of angiotensin-II receptor antagonists.
Combination of sartans with diuretics
Angiotensin II receptor blockers are often prescribed along with diuretics, especially dichlorothiazide (hydrochlorothiazide). It is officially recognized that this combination is good for lowering blood pressure, and it is advisable to use it. Sartans in combination with diuretics act evenly and for a long time. The target blood pressure level can be achieved in 80-90% of patients.
Examples of tablets containing fixed combinations of sartans with diuretics:
- Atacand plus - candesartan 16 mg + hydrochlorothiazide 12.5 mg;
- Co-diovan - valsartan 80 mg + hydrochlorothiazide 12.5 mg;
- Lorista N/ND - losartan 50/100 mg + hydrochlorothiazide 12.5 mg;
- Micardis plus - telmisartan 80 mg + hydrochlorothiazide 12.5 mg;
- Teveten plus - eprosartan 600 mg + hydrochlorothiazide 12.5 mg.
Practice shows that all these drugs effectively lower blood pressure and also protect the internal organs of patients, reducing the likelihood of heart attack, stroke and kidney failure. Moreover, side effects develop very rarely. However, it must be borne in mind that the effect of taking the tablets increases slowly, gradually. The effectiveness of a particular drug for a particular patient should be assessed no earlier than after 4 weeks of continuous use. If the doctor and/or the patient himself does not know this, then they may make the wrong decision too early that the pills need to be replaced with others because they are weak.
In 2000, the results of the CARLOS study (Candesartan/HCTZ versus Losartan/HCTZ) were published. It involved 160 patients with stage 2-3 hypertension. 81 of them took candesartant + dichlothiazide, 79 - losartan + dichlothiazide. As a result, they found that the combination with candesartan lowers blood pressure more strongly and lasts longer. In general, it should be noted that very few studies have been conducted that directly compare combinations of various angiotensin II receptor blockers with diuretics.
How angiotensin II receptor blockers act on the heart muscle
The decrease in blood pressure with the use of angiotensin II receptor blockers is not accompanied by an increase in heart rate. Of particular importance is the blockade of the activity of the renin-angiotensin-aldosterone system directly in the myocardium and vascular wall, which contributes to the regression of hypertrophy of the heart and blood vessels. The effect of angiotensin II receptor blockers on the processes of myocardial hypertrophy and remodeling is of therapeutic importance in the treatment of ischemic and hypertensive cardiomyopathy, as well as cardiosclerosis in patients with coronary disease hearts. Angiotensin II receptor blockers also neutralize the participation of angiotensin II in the processes of atherogenesis, reducing atherosclerotic damage to heart vessels.
Indications for the use of angiotensin II receptor blockers(year 2009)
| Index | Losartan | Valsartan | Candesartan | Irbesartan | Olmesartan | Eprosartan | Telmisartan |
|---|---|---|---|---|---|---|---|
| Arterial hypertension | + | + | + | + | + | + | + |
| Patients with hypertension and left ventricular myocardial hypertrophy | + | ||||||
| Nephropathy (kidney damage) in patients with type 2 diabetes | + | + | |||||
| Chronic heart failure | + | + | + | ||||
| Patients who have had myocardial infarction | + |
How do these pills affect the kidneys?
The kidney is a target organ for hypertension, the function of which is significantly affected by angiotensin II receptor blockers. They usually reduce protein excretion in the urine (proteinuria) in patients with hypertensive and diabetic nephropathy (kidney damage). However, it must be remembered that in patients with unilateral renal artery stenosis, these drugs can cause an increase in plasma creatinine levels and acute renal failure.
Angiotensin II receptor blockers have a moderate natriuretic effect (cause the body to eliminate salt in the urine) by inhibiting the reabsorption of sodium in the proximal tubule, as well as by inhibiting the synthesis and release of aldosterone. A decrease in the reabsorption of sodium into the blood in the distal tubule due to aldosterone contributes to some diuretic effect.
Medicines for hypertension from another group - ACE inhibitors - have a proven property of protecting the kidneys and inhibiting the development of renal failure in patients. However, as application experience accumulated, the problems associated with their purpose became apparent. 5-25% of patients develop a dry cough, which may be so painful that it requires discontinuation of the medication. Occasionally, angioedema occurs.
Also, nephrologists attach special importance to specific kidney complications, which sometimes develop while taking ACE inhibitors. This sharp drop glomerular filtration rate, which is accompanied by an increase in the level of creatinine and potassium in the blood. The risk of such complications is increased for patients diagnosed with atherosclerosis of the renal arteries, congestive heart failure, hypotension and a decrease in circulating blood volume (hypovolemia). This is where angiotensin II receptor blockers come to the rescue. Compared to ACE inhibitors, they do not reduce the glomerular filtration rate of the kidneys as sharply. Accordingly, the level of creatinine in the blood increases less. Sartans also inhibit the development of nephrosclerosis.
Side effects
A distinctive feature of angiotensin II receptor blockers is their good tolerability, comparable to placebo. Side effects when taking them are observed much less frequently than when using ACE inhibitors. Unlike the latter, the use of angiotensin II blockers is not accompanied by the appearance of a dry cough. It also develops much less frequently angioedema.
Like ACE inhibitors, these drugs can cause a fairly rapid decrease in blood pressure in hypertension, which is caused by increased renin activity in the blood plasma. In patients with bilateral narrowing of the renal arteries, renal function may deteriorate. The use of angiotensin II receptor blockers in pregnant women is contraindicated due to high risk developmental disorders of the fetus and its death.
Despite all these undesirable effects, sartans are considered the most well tolerated group of drugs for lowering blood pressure by patients, with the lowest incidence of adverse reactions. They combine well with almost all groups of drugs that normalize blood pressure, especially with diuretics.
Why choose angiotensin II receptor blockers?
As you know, there are 5 main classes of drugs for the treatment of hypertension, which reduce blood pressure approximately equally. Read the article “” for more details. Since the potency of the drugs differs slightly, the doctor chooses the drug depending on how it affects metabolism and how well it reduces the risk of heart attack, stroke, kidney failure and other complications of hypertension.
Angiotensin II receptor blockers have a uniquely low incidence of side effects, comparable to placebo. Their “relatives” - ACE inhibitors - are characterized by undesirable effects such as dry cough, and even angioedema. When prescribing sartans, the risk of these problems is minimal. Let us also mention that the ability to reduce concentration uric acid in the blood distinguishes losartan from other sartans.
Didn't find the information you were looking for?
Ask your question here.
How to cure hypertension on your own
in 3 weeks, without expensive harmful drugs,
"starvation" diet and heavy physical training:
free step-by-step instructions.
or, conversely, criticize the quality of site materials