olga Lukinskaya
Little is said about kidney health, and their diseases may not manifest themselves at all until a certain stage. Nevertheless, if insufficiency develops, that is, the organs do not cope with their task, the person finds himself in a very dangerous situation: the body does not have time to cleanse itself and intoxication can quickly lead to death.
People with severe renal failure have two treatment options: kidney transplantation and dialysis, that is, the purification of the blood with a special apparatus. Transplant opportunities are limited by the lack of donor kidneys - which is why people live on dialysis for years. We talked with L. about what life is like on dialysis and why you shouldn't give up even in the most dramatic situations.
my story with kidney problems began in early childhood, in circumstances that no one remembers for sure. It seems that I had some kind of complicated poisoning, pulmonary edema, resuscitation and two days in a coma. They saved my life, but I became a patient of nephrologists forever.
My diagnosis then was quite abstract - nephritis, that is, inflammation of the kidney. As a child, I poorly understood why my mother "tortures" me with diets, frequent tests, why I have a group of exercise therapy in physical education. Mom always told me about my peculiarities, about what happened in childhood, but I did not attach any importance to this, since I did not see any real manifestations of the disease. Childhood and adolescence were carefree, like everyone else. By the age of eighteen, during regular routine blood tests, an increased level of creatinine was found, and this alerted the doctors. I underwent a full examination at the Clinic of Nephrology, Internal and Occupational Diseases named after E.M. Tareev was with Professor Shilov, and after a couple of weeks I was diagnosed with chronic tubulointerstitial nephritis. The kidneys have glomeruli made of thin tubules - and with this disease, their work is disrupted.
I must say that with all today's promotion of a healthy lifestyle, kidneys are not talked about at all. The kidneys are an organ that removes food breakdown products and various chemical reactions from the body. They cleanse the blood from such decay products as creatinine and urea, normalize the content of trace elements (potassium, phosphorus, calcium), allowing them to maintain their balance and remove excess in the urine. The kidneys do their job thanks to the glomerular tubules, in which the blood is filtered. With kidney disease, these tubules suffer - and the worst thing is that they do not recover. They don't grow out like nails or hair; if they die, then for good. As a result, the body is not sufficiently cleansed and its intoxication with food decay products, muscle tissue (it is destroyed during exertion) and other things develops.
The degree of impairment is determined by the indicator of the glomerular filtration rate (GFR), that is, how the renal tubules work. The causes of kidney disease are completely different: high blood pressure, genetic diseases like polycystic kidney disease, severe alcohol and food poisoning when the kidneys cannot cope with a large amount of toxins, various infections, side effects of drugs such as diuretics or blood pressure lowering drugs. My illness has mixed causes, and it was difficult to establish a specific one - but I was glad that I was diagnosed and prescribed medications.
Every month I donate blood to the tissue bank of the Sklifosovsky Institute; there it is compared with all incoming cadaveric kidneys for compatibility. So, some may be "lucky" in three months, while others wait several years
Nevertheless, I did not see any manifestations of the disease at this stage, and I remembered it only once every few months, when my mother made me undergo tests for control and go to a nephrologist for a consultation. I lived a full life - I was actively involved in sports, ran ten kilometers a day, drank with friends, was fond of different dietary regimes - and my body did not give me any signs. Kidney disease is a very quiet disease that manifests itself when things have gone far.
At that time, I made many mistakes: the fact is that in order to inhibit kidney disease, it is very important to follow a low protein diet so as not to burden the kidneys (which is why the Ducan diet is dangerous). It is important to avoid strenuous exercise that raises blood creatinine levels, monitor blood pressure, and eat less salt. In my case, I also had to take blood thinning drugs - I also have thrombophilia, that is, a tendency to blood thickening. True, it is not a fact that dieting would help me to delay dialysis: my kidney failure had lasted twenty-seven years before it - and this is a very long time.
I realized the seriousness of the situation late, eight years after the diagnosis, when I already had the fourth stage of chronic kidney disease (there are five of them, and the fifth stage is terminal, when the kidneys simply do not work). Then I began to fanatically fight for what was left: I followed a protein-free diet, watched for edema, took care of myself as best I could. Then I found out what happens to a person when his kidneys fail - dialysis appears in his life or, if he is lucky to find a transplant on time, a kidney transplant.
With regard to transplantation, in our country a relative (from a close relative, and a husband or wife is not considered to be) or corpse organ transplant is allowed in our country. This area is strictly regulated by law, and transplants for money or even volunteering are prohibited by law. With related transplants, everything is quite clear: the donor and recipient are examined in detail, a transplant verdict is issued, and in case of a positive decision, a double operation is performed - one kidney is taken from the donor and implanted into the recipient.
With cadaveric transplants, everything is a little more complicated - if I'm not mistaken, we have one waiting list for the whole country. I live in Moscow, and now they are put on a waiting list in two clinics, but this is the same list. Many people mistakenly call it a queue, but it is not: the sequence of transplants depends on the receipt of suitable organs. Every month I bring a test tube of blood to the tissue bank of the Sklifosovsky Institute; within a month, it is compared with all incoming cadaveric kidneys for compatibility. Therefore, some may be "lucky" in three months, while others wait several years.

