Type 2 diabetes- symptoms and treatment
What is type 2 diabetes? We will analyze the causes of occurrence, diagnosis and treatment methods in the article of Dr. Khitaryan A. G., a phlebologist with an experience of 34 years.
Definition of disease. Causes of the disease
Epidemic diabetes(SD) has been going on for quite some time. According to the World Health Organization (WHO), in 1980 there were about 150 million people on the planet suffering from diabetes, and in 2014 - about 421 million. Unfortunately, the trend towards regression of incidence over the past decades has not been observed, and today we can safely say that DM is one of the most common and serious diseases.
Type II diabetes- a chronic non-infectious, endocrine disease, which is manifested by profound disorders of lipid, protein and carbohydrate metabolism associated with an absolute or relative deficiency of a hormone produced by the pancreas.
In patients with type II diabetes, the pancreas produces a sufficient amount of insulin, a hormone that regulates carbohydrate metabolism in the body. However, due to a violation of metabolic reactions in response to the action of insulin, a deficiency of this hormone occurs.
Insulin-dependent type II DM has a polygenic nature, and is also a hereditary disease.
The cause of this pathology is a combination of certain genes, and its development and symptoms are determined by concomitant risk factors, such as unbalanced nutrition, low physical activity, constant stressful situations, age from 40 years.
The growing pandemic of obesity and type II diabetes are closely linked and represent major global health threats in society. It is these pathologies that are the causes of chronic diseases: coronary heart disease, hypertension, and hyperlipidemia.
If you experience similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Type 2 diabetes symptoms
Most often, the symptoms of type II diabetes are mild, so this disease can be detected thanks to the results of laboratory tests. Therefore, people belonging to the risk group (presence of obesity, high pressure, various metabolic syndromes, age from 40 years), you should undergo a routine examination to exclude or timely detect the disease.
The main symptoms of type II diabetes include:
- permanent and unmotivated weakness, drowsiness;
- constant thirst and dry mouth;
- polyuria - frequent urination;
- increased appetite (during the period of decompensation (progression and deterioration) of the disease, appetite decreases sharply);
- skin itching (in women often occurs in the perineum);
- slow healing wounds;
- blurred vision;
- limb numbness.
The period of decompensation of the disease is manifested by dry skin, a decrease in firmness and elasticity, and fungal infections. Due to abnormally elevated lipid levels, skin xanthomatosis (benign neoplasms) occurs.

In patients with type II diabetes, the nails are prone to brittleness, loss of color or the appearance of yellowness, and 0.1 - 0.3% of patients suffer from lipoid necrobiosis of the skin (deposits of fat in the destroyed areas of the collagen layer).
In addition to the symptoms of type II diabetes itself, symptoms also make themselves felt late complications diseases: ulcers on the legs, decreased vision, heart attacks, strokes, damage to the vessels of the legs and other pathologies.
The pathogenesis of type 2 diabetes
The main cause of type II diabetes is insulin resistance(loss of cell response to insulin), due to a number of environmental factors and genetic factors, occurring against the background of dysfunction of β-cells. According to research data, with insulin resistance, the density of insulin receptors in tissues decreases and translocation (chromosomal mutation) of GLUT-4 (GLUT4) occurs.
Elevated levels of insulin in the blood hyperinsulinemia) leads to a decrease in the number of receptors on target cells. Over time, β-cells stop responding to rising glucose levels. As a result, a relative deficiency of insulin is formed, in which carbohydrate tolerance is impaired.
Insulin deficiency leads to a decrease in the utilization of glucose (sugar) in tissues, an increase in the breakdown of glycogen to glucose and the formation of sugar from non-carbohydrate components in the liver, thereby increasing glucose production and aggravating hypoglycemia- a symptom characterized by high blood sugar.

The endings of peripheral motor nerves secrete a calcitonin-like peptide. It contributes to the suppression of insulin secretion by activating ATP-dependent potassium channels (K+) in the membranes of β-cells, as well as the suppression of glucose uptake by skeletal muscles.
An excess level of leptin, the main regulator of energy metabolism, contributes to the suppression of insulin secretion, leading to insulin resistance of skeletal muscles to adipose tissue.
Thus, insulin resistance includes various metabolic changes: impaired carbohydrate tolerance, obesity, arterial hypertension, dyslipoproteinemia and atherosclerosis. The main role in the pathogenesis of these disorders is played by hyperinsulinemia, as a compensatory consequence of insulin resistance.