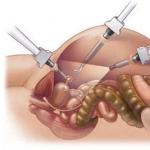
If it was not possible to make the transplant on time (and it is extremely rare, because a suitable kidney still needs to be found), then when the kidneys begin to fail completely, dialysis is performed. This is a procedure that mimics the work of the kidneys, that is, it cleans the blood from decay products and removes excess fluid. Dialysis is of two types: hemodialysis and peritoneal dialysis. In the case of hemodialysis, cleansing is performed by a dialysis machine, which draws blood, cleans it and returns it back - usually this procedure lasts four to five hours, and it is carried out three times a week in a special dialysis center. To purify blood efficiently, the speed must be quite high, and you cannot simply insert thick dialysis needles into a vein and thin-walled artery. Therefore, a so-called vascular access is formed on the hand - the vessels are sutured, forming an intense blood flow; this is called a fistula. The preparation of the fistula itself is a whole operation; then you need to train the hand with an expander in order to strengthen the walls of the formed vessel, but at the same time it is impossible to load too much.
When it turned out that I had the fourth stage of renal failure, I began to prepare for the coming of the fifth - and I would need dialysis. I knew all the symptoms of kidney failure by heart and constantly looked for them in myself: swelling, a strange taste in the mouth, a change in skin odor, weakness, dizziness, anemia, nausea, lack of appetite, weight gain due to internal edema. Nothing hurt me, but I was scared: the ring on my finger presses a little - is it really edema? I asked those close to me if my breath smelled, and generally pounded myself incredibly; all the time it seemed to me that tomorrow I would be on dialysis.
Two things helped to balance my psychological state: working with a psychologist and obtaining the most detailed information about dialysis and people who have already gone through it. Classes with a psychologist helped to distract from heavy thoughts and begin to assess their prospects soberly, without unnecessary drama. In terms of information, the forum of Dr. Denisov became a discovery for me. This is the place where people with kidney disease can talk to each other and ask any medical or psychological questions. I am very grateful to Dr. Denisov for this forum - this is a support group and a treasure trove of information for anyone with kidney failure.
Unfortunately, kidney disease does not develop linearly: against the background of relative stability, a sharp deterioration can occur. Thanks to the information from the forum, I realized that I need to form vascular access in advance - otherwise, you may find yourself in a situation where there is no access and dialysis is carried out for a long time through a subclavian catheter that goes directly to the heart vessels - this method is used, but ideally it is short-term. I plucked up my courage, went to the vascular surgeon, and had a fistula. Although the indicators still allowed me to live without dialysis, I was assigned to a dialysis station - they are in government institutions and commercial (but subsidized by the state). Any citizen of the Russian Federation has the right to such therapy at the expense of the state; in addition, a person on dialysis can receive the first group of disabilities, most often indefinitely. Free dialysis can be taken (by prior arrangement) in any city in the country, and this allows you to travel around Russia.
You cannot insert thick dialysis needles into a vein or thin-walled artery. Therefore, a "vascular access" is formed on the arm, a fistula - the vessels are sutured, forming an intense blood flow
Exactly one year after the formation of access, my doctor and I made a decision: it was time to start renal replacement therapy (that is, dialysis), without bringing the body to extreme stress. I did not want to go through intensive care and swelling of twenty to thirty kilograms, and I smoothly entered dialysis mode. My center is open 24 hours a day, six days a week, and it was possible to choose a suitable schedule; I was working and did not plan to stop, so I chose the evening shift. Transportation is provided for people in a very serious condition, but I travel myself. You come, change into comfortable clothes, weigh yourself, discuss your well-being with the doctor - and go to the dialysis room. Usually there are five or six (sometimes more) patients and a health worker who monitors the indicators, connects the devices, is responsible for sterilizing the machines after the procedures. Several doctors are always on duty in the center. Dialysis lasts several hours, during which time they are fed cookies and treated with tea; some take snacks with them. Some dialysis centers allow visitors.
I spend my four hours just like most people do on a regular evening at home: reading, watching TV shows, sleeping. I was lucky and after dialysis I feel very good - no headaches, no nausea. As for the restrictions, they have changed. If earlier I needed to eat less protein in order not to burden the kidneys, now I need a lot of protein, because many important components are washed out during dialysis. There is no need to be afraid for the kidneys - they will not get any worse. Now the main danger is heart problems. It is important to exclude sweet fruits, starchy vegetables, and not eat too many greens. There are real stories when a person on dialysis ate one and a half kilograms of grapes or a small melon and died: the kidneys do not work and do not excrete potassium, and because of its excess, the work of the heart is disrupted, and it can stop. I try to eat no more than one small vegetable a day and a minimum of fruit - sometimes some berries or an apple. Foods high in phosphorus (such as cheese) are not yet recommended, and it is important not to drink a lot of fluids. I still excrete urine, and with the right balance of dialysis and fluid intake, this state can be maintained for a long time, but sooner or later the kidneys will stop working. Excess fluid puts stress on the heart, leads to shortness of breath, swelling of internal organs, and you need to try to avoid this.