Classification and stages of development of type 2 diabetes
Currently, Russian diabetologists classify DM according to the degree of severity, as well as the state of carbohydrate metabolism. However, the International Diabetes Federation (IDF) quite often makes changes in the goals of diabetes care and the classification of its complications. For this reason, Russian diabetologists are forced to constantly change the classifications of type II diabetes accepted in Russia according to the severity and degree of decompensation of the disease.
There are three degrees of severity of the disease:
- I degree - symptoms of complications are observed, dysfunction of some internal organs and systems. Improving the condition is achieved by following a diet, prescribing drugs and injections.
- II degree - complications of the organ of vision appear quite quickly, there is an active release of glucose in the urine, problems with the limbs appear. Drug therapy and diets do not give effective results.
- III degree - glucose and protein are excreted in the urine, kidney failure develops. To this extent, the pathology is not treatable.
According to the state of carbohydrate metabolism, the following stages of type II diabetes are distinguished:
- compensated - a normal blood sugar level achieved with the help of treatment, and the absence of sugar in the urine;
- subcompensated - the level of glucose in the blood (up to 13.9 mmol / l) and in the urine (up to 50 g / l) is moderate, while there is no acetone in the urine;
- decompensated - all indicators characteristic of subcompensation are significantly increased, acetone is detected in the urine.
Complications of type 2 diabetes
TO acute complications Type II diabetes includes:
- Ketoacidotic coma is a dangerous condition in which total intoxication of the body with ketone bodies occurs, as well as metabolic acidosis (increased acidity), acute liver, kidney and cardiovascular failure.
- Hypoglycemic coma is a state of depression of consciousness that develops with a sharp decrease in blood glucose below a critical level.
- Hyperosmolar coma - this complication develops within a few days, as a result of which metabolism is disturbed, cells are dehydrated, and the level of glucose in the blood increases sharply.
Late complications of type II diabetes are:
- diabetic nephropathy (kidney pathology);
- retinopathy (damage to the retina that can lead to blindness);

- polyneuropathy (damage to the peripheral nerves, in which the limbs lose sensitivity);
- diabetic foot syndrome lower limbs open ulcers, purulent abscesses, necrotic (dying) tissues).

Diagnosis of type 2 diabetes
In order to diagnose type II diabetes, it is necessary to assess the symptoms of the disease and conduct the following studies:
- Plasma glucose determination. Blood is taken from a finger, on an empty stomach. A positive diagnosis of type II diabetes is established in the presence of glucose over 7.0 mmol / l when the analysis is carried out two or more times on different days. Indicators may vary depending on physical activity and food intake.
- Glycated hemoglobin (HbAc1) test. Unlike blood sugar readings, HbAc1 levels change slowly, so this test is a reliable method for diagnosing as well as monitoring the disease. An indicator above 6.5% indicates the presence of type II diabetes.
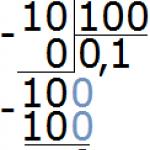
- Urinalysis for glucose and acetone. In patients with type II diabetes, daily urine contains glucose, it is determined only if the level of glucose in the blood is elevated (from 10 mmol / l). The presence of three or four “pluses” of acetone in urine also indicates the presence of type II diabetes, while this substance is not found in the urine of a healthy person.
- Blood test for glucose tolerance. It involves determining the concentration of glucose two hours after taking on an empty stomach a glass of water with glucose dissolved in it (75 g). The diagnosis of type II diabetes is confirmed if the initial glucose level (7 mmol / l or more) after drinking the solution increased to at least 11 mmol / l.
Type 2 Diabetes Treatment
Treatment of type II diabetes involves the solution of the main tasks:
- compensate for the lack of insulin;
- correct hormonal and metabolic disorders;
- treatment and prevention of complications.