If you monitor your health and nutrition, everything will be fine. I’m thirty now and have been on dialysis for two years, but I know people who have been living this way for about twenty years. For a woman who needs dialysis, pregnancy is a huge risk. There are examples, but it is very difficult, and no one comes out of this story healthy. The woman has to do dialysis every day. It also happens that menstruation disappears on dialysis (I don't know the reasons), but it recovers after a kidney transplant. Without dialysis, a person dies of intoxication - and this happens quickly, in a week or a month.

I'll tell you about my life outside of dialysis: I have always been very active, loved to play sports and did not perceive myself as a sick person. I have several degrees in economics and marketing, I speak English fluently and some other languages. After my first education, I started to work and did not stop doing it. My profession is office, without physical exertion, it is quite suitable for my condition. In the last year before dialysis, the employer knew about my problem and supported me in every possible way; I am very grateful for this, because when I was worried about my future life on dialysis, at least the issue of employment did not press me. I tried to be as involved as possible in the work, I took her with me to the hospital if I went to the examination. When dialysis began, it had almost no effect on the work area - the only thing is that after late dialysis it is difficult to get up early.
Now I have changed my place, the employer does not yet know about my situation, and I am in no hurry to reveal my cards, because I see no reason. I cover the holes from the needles on my arm with a plaster or a long sleeve. In my free time I swim and do moderate cardio loads. I read books, go with friends to restaurants and exhibitions, to the cinema. It's just like everyone else - just several times a week I need to spend four to five hours in the dialysis room.
When I go to a government agency to receive disability benefits, they do not believe me that I am a disabled person of the first group. Some are silent, others say that people like me look very different. There are many elderly people on dialysis, and they often begin to lament how such a young girl ended up on dialysis. There are also many middle-aged men; my favorite story is how they get drunk hard before dialysis, and then sober as a glass go to work or home, as dialysis washed everything.
Great stress is going to the doctor with any other ailments. Whether it’s stomach pain or acne, everything is attributed to kidney failure: "What did you want, you are on dialysis." Some doctors do not even know what dialysis is, they brush it off and call it "innovation", although it has been used for several decades. Often the only adequate doctors who understand you are nephrologists: when you get dialysis, you understand that you are with these people for a long time and in their hands your health, well-being and life. Therefore, it is very important to think carefully about their work, to be interested in the processes in your body, to understand how a machine works - to be a conscious patient, and not an eternal complainant. With a proper attitude towards people comes respect and understanding on their part. Many patients mistakenly think that they are being tortured, that the apparatus only makes it worse - but these thoughts are only from ignorance. Dialysis is not a sentence, but a second chance at life.
Any discomfort is written off
on renal failure: "What did you want, you are on dialysis." Some doctors do not even know what dialysis is and call it "innovation", although it has been used for several decades
In the last year before dialysis, I was depressed and under the weight of fear. My boyfriend at that time tried to support me, but he could not cope with the fact that it is simply dangerous for me to have children now. We separated during the pre-dialysis period. Now I am in a different relationship and very happy: my partner understands my situation, accepts me and tries to help in everything. It is very important to have support and support - in my case, these are my parents, my beloved man and close friends who listened for hours to my fears, tears and endless stories.
I have traveled all my pre-dialysis life. It is possible now, but additional expenses are needed: I have to plan and pay for dialysis abroad. Depending on the country, one procedure costs two to five hundred dollars; there are agencies that help organize this. I have already traveled on dialysis; the devices are arranged approximately the same, it is important to set the usual settings, and then everything will go well.
It can be hard and sad for me, because I would like to have time and do more, but I do not have enough energy or time. I scold myself, sometimes I regret it, but more often I try to find ways to better organize my time. I am grateful that I have been given the chance to live life to the fullest in such circumstances, and I try to use this chance. Perhaps I will not become known as Stephen Hawking or Nick Vuychich, and I will not have billions of dollars in income, but I manage to lead a full life and enjoy it no less than healthy people, see prospects and make plans - and this is already a small victory.
I want to convey to those who are faced with the same situation that they are not alone and that there is life on dialysis. I talked with girls of my age who were on dialysis after resuscitation or living with kidney failure and know what may lie ahead. They are all very scared and it seems that there is no further life. These are tears, depression and, literally, a desire to lay hands on oneself. I thought so too, but you really don't need to be afraid. You need to collect information and learn to accept circumstances, live with them and enjoy life in spite of everything.
The kidneys are a complex mechanism. Their functioning is essential for a healthy life. Kidney hemodialysis is needed in case of a decrease in the functioning of an organ, when chronic processes of urine separation in the body lead to the fact that the kidneys cannot cope with the purification of blood from harmful metabolic results, poisons poison the blood, it is impossible to live without help and a person can become disabled.
What is kidney hemodialysis?
Nephrology and dialysis is a branch of science that studies the principles of work and kidney disease. Nephrology considers the principle of diagnosis, treatment, prognosis of recovery and the ability to live with the problem. Dialysis is the last chance to live before transplantation. Kidney hemodialysis is an extracorporeal method of blood purification from toxic elements, toxins (urea, creatinine, poisons), carried out outside the body in acute renal failure.