To solve them, the following methods of treatment are used:
- diet therapy;
- physical exercise;
- the use of hypoglycemic drugs;
- insulin therapy;
- surgical intervention.
diet therapy
A diet for type II diabetes, like a regular diet, involves the optimal ratio of the main substances contained in the products: proteins should make up 16% of the daily diet, fats - 24%, and carbohydrates - 60%. The difference in the type II diabetes diet lies in the nature of the carbohydrates consumed: refined sugars are replaced by slowly digestible carbohydrates. Since this disease occurs in overweight people, weight loss is the most important condition that normalizes blood glucose levels. In this regard, a caloric diet is recommended in which the patient will lose 500 g of body weight weekly until the ideal weight is reached. However, the weekly weight loss should not exceed 2 kg, otherwise it will lead to excessive loss of muscle rather than adipose tissue. The number of calories needed for the daily diet of patients with type II diabetes is calculated as follows: women need to multiply the ideal weight by 20 kcal, and men by 25 kcal.
When following a diet, it is necessary to take vitamins, since during diet therapy there is an excess excretion of them in the urine. The lack of vitamins in the body can be compensated with the help of rational use useful products such as fresh herbs, vegetables, fruits and berries. In winter and spring, it is possible to take vitamins in yeast form.
A correctly selected system of physical exercises, taking into account the course of the disease, age and present complications, contributes to a significant improvement in the condition of the patient with diabetes. This method of treatment is good because the need for the use of insulitis is practically eliminated, since during physical exertion glucose and lipids are burned without his participation.
Treatment with hypoglycemic drugs
To date, derivatives of hypoglycemic drugs are used:
- sulfonylurea ( tolbutamide, glibenclamide);
- biguanides, which reduce gluconeogenesis in the liver and increase the sensitivity of muscles and liver to insulin ( metformin);
- thiazolidinediones (glitazones), similar in properties to biguanides ( pioglitazone, rosiglitazone);
- alpha-glucosidase inhibitors that reduce the rate of glucose absorption in the gastrointestinal tract ( acarbose);
- agonists of glucagon-like peptide-1 receptors, stimulating the synthesis and secretion of insulin, reducing glucose production by the liver, appetite and body weight, slowing down the evacuation of the food bolus from the stomach ( exenatide, liraglutide);
- inhibitors of depeptidyl-peptidase-4, which also stimulate the synthesis and secretion of insulin, reduce the production of glucose by the liver, do not affect the rate of evacuation of food from the stomach and have a neutral effect on body weight ( sitagliptin, vildagliptin);
- inhibitors of sodium-glucose cotransporter type 2 (gliflozins), which reduce the reabsorption (absorption) of glucose in the kidneys, as well as body weight ( dapagliflozin,empagliflozin).
insulin therapy
Depending on the severity of the disease and the complications that arise, the doctor prescribes insulin. This method of treatment is indicated in approximately 15-20% of cases. Indications for the use of insulin therapy are:
- rapid weight loss for no apparent reason;
- the occurrence of complications;
- insufficient effectiveness of other hypoglycemic drugs.
Surgery
Despite the many hypoglycemic drugs, the issue of their correct dosage, as well as the adherence of patients to the chosen method of therapy, remains unresolved. This, in turn, creates difficulties in achieving long-term remission of type II diabetes. Therefore, surgical therapy of this disease - bariatric or metabolic surgery - is gaining more and more popularity in the world. IJF believes this method treatment of patients with type II diabetes effective. Currently, more than 500,000 bariatric surgeries are performed worldwide every year. There are several types of metabolic surgery, the most common being gastric bypass and mini gastric bypass.

During the bypass, the stomach is cut below the esophagus so that its volume is reduced to 30 ml. Remaining most of the stomach is not removed, but choked, preventing food from entering it. As a result of the intersection, a small stomach is formed, to which the small intestine is then sewn, retreating 1 m from its end. Thus, the food will directly enter the large intestine, while processing it with digestive juices will decrease. This, in turn, provokes irritation of the L-cells of the ileum, which contributes to a decrease in appetite and an increase in the growth of cells that synthesize insulin.

The main difference between mini gastric bypass and classical gastric bypass is the reduction in the number of anastomoses (connections of intestinal segments). When performing a traditional operation, two anastomoses are superimposed: the connection of the stomach and small intestine and the connection of different parts of the small intestine. With minigastric bypass, there is only one anastomosis - between the stomach and the small intestine. Due to the small volume of the newly formed stomach and the rapid entry of food into small intestine the patient has a feeling of fullness even after taking small portions of food.
Other types of bariatric surgery include:

- sleeve gastroplasty (otherwise it is called laparoscopic longitudinal resection of the stomach) - cutting off most of the stomach and forming a gastric tube with a volume of 30 ml, which contributes to rapid saturation, and also avoids following a strict diet;

- gastric banding - a reduction in the volume of the stomach with the help of a special ring (bandage) superimposed on the upper part of the stomach (this intervention is reversible).

Contraindications for surgical treatment- the patient has esophagitis (inflammation of the esophageal mucosa), esophageal varicose veins, portal hypertension, liver cirrhosis, peptic ulcer stomach or duodenum, chronic pancreatitis, pregnancy, alcoholism, severe diseases of the cardiovascular system or mental disorders, as well as long-term use of hormonal drugs.
Forecast. Prevention
Unfortunately, there is no cure for type II diabetes. However, there are ways to improve the quality of life of patients with this disease.
Today, there are a large number of “bases” where endocrinologists explain to patients what their lifestyle should be like, how to eat right, what foods should not be consumed, what should be daily physical activity.
A huge number of hypoglycemic drugs have also been created, which are improved every year. In order for them to have a positive effect on the body, medicines must be taken regularly.
Practice shows that compliance with all the recommendations of endocrinologists improves the treatment of type II diabetes.
Bariatric surgery is an operative method that improves the quality of life in type II diabetes, according to the MFD.
Significantly improve the condition of patients with this disease allows gastrointestinal operations (therapy), as a result of which the level of glycohemoglobin and glucose in the blood is normalized, the need for the use of antidiabetic drugs and insulin is lost.
Bariatric surgery can lead to significant and sustained remission as well as improvement in type II diabetes and other metabolic risk factors in obese patients. Surgery within 5 years of diagnosis most often leads to long-term remission.
To prevent the occurrence of type II diabetes, the following preventive measures must be observed:
- Diet- in case of excess body weight, it is necessary to monitor what is included in the diet: it is very useful to eat vegetables and fruits with a low glucose content, while limiting the use of foods such as bread, flour products, potatoes, fatty, spicy, smoked and sweet dishes.
- Strong physical activity- Exhausting workouts are not necessary. The best option would be daily walking or swimming in the pool. Light exercise, if done at least five times a week, reduces the risk of type II diabetes by 50%.
- Normalization of the psycho-emotional state is an integral method of preventing this disease. It is important to remember that stress can cause metabolic disorders leading to obesity and the development of diabetes. Therefore, it is necessary to strengthen stress resistance.
Type 2 diabetes is an insulin-dependent disease in which tissues become insensitive to the hormone insulin. A prerequisite for the development of the disease is the accumulation of lipids on the surface of cell receptors. This condition results in the inability to absorb glucose.
This pathological process causes increased production of insulin in the pancreas. If type 1 diabetes does not involve the introduction of a hormone, then in this situation it is simply impossible to do without it.
The World Health Organization insists that this disease is equally diagnosed in all countries of the world. Until recently, diabetes was considered a problem for the elderly, but today the picture has changed radically.
According to medical statistics, diabetes is the third leading cause of death. This disease has lost the palm only to oncology and cardiovascular diseases. In many countries, disease control occurs at the state level.
Features of type 2 diabetes
This type of diabetes refers to those health problems that remain with a person for life. Modern science has not yet learned how to effectively get rid of this dangerous pathology. In addition, there is a fairly high probability of microangiopathy, which provokes problems with vision, as well as with the kidneys of a sick person.
If you systematically and efficiently control blood sugar, then it is possible to take control of various aggressive changes in the vessels:
- fragility;
- excessive permeability;
- thrombus formation.
With proper therapy, ischemic changes, as well as cerebrovascular diseases, can be reduced several times.
The main goal of therapy is to compensate for the imbalance of carbohydrate metabolism, not only in the presence of problems with glucose, but also with secondary reactions from metabolism.
Over time, such changes become a prerequisite for a progressive decrease in the mass of beta cells that are produced by the pancreas.
Hypoglycemia is an extremely dangerous condition in the elderly diabetic. If, with the first type of disease, restoring the imbalance in insulin production will lead to prolonged control of sugar levels, then with the second type of pathology, therapy will be quite complicated and lengthy.
Medical therapy
In cases where monotherapy in the form of following the strictest diet does not give the expected result, it is necessary to connect special medical preparations that lower blood glucose levels. Some of the most modern medications that only a doctor can prescribe may not preclude carbohydrate intake. This makes it possible to minimize hypoglycemic conditions.