The essence of hemodialysis is to urgently cleanse the body and regulate the violation of the water-electrolyte, acid balance, and improve human life. In the last stages of oncology, it relieves intoxication.
Types of procedures
Depending on the venue
In a home environment
Special equipment (new System One) allows you to replace the natural filter and purify the blood every day at home. The process lasts 2-4 hours. Hemodialysis at home - a software method that improves the quality of life, can replace organ transplant surgery. In our country, due to the high cost, connecting the installation of a house is not very popular, although a disabled person cannot always get to the hospital.
- Pros: easy to use (the One system weighs no more than 30 kg), it is possible to combine the time of the procedure and the needs of the body, the likelihood of complications in the form of hepatitis decreases.
- Cons: high cost of equipment, not all people can use vascular needles, training is necessary.
On an outpatient basis
 The duration of one stage procedure takes 4 hours.
The duration of one stage procedure takes 4 hours. The procedure is carried out in a special clinic 3 times in 7 days. The duration of one stage takes 4 hours. This method is needed for a person with acute insufficiency of kidney function or at the stage of a chronic process when it is impossible to restore the functionality of the organ. Consider how many advantages the procedure has:
- Pros: monitoring specialists, tracking test results to adjust treatment (low creatinine in urine, creatinine in the blood, anemia), sterile cleanliness of the room, the ability to deliver a disabled patient for treatment and home (if necessary).
- Cons: visiting the clinic several times a week, waiting in line, small risk of contracting hepatitis.
In the hospital
This type of therapy is used for patients with severe poisoning of the body, improving the functioning of the liver and kidneys. In any clinic, there are rooms with artificial kidney equipment. Technically, a blood purification operation in a hospital does not differ from an outpatient one. Moreover, the equipment used for filtering is the same.
- Pros: constant supervision of specialists.
- Cons: the need to stay in the hospital, the possibility of contracting hepatitis is great.
Depending on the functionality of the device
Conventional dialysis
Filtration is done using equipment based on a cellulose membrane with a size of 0.8-1.5 sq.m. Using a low flow filter allows small particles to pass through. The blood flow rate is low and reaches 200-300 ml per minute. It takes 4-5 hours.
Highly effective dialysis
Hemodialysis is done with a machine called a dialyzer. Dialyzer surface size 1.5-2.2 sq.m. Blood moves at a speed of up to 350-500 ml per minute, dialysate is directed in the opposite direction, a speed of 600-800 ml per minute. By increasing the effectiveness of the membrane, the blood flow rate increases, the application time decreases to 3-4 hours and the number of procedures per week.
Hemodialysis using highly permeable membranes
 During the procedure, the patient's blood is repeatedly passed through the dialyzer.
During the procedure, the patient's blood is repeatedly passed through the dialyzer. In this form, hemodialysis and hemofiltration are combined. The bottom line is to use special highly permeable surfaces. High-flux hemodialysis facilitates the passage of large molecules. The highly permeable membrane reduces the likelihood of complications. But the likelihood of substances from the dialysate entering the blood increases, so a sterile apparatus is needed.
In medicine, an alternative to the above-described hemodialysis is the peritoneal method. It is worth replacing hemodialysis with the peritoneal method in case of individual intolerance, when it is impossible to get access to the connection of the "artificial kidney" apparatus. It is often used in oncology. No need to use expensive sets of instruments, the abdominal cavity acts as a filter in the peritoneal method. The method of peritoneal filtration has disadvantages:
- duration;
- the risk of contracting an infection;
- development of peritonitis.
Indications for
Not every disease needs extracorporeal filtration. The prescriptions for carrying out are determined strictly and include signs of the following conditions:
- renal failure (acute or chronic);
- with severe poisoning (alcohol, poison, drugs);
- significant changes in the electrolyte composition of blood plasma;
- excess water content in the body (lungs swell).
Chronic renal failure (CRF) cannot be cured by conservative methods; disability is assigned. Without hemodialysis, the quality of life deteriorates, and death occurs.
The main indicator for cleansing procedures for renal pathologies are indications:
- with creatinine in the blood of more than 1 μmol per liter;
- urea 20-40 mmol per liter;
- filtration rate less than 5 ml per minute.
Contraindications
 Hemodialysis is contraindicated in active pulmonary tuberculosis.
Hemodialysis is contraindicated in active pulmonary tuberculosis. There are situations in which, in the presence of the above indications, the hemodialysis procedure is not performed. For example, complications are likely to occur during pregnancy. But with the development of sudden acute insufficiency already during pregnancy, there is no way out, the installation of an "artificial kidney" is connected. An emergency case has no contraindications. Contraindications for conducting:
- Absolute:
- cirrhosis of the liver;
- active pulmonary tuberculosis;
- diseases dangerous by the sudden onset of heavy bleeding.
- Relative:
- insane conditions (seizures, schizophrenia, mental illness);
- advanced oncology;
- blood pathology (anemia, oncology);
- serious nervous disorders;
- pregnancy;
- age restrictions (over 80 years old or with diabetes mellitus 70 years old);
- acute alcohol or drug addiction syndrome;
- the presence of two or more violations.