The choice of drug will be made taking into account all the individual characteristics of the patient, as well as his history. Self-selection of drugs based on the recommendations of other diabetic patients is an extreme degree of irresponsibility!
This can cause significant damage to the health of the patient or even cause death from diabetes.
Means that are used for treatment are contraindicated during pregnancy and lactation.
There are several generations of oral drugs for diabetes:
1st generation:
- Tolbutamide (butamide). Take 500-3000 mg / day for 2-3 doses;
- Tolazamide (tolinase). 100-1000 mg / day for 1-2 doses;
- Chlorpropamide. 100-500 mg / day once.
II generation:
- Nateglinide (glibenclamide). Take 1.25-20 mg / essence. It can be 1-2 doses;
- Glipizide. 2.5-40 mg / day for 1-2 doses.
There are equally effective alternative drugs for the treatment of type 2 diabetes:
- Metformin. Take 500-850 mg / day (2-3 doses). This drug may be given to increase levels of effectiveness or to overcome insulin resistance. It is contraindicated with a high probability of developing lactic acidosis, renal failure. In addition, Metformin should not be used after radiopaque agents, operations, myocardial infarction, inflammation of the pancreas, alcoholism, heart problems, and also together with tetracyclines;
- Acarbose. 25-100 mg / day (3 doses). The drug is used at the very beginning of the meal. This makes it possible to prevent hyperglycemia developing after eating. The drug is contraindicated in renal failure, inflammatory processes in the intestines, ulcerative colitis and partial obstruction this organ.
International practice of getting rid of the second type of diabetes mellitus
There is good evidence that controlling blood sugar can help reduce the chance of complications from diabetes. To do this, a diabetes management strategy was created, which provides for 4 stages:
- diet food low in carbohydrates;
- physical activity according to the prescribed treatment regimens;
- medications;
- hormonal injections, but only when such a need arises.
 Compensation of carbohydrates must be made taking into account the degree of the course of the disease (chronicle, exacerbation, remission). The cycle of diabetes mellitus involves the use of medicines taking into account this process and possible daily circadian rhythms production of insulin.
Compensation of carbohydrates must be made taking into account the degree of the course of the disease (chronicle, exacerbation, remission). The cycle of diabetes mellitus involves the use of medicines taking into account this process and possible daily circadian rhythms production of insulin.
Thanks to a low-carbohydrate diet, it is possible to reduce sugar and bring it within the normal range. At the subsequent stages, regular monitoring of glycemia is carried out. If the drug is not sufficient to adequately maintain glucose, then special exercise therapy for diabetes mellitus may be recommended. It will help to remove excess carbohydrates from the body, and will act as a kind of treatment.
In some situations, only the first levels of diabetes control may be prescribed. in the form of tablets can be shown only under the condition of an uncontrolled course of the disease, as well as an increase in glycemia. In some cases, additional injections of insulin may be made. This is necessary to bring glucose to normal levels.
Dietary nutrition for type 2 diabetes
The treatment of this pathology should begin with an adequate diet, which is always based on the following principles:
- fractional meals at least 6 times a day. It is very good to eat every day at the same time;
- caloric content cannot exceed 1800 kcal;
- normalization of excess weight in a patient;
- limiting the amount of saturated fat consumed;
- reduced salt intake;
- minimizing alcoholic beverages;
- eating food with a high percentage of trace elements and vitamins.
If there is a deterioration in fat metabolism against the background of developed glycemia, then this becomes a prerequisite for the occurrence of blood clots in the vessels. The fibrinolytic activity of human blood and the degree of its viscosity can affect the level of platelets, as well as fibrinogen - those factors that are responsible for blood clotting.
Carbohydrates cannot be completely eliminated from the diet, because they are extremely important for saturating the cells of the body with energy. If there is a lack of it, then the strength and frequency of contractions in the heart and vascular smooth muscles may be impaired.
Physiotherapy
Against the background of type 2 diabetes, various physical activities can be successfully applied, which help to better cope with the disease, this is also a kind of treatment that goes together. It can be:
- swimming;
- walks;
- a ride on the bicycle.
Therapeutic exercises give positive result, lowering blood sugar levels, however, this effect is short-lived. The duration and the very nature of the load should be selected strictly individually for each diabetic.