Dialysis machine and special solution
For the extracorporeal filtration procedure, artificial kidney machines (dialyzers) are used. The main task of the set of equipment is to purify blood from urea, the end product of protein metabolism, calcium, potassium, sodium, water. In modern medicine, equipment designs are diverse. The set includes: a dialyzer, a blood supply system, a system for preparation and supply of a special solution under pressure. The devices differ in the structure of the semi-permeable membrane.
Plate type dialyzer
 The system consists of lamellar grooves through which acid dialysate passes. The plates are interconnected by vertical cylindrical channels, covered with a membrane on top. Liquid flows through the plates, and blood flows through the membrane. The device is difficult to manufacture, but its operation has several advantages:
The system consists of lamellar grooves through which acid dialysate passes. The plates are interconnected by vertical cylindrical channels, covered with a membrane on top. Liquid flows through the plates, and blood flows through the membrane. The device is difficult to manufacture, but its operation has several advantages:
- slight opposition to blood flow, reducing the risk of blood clots;
- the dosage of the anti-clotting drug is reduced;
- free control of the degree of filtration;
- filling the dialyzer does not require a large volume of blood, so the body is not deficient.
Capillary dialyzer
The most efficient and safest apparatus. Used sets of synthetic, biologically inactive materials for the manufacture of the membrane. A set of parallel tubes represents a system that allows blood to pass through. Their number reaches 10 thousand, diameter 0.3 mm. Outwardly, in the opposite direction, dialysate fluid flows. Thanks to this design, the cleaning quality is higher.
If hemodialysis is being performed in children or the initial procedure in adults, a lightweight programmed filtration method is used, in which the hemodialysis concentrate is directed along the blood flow. This reduces discomfort and the likelihood of negative consequences.
Capillary device advantages:
- high quality, achieved by a large filter surface;
- constant circulation and purity of the dialysis fluid, which reduces the likelihood of contamination of the blood by viruses, germs and bacteria. Before the operation, the patient must be examined in the clinic. Blood pressure, body temperature and pulse are measured. During, after the procedure, the indicators of a person's well-being are monitored. Preliminarily, in 7 days, prepare the vascular access (prostheses). Arteriovenous fistula formation is the most common. A fistula for hemodialysis is formed in the vessel. It is located under the skin, resembling a cord. An alternative to a fistula is the use of prostheses. A synthetic material is used to form a prosthesis. Access operations (for example, a prosthesis) are performed by a doctor in the operating room.
The procedure goes through the stages:
- Preparation of equipment and material.
- The person lies down in a special chair in a reclining position.
- The device is installed next to the chair. The venovenous or arteriovenous line communicates it with the body.
- The operation of the pump creates pressure, under which the blood is removed into the filter for contact with a special liquid.
- Purified blood is returned to the body through the connected second vein.
How much filtration is needed depends on the severity of the disease. One procedure is enough for some, while others need chronic hemodialysis. Usually, blood purification is carried out up to 3 times a week with a duration of 4-5 hours. The mode, the time of hemodialysis is set according to individual indicators. The adequacy of hemodialysis consists of biochemical and other blood parameters. An antibiotic may be administered to avoid infection. At the end of the procedure, a bandage is applied to the site of access to the vessels.
Currently, 1000 kidney transplants are performed annually in Russia.
While awaiting transplantation, about 24,000 patients are living on hemodialysis, their non-working kidneys are replaced by a machine. One of these patients agreed to tell us about his daily life.
The neighbor says: “Why is the ambulance coming for you? You work for it or something. " It turns out that I work. The patient.
15 291 is my code. Every dialysis patient gets this number. When I call a transport ambulance and order a transfer, I call this number, and at the other end of the line everyone immediately understands. Two or three words, and: "Order accepted." Transport is well organized, it's a sin to complain.
You need to get dialysis every other day by a certain time, regardless of traffic jams, you can't be late. Either an ambulance or a bus with a red cross comes for me, the same ambulance, but without the right to overtake, drive through a red light. I live in the center, and my dialysis center is on Shchukinskaya. The road takes about an hour, if there are traffic jams, then more. There is no choice. There is a map of Moscow dialysis centers on the Internet. The center and east are the “big white spot”. There are only departmental ones - not for us.
In the provinces, dialysis is more difficult, from small towns they are taken to the region, a bus is assembled and brought to the regional hospital. It takes a whole day to get there. There are fewer hemodialysis centers in Russia than we would like, and if a person has renal failure, it is better for him to move closer to dialysis.
In fairness, I must say that in addition to hemodialysis, there is also peritoneal dialysis, when a container with a solution is sewn into the stomach, tubes are taken out, and the patient must periodically change this solution. But, as they say, it takes a lot of time, only managed to fill it, and it's time again. Moreover, this must be done in a sterile room, which must be quartzated all the time. With such dialysis it is quite easy to earn peritonitis, however, they say that the peritonitis there is not as severe as in other cases.
Patients with renal failure do not immediately go to dialysis, but only when the kidneys are no longer able to cope with the load. A year ago, I had a fistula, an entrance for the apparatus, for this they performed an operation on the vessels, I now have such a thing on my arm, it hums like a motor. I still, frankly, have not understood all this physics and chemistry. When connected to the device, a needle is inserted into this one arm, near the fistula, one into a vein, the other into an artery. But this fistula can deteriorate over time. For some, it takes off after a couple of months, for others it lasts for several years. When it falls into disrepair, and it is done again, in another place.