Physical education sets you in a good emotional mood and makes it possible to better cope with stressful situations. It also increases the level of endorphins - those hormones that are responsible for pleasure, and also helps to increase the concentration of testosterone (the main male hormone).
How is the treatment?
It has been established by medicine that glycosylated hemoglobin becomes a control marker of type 2 diabetes mellitus. The reference point is considered to be the concentration of this important substance, which will be equal to 7 percent.
If this figure drops to 6 percent, then in this case it becomes a signal to start getting rid of the disease. In some situations, this concentration may be considered normal.
At the onset of diabetes mellitus, it is possible to normalize the patient's condition with the help of dietary nutrition and physiotherapy exercises. Serious weight loss makes it possible to keep glycemia under control. If this is not enough, then the connection of drugs is necessary.
Experts recommend for initial stages use metformin for treatment. This tool helps to more accurately control blood glucose. If there are no significant contraindications, then the following drugs can be connected:
- biguanides. These remedies for diabetes have an impressive history. In view of the likelihood of developing acidosis against the background of existing blood lactic acid and high glucose levels, the use of biguanides for another 20 years made it possible for patients to keep their blood sugar at an acceptable level. Over time, buformin and phenformin with their derivatives were excluded from the therapy regimen;
- sulfonylurea preparations. This group of drugs is responsible for the production of insulin in the pancreas. Such a substance is extremely important for improving the absorption of glucose. Treatment of the second type of disease with the help of sulfonylureas should be started with small doses. If the patient has increased glucose toxicity, then each time the volume of the administered substance should be produced under glucose control;
- glitazones (thiazolidinediones). These drugs are a class of oral hypoglycemic agents. They help to increase the susceptibility of cells. The whole mechanism of action is that the manifestation of multiple genes that are responsible for controlling the process of processing sugar and fatty acids increases;
- glinides (prandial regulators). These drugs lower blood sugar. Their action lies in stopping ATP-sensitive channels. This group of drugs includes nateglinide, as well as repaglinide;
- alpha-glucosidase inhibitors can compete with carbohydrates. They carry out a bunch of intestinal enzymes and take part in the breakdown of glucose. In domestic medical practice, they use medicine acarbose.
In people with type 2 diabetes, it is important to control blood sugar levels and this is where any therapy begins. For this, each of the patients must have their own glucometer, without which the treatment is complicated. It is extremely important to control the concentration of glucose in the presence of heart disease, which is combined with a too rapid frequency of its reduction and high blood pressure.
How is impaired glucose uptake treated?
Treatment aimed at eliminating glucose malabsorption should be effective. All pathophysiological aspects of this disease make it possible to maintain target levels of glycemia.
A medical study that was aimed at testing the effectiveness of insulin therapy in patients with type 2 diabetes showed that at high concentrations of sugar it is not always possible to normalize it with the help of oral preparations.
When deciding on methods of therapy, it is important to understand that you will have to get rid of the disease for quite a long time. If we talk about combination therapy, then it can be carried out throughout the entire period of life of such a patient.
Studies have shown that diabetes only gets worse over time. An exacerbation of pathologies begins, which involve treatment with other means than those indicated above.
Type 2 diabetes varies from person to person. If one patient, even after 10 years, does not experience damage to the walls of blood vessels, then another can begin quite quickly.
If the disease is constantly progressing, then this should not be left without attention and control of glycosylated hemoglobin. If there is even an insignificant decrease in it, then in this case, symptomatic drugs or insulin therapy should be prescribed.
First of all, it is important to note that diabetes mellitus of the second degree progresses extremely slowly, so a typical patient cannot always recognize the predominance of pathology in his own body. The first signs of violations endocrine system are weakly expressed, so many simply ignore them. In the meantime, the disease continues to prevail, moreover, the pathological process is slowly but surely progressing, giving diabetes the status of a chronic disease.
The first symptoms, due to which doubts and suspicions creep in, are an irresistible feeling of thirst, frequent urination and dry mucous membranes. The patient often goes to relieve himself, and this also happens during a night's sleep, so very often disorientation in space progresses, and there is a disturbance in the work of the central nervous system.
In addition, there are complaints of severe itching and weight gain. In the latter case, all diets are useless, and the patient is rapidly gaining weight, and after a couple of months they learn from the doctor that he suffers from one of the forms of obesity. This is not surprising, since the affected body is dominated by increased appetite due to the high concentration of insulin in the blood.