In the hospital, where I had a fistula, I ended up in a two-bed ward. And they put Vasya to me. He came to Moscow to work, worked somewhere in a warehouse, and apparently lived there. He was a simple, dirty, smelly man. He seemed to know that he had kidney problems, but endured to the last. They brought me straight from work, he just moaned and wheezed: "That's it, I say goodbye to life." He would have said goodbye if not for our good doctor Kolya. True, Kolya was later reprimanded by colleagues: “Why did you take some bum?” But they saved Vasily, gave him pieces of paper and wrote him out, like they sent him to the place of registration. Where he went there, I don't know. And then I had another neighbor. Such a dialysis veteran, all cut, he has been on dialysis for ten years, but nothing, cheerful.
I drive around Moscow in an ambulance, when with flashing lights, when not. They say that from the new year we will be deprived of the ambulance and we will travel by bus. The buses are 6-seater, and they have already tried to load six of us once. Two aunts from Novokosino, looked at this case, said: "Well, no, we'll come home in three hours, better on our own." But this is the only time, however, usually 2-3 people are carried. As a rule, you travel with the same people
Although without delay, it turns out quite long. I have a connection at two, but I have to be in place at half past one, go through a doctor's examination, weigh in, change. They take me away at 12 o'clock, or even earlier. The procedure takes me 4.5 hours. In fact, a whole working day is spent on this. I return home at nine o'clock.
The dialysis center operates around the clock, in four shifts. It is believed that day shifts are for those who do not work, and evening and night shifts for those who are younger. It turns out that many people combine dialysis with work, work during the day, dialysis at night.
I've been on dialysis for a year now. I'm waiting in line for a kidney transplant. The average waiting period for Moscow is three years. In the regions it is worse, the patients there, when the turn comes, go to Moscow and wait here. This can take several years. Sometimes the patient lives in a hospital, who can rent a house. It happens that a patient's health condition worsens, and he lives in limbo. Leaving means losing the queue, and they cannot transplant a kidney to him with deterioration either. There are kidney transplant centers in Moscow, St. Petersburg, and, it seems, in two or three other cities. So Muscovites are lucky. There are three such centers in Moscow.
Personally, I am not particularly eager for a transplant. Waiting for my turn calmly. The people with whom I communicate have had mostly negative experiences, which is understandable, those who are doing well do not return to dialysis.
I talked, for example, with a woman who had a kidney transplant in 2010, and she practically did not stand in line for a transplant, only three months. Transplanted in Sklif. They say that Sklif is the best, but, nevertheless, it did not go well. It was that summer when the peat bogs were burning and the kidney did not take root. The woman suffered this year with a transplanted kidney, she says, she felt very bad, she was in torment all year. Those who have gone through a kidney rejection are already quite skeptical about the prospect of a transplant. But I mostly communicate with pensioners. Young people have different views, they have not lived yet, a transplant for them is a chance, of course.
They die, of course. Once a man died in my presence - his heart seized. He was sitting on the sofa in the lobby, waiting for a pre-dialysis medical examination, and suddenly his wife shouts: "Petya, Petya!" And Petya - everything. They pumped it out, we must pay tribute to them, probably, about 40 minutes. And an additional ambulance arrived, and the local doctors themselves pumped it out.
Of course, dialysis is not a panacea, deterioration gradually begins: phosphorus accumulates, potassium. One died in the spring. A normal guy, not a disabled person, nevertheless, died suddenly. An excess of potassium is a violation of the heart rhythm.
Our life is with certain restrictions, the diet must be monitored, the level of potassium and phosphorus. And so that calcium is not too little. I take a whole box of medicines. I can't leave Moscow anywhere. That is, you can, but where there is dialysis, but for this you need money for dialysis and for rest.
But on dialysis people live for decades and are happy that they are alive. I go to the ambulance with my grandmother, she is over 70, 10 years old on dialysis, lives. Fine. And yet, God willing. Not that we are all such optimists and lovers of life ... But, on the other hand, everyone understands that if it were not for dialysis, then everything is already, a cemetery. This time for us is extra, like in football. So - I live!
Most current guidelines require hemodialysis at least 3 times per week and at least 12 hours per week (unless the patient has significant residual renal function). There is strong evidence that, in at least some clinical situations, more frequent and / or prolonged dialysis provides significant benefits. These situations include:
Hemodynamic instability or instability of cardiovascular pathology
Arterial hypertension despite the maximum achievable level of dehydration
Poor control of phosphate levels
Protein-energy malnutrition uncorrected by other measures
The available options for increasing / lengthening dialysis are:
Prolonged dialysis (\u003e 5.5 hours) 3 times a week
Increased dialysis (4-5 times a week)
Short daily dialysis (2-3 hours 6-7 times a week)
· Long night ("nightly") dialysis 6-8 hours 6-7 times a week
The ideal duration and frequency of dialysis sessions can be determined only on the basis of a balance between the interests of the quality of treatment (deepening of cleansing and increasing tolerance with an increase in the frequency and duration of treatment) and the restrictions introduced to the style and quality of life of patients by such an increase in the time spent on treatment. Adequate randomized controlled trials on this issue have not been conducted, especially since it is not very clear what should be determined by the endpoints of the study: along with survival, additional costs must be taken into account: time, social, economic. Nevertheless, certain recommendations can be made now.