In more advanced clinical pictures, a slightly different symptomatology prevails, which already poses a threat to the patient's life. This is a hyperosmolar coma, angiopathy or neuropathy, where each condition entails the most irreversible health consequences. So, hyperosmolar coma provokes an increase in glucose concentration, resulting in complete or partial dehydration of the body. In this clinical picture, immediate hospitalization is required, otherwise the life of the victim may not be saved.

Angiopathy is accompanied by fragility of blood vessels, as a result of which not only the general blood flow is disturbed, but also serious diseases of the cardiovascular system progress. Moreover, in the case of type II diabetes mellitus, large-scale damage to the walls of large vessels first occurs, and microangiopathy progresses. But the diabetic foot is one of the most serious complications of a characteristic ailment.
Among the additional symptoms that become a problem in the life of the patient, the following can be distinguished:
- progression of chronic pyelonephritis and cystitis;
- a rapid drop in visual acuity;
- a serious violation of the biochemistry of fluids, in particular clouding of the lens;
- reduced resistance to all viruses and pathogenic infections;
- Prolonged course of infectious diseases;
- Weakened immunity.
In any case, the most irreversible processes take place in the human body that turn the patient into an invalid and force him to live on pills. That is why early diagnosis and prompt treatment of type 2 diabetes is so important.
The main goals of treating diabetes mellitus of any type include maintaining a normal lifestyle; normalization of the metabolism of carbohydrates, proteins and fats; prevention of hypoglycemic reactions; prevention of late complications (consequences) of diabetes; psychological adjustment to life chronic disease. These goals can only be partially achieved in diabetic patients, due to the imperfection of modern replacement therapy. At the same time, today it is firmly established that the closer the patient's glycemia is to the normal level, the less likely it is to develop late complications of diabetes.
Despite numerous publications on the treatment of type 2 diabetes mellitus, the vast majority of patients do not achieve compensation for carbohydrate metabolism, although their general health may remain good. Not always a diabetic is aware of the importance of self-control and the study of glycemia is carried out from case to case. The illusion of relative well-being, based on normal well-being, delays the initiation of drug treatment in many patients with type 2 diabetes mellitus. In addition, the presence of morning normoglycemia does not exclude the decompensation of diabetes mellitus in such patients.
The key to successful treatment of patients with type 2 diabetes is education in a diabetic school. Teaching patients how to treat and manage their diabetes at home is extremely important.
Diet to treat type 2 diabetes
90% of people with type 2 diabetes have some degree of obesity, so weight loss through a low-calorie diet and exercise is of paramount importance. It is necessary to motivate the patient to lose weight, since even a moderate weight loss (by 5-10% of the original) can achieve a significant reduction in glycemia, blood lipids and blood pressure. In some cases, the condition of patients improves so much that there is no need for hypoglycemic agents.
Treatment usually begins with the selection of a diet and, if possible, expand the amount of physical activity. Diet therapy is the basis for the treatment of type 2 diabetes mellitus. Diet therapy consists in prescribing a balanced diet containing 50% carbohydrates, 20% proteins and 30% fats and following regular 5–6 meals a day - table number 9. Strict adherence to diet number 8 with fasting days for obesity and increased physical activity can significantly reduce the need in hypoglycemic drugs.
Physical exercise reduces insulin resistance, reduces hyperinsulinemia and improves carbohydrate tolerance. In addition, the lipid profile becomes less atherogenic - plasma total cholesterol and triglycerides decrease and lipoprotein cholesterol increases. high density.
A low-calorie diet can be balanced or unbalanced. With a balanced low-calorie diet, the total calorie content of food is reduced without changing its qualitative composition, in contrast to an unbalanced diet low in carbohydrates and fats. In the diet of patients should be foods with high content fiber (cereals, vegetables, fruits, wholemeal bread). The diet is recommended to include fibrous fiber, pectin or guar-guar in the amount of 15 g / day. If it is difficult to restrict dietary fat, you should take orlistat, which prevents the breakdown and absorption of 30% of the fat taken and, according to some reports, reduces insulin resistance. The result of monotherapy with a diet can be expected only with a decrease in weight by 10% or more from the original. This can be achieved by increasing physical activity along with a low-calorie balanced diet.