Uncontrolled studies indicate the possibility of improving the control of arterial hypertension, reducing intradialysis complications, improving nutritional status and increasing survival by extending dialysis to 8 hours (3 times a week). Increasing the session time decreases the UV rate and can lead to improved hemodynamic stability, especially in the elderly. The same randomized study, however, recorded an increase in other intradialysis symptoms with 5-hour dialysis: headache, nausea, back pain and itching. In randomized prospective studies with lengthening dialysis time, improvement in hypertension control was achieved both with a decrease in extracellular volume and without a change in dry weight.
The lengthening of dialysis sessions minimally affects the removal of easily diffusing low molecular weight substances (urea, etc.), but is significant for substances predominantly located in the intracellular sector (phosphates) and medium molecular substances (β 2 -microglobulin). Extension of the session does not improve endothelial function.
Convincing evidence of the effect of moderate lengthening of dialysis time on survival has not yet been obtained. In the Japanese dialysis registry, extending the time to 5.5 hours (3 times per week, adjusted for the supplied dialysis dose) was associated with increased survival. The difficulty in assessing the effect of time lies in the fact that it is difficult to separate it from the effect of increasing the dose of dialysis.
Most studies on increasing the frequency of dialysis sessions have been conducted in a small number of patients and over a short period of time, so there is no convincing evidence of the potential benefits of this approach. It should be noted that in the presence of a series of publications on the positive effects of increasing the frequency of dialysis, evidence of risks and dangers was not obtained. Increasing the frequency of sessions makes it easier to achieve target weight in unstable dialysis patients with high comorbidity, increasing session tolerance (convulsions, weakness, headaches) and reducing the incidence of hypotension. Daily dialysis can reduce the dose and frequency of antihypertensive drugs, as well as reduce the severity of left ventricular hypertrophy, probably due to better control of water balance. Daily dialysis improves nutritional parameters and appetite, effectively reduces phosphate levels (with a duration of more than 2 hours daily; shorter daily sessions, increasing the excretion of phosphates, do not lead to a decrease in their concentrations, possibly due to an increase in the intake of phosphate from food associated with an improvement appetite). Daily dialysis helps to reduce the levels of pro-inflammatory factors, markers of oxidative stress, homocysteine, proteins associated with uremic toxins. Daily dialysis improves quality of life, and patients rarely wish to return to a standard regimen. Sometimes the positive effect of daily dialysis is associated with "positive" patient selection for this modality (more motivated, with better treatment compliance). All the more valuable is the observation, where a positive effect on the control of blood pressure, anemia, QoL and survival was achieved with a “negative” selection (patients with the greatest comorbidity).
The possible negative effects of frequent dialysis are associated with organizational problems, cost, and more frequent use of vascular access. The cost of more frequent dialysis may become comparable to the standard one, given the likely decrease in the need for expensive drug therapy (erythropoietins, phosphate binders and calcimimetics, antihypertensive drugs), as well as in hospital treatment. If “standard” dialysis does not consider the need for expensive drug therapy, and the cost of full-fledged inpatient treatment is ignored, frequent dialysis will certainly lose in cost to “standard” dialysis, however, in this situation, the clinical benefits for certain categories of patients may outweigh the economic arguments ... In relatively short-term observations, the deterioration of the "survival" of the vascular access was not recorded, however, this issue may become relevant among the long-term consequences of frequent dialysis.
The first kidney hemodialysis was carried out back in 1960 and since then this is the only medical invention that completely replaces the functions of a human internal organ.
Many have probably heard about the procedure and know that the apparatus on which the blood is purified from accumulated toxins is called an "artificial kidney". The correct name, because with hemodialysis, the blood is purified similarly to what the kidneys would do if they did not fail.
Modern hemodialysis department
What is a kidney hemodialysis machine?
Yes, you understood correctly. If a person's kidneys fail, he will not die, but will be able to live. Someone thinks that this is an inferior life, because a sick person has to be attached to the apparatus. On the contrary, patients who have received indications for hemodialysis thank both God and technical progress for the opportunity to continue living in the hope of waiting for a transplant.
It's important to know! The kidneys are obliged by nature to purify the blood and hemodialysis is a method in which the human body is cleansed without the involvement of the kidneys. During the procedure, toxins and toxins are removed, the water and electrolyte balance is normalized.
It is based on metabolism through a special membrane, in which blood flows through one side, and dialysis solution through the other. The artificial kidney apparatus consists of:
- dialyzer;
- device through which blood is supplied;
- the device in which the dialysate is prepared and through which it is delivered.
The device has a roller pump that delivers blood through the tubes to the dialyzer. Instruments are configured in the system to measure the pressure and speed of the incoming blood. The optimal speed is about 300-450 ml per minute. The prepared hemodialysis solution flows near the membrane in the opposite direction from the blood flow at a rate of approximately 500 ml per minute.
Attention! The composition of the dialysis solution is similar to that of blood plasma. It can be adjusted depending on the patient's blood electrolyte level. The content of calcium, chlorine, bicarbonate practically never changes, more often it is necessary to regulate potassium. In order for the amount of fluid removed from the blood to be normal, the sodium supply to the solution increases or decreases.
How is the procedure performed?
Attention! Before starting hemodialysis, each patient is examined by a doctor, his pressure, temperature and pulse are recorded. In the process and for some time after completion, the patient also remains under observation so as not to miss a possible deterioration in his well-being.

How renal hemodialysis works
A week before the start of the patient, a fistula is installed in the desired vessel (dialysis access is obtained), and hepatitis is vaccinated for prophylactic purposes. The procedure itself is as follows:
- The patient is placed in a reclining position in a special chair.
- There is an apparatus near the chair, which is connected by a veno-venous or arterial-venous route.
- With the help of a pump, blood is removed into the dialyzer, where it comes into contact with the solution.
- Through another vein, the purified blood is returned back to the body.
How often should you visit the hemodialysis room? It all depends on the severity of the disease. In some cases, one procedure is enough for qualitative changes to occur in the kidneys, in others it is an appointment for life. The frequency depends not only on the diagnosis, but also on the patient's age, weight and height, and some other circumstances.
There are different membranes that differ in the size of the usable surface. Because of this, hemodialysis of the kidneys can be carried out according to different programs - from a daily procedure of 2 hours to 2 times a week. The regime is determined individually, but most often there is a three-time visit per week to the hemodialysis room with a duration of 4-5 hours.
Is hemodialysis possible outside the hospital?
This is an outpatient procedure, but there are also portable machines that allow hemodialysis at home. Numerous cases are known when patients at their own expense purchased “artificial kidney” devices so as not to be dependent on the medical center.
The advantage of the home apparatus is that the patient's mode of life is not particularly disturbed, you can not think too much about following the diet. The portable device can be installed anywhere - not only at home, but also at work or on the road. There is no need to prove that a sick person will be much more comfortable undergoing treatment at home.
There is one drawback of home kidney hemodialysis and that is the cost of installation and consumables. For this reason, there is no particular distribution in our country, but portable "artificial kidneys" are widely used abroad. People continue to live a full life, travel, go on business trips, their usual routine is not disturbed due to visits to the clinic.
Who is the procedure indicated for?
If hemodialysis of the kidneys is prescribed by the attending physician, should the procedures begin immediately or is there time for reflection? Delay can be disastrous, so treatment cannot be postponed.
Attention! The psychological component is important. If the patient understands the seriousness of the situation, is psychologically prepared, one can hope for a greater effect from the hemodialysis.
The main indications for hemodialysis are acute renal failure, in addition, the procedure is indicated for:
- chronic renal failure;
- drug overdose;
- severe poisoning with poisons, drugs, alcohols;
- overhydration that threatens human life;
- significant changes in blood composition in terms of electrolytes;
- shock due to trauma.
Need to know! Most often, we do hemodialysis, where the indication is chronic renal failure at the final stage, when the kidneys completely lose the ability to filter blood and poisons begin to poison the body.

Kidney hemodialysis procedure
It would be ideal if hemodialysis could be performed for all patients in need, but contraindications exclude this possibility. The procedure has absolute and relative contraindications.
Absolute contraindications for:
- malignant neoplasms;
- severe lesions of the nervous system;
- schizophrenia, epilepsy;
- age 80 and older;
- over 70 years of age with diabetes mellitus;
- the presence of several concomitant pathologies;
- serious diseases of the circulatory system.
Relative contraindications - with an active form of pulmonary tuberculosis and with diseases when massive bleeding may occur - uterine fibroma, stomach ulcer, Melory-Weiss syndrome.
Attention! Alcoholism and drug addiction are contraindications if the doctor notices the patient's lack of interest in starting a new life, if the patient is not looking for ways to socially rehabilitate.
The procedure has numerous complications due to a sharp decrease in plasma osmotic pressure and blood levels of calcium, sodium and potassium:
- heart rhythm disturbances;
- allergic reactions;
- epileptic seizures;
- nausea, vomiting;
- loss of consciousness;
- convulsions, stunning;
- arterial hypertension and hypotension.
Minor complications are resolved by changing the program so that the rate of blood flow decreases in the process. But during treatment, local complications associated with infection may also arise. Rarely, septic embolism, bacterial endocarditis, and similar problems occur.
How to eat during hemodialysis procedures?
Not only the procedure itself is important, but also a strict diet before and after it, since proper nutrition during hemodialysis makes it possible to preserve the result of treatment. For exact recommendations, ask your doctor.
The special diet is based on:
- restriction of foods that contain calcium, potassium, phosphorus;
- exclusion of preparations containing aluminum;
- strict control of the volume of water drunk during the day;
- almost complete rejection of salt;
- consumption of a lot of protein foods, but on certain schedules.
Attention! There are a lot of restrictions in the diet, so the patient should keep a food diary, where he will indicate all the foods consumed during the day and the amount of water drunk. Do not forget that first courses are also liquid.