Of the sweeteners today, aspartame (a chemical compound of aspartic and phenylalanine amino acids), sucrasite, sladeks, saccharin are widely used. Acarbose, an antagonist of amylase and sucrase, which reduces the absorption of complex carbohydrates, can be included in the diet of a diabetic patient.
Exercise for the treatment of type 2 diabetes
Daily exercise is essential for type 2 diabetes. This increases the uptake of glucose by muscles, the sensitivity of peripheral tissues to insulin, improves the blood supply to organs and tissues, which leads to a decrease in hypoxia, an inevitable companion of poorly compensated diabetes at any age, especially the elderly. The amount of exercise in the elderly, hypertensive patients and those with a history of myocardial infarction should be determined by the doctor. If there are no other prescriptions, you can limit yourself to a daily 30-minute walk (3 times for 10 minutes).
With decompensation of diabetes mellitus, physical exercises are ineffective. With heavy physical exertion, hypoglycemia may develop, so the doses of hypoglycemic drugs (and especially insulin) should be reduced by 20%.
If diet and exercise fail to achieve normoglycemia, if this treatment does not normalize the disturbed metabolism, one should resort to drug treatment of type 2 diabetes mellitus. In this case, tableted hypoglycemic agents, sulfonamides or biguanides are prescribed, and if they are ineffective, a combination of sulfonamides with biguanides or hypoglycemic drugs with insulin. New groups of drugs - secretagogues (NovoNorm, Starlix) and insulin sensitizers that reduce insulin resistance (thiazolidinedione derivatives - pioglitazone, Aktos). With complete depletion of residual insulin secretion, they switch to insulin monotherapy.
Medical treatment of type 2 diabetes
More than 60% of patients with type 2 diabetes are treated with oral hypoglycemic drugs. For more than 40 years, sulfonylurea has been the mainstay of oral hypoglycemic therapy for type 2 diabetes mellitus. The main mechanism of action of sulfonylurea drugs is to stimulate the secretion of their own insulin.
Any sulfonylurea preparation, after oral administration, binds to a specific protein on the pancreatic β-cell membrane and stimulates insulin secretion. In addition, some sulfonylurea drugs restore (increase) the sensitivity of β-cells to glucose.
Sulfonylureas are attributed to the action, which consists in increasing the sensitivity of cells of adipose, muscle, liver and some other tissues to the action of insulin, in increasing the transport of glucose in skeletal muscles. For patients with type 2 diabetes mellitus with well-preserved function of insulin secretion, the combination of a sulfonylurea drug with biguanide is effective.
Sulfonamides (sulfonylurea drugs) are derivatives of the urea molecule, in which the nitrogen atom is replaced by various chemical groups, which determines the pharmacokinetic and pharmacodynamic differences of these drugs. But they all stimulate the secretion of insulin.
Sulfonamide preparations are rapidly absorbed, even when taken with food, and therefore can be taken with food.
Suphanilamides for the treatment of type 2 diabetes mellitus
Let's give brief description the most common sulfonamides.
Tolbutamide (Butamid, Orabet), tablets of 0.25 and 0.5 g - the least active among sulfonamides, has the shortest duration of action (6-10 hours), and therefore can be administered 2-3 times a day. Although this is one of the first sulfonylurea drugs, it is still used today, because it has little side effects.
Chlorpropamide (Diabenez), tablets of 0.1 and 0.25 g - has the longest duration of action (more than 24 hours), is taken 1 time per day, in the morning. Causes many side effects, the most serious is long-term and difficult to eliminate hypoglycemia. Severe hyponatremia and antabuse-like reactions were also observed. Currently, chlorpropamide is rarely used.
Glibenclamide (Maninil, Betanaz, Daonil, Euglucon), 5 mg tablets is one of the most commonly used sulfonamides in Europe. It is prescribed, as a rule, 2 times a day, in the morning and in the evening. The modern pharmaceutical form is micronized maninil at 1.75 and 3.5 mg, it is better tolerated and more powerful.
Glipizide (Diabenez, Minidiab), tablets of 5 mg / tab. Like glibenclamide, this drug is 100 times more active than tolbutamide, the duration of action reaches 10 hours, it is usually prescribed 2 times a day.
Gliclazide (Diabeton, Predian, Glidiab, Glizid), tablets of 80 mg - its pharmacokinetic parameters are somewhere between the parameters of glibenclamide and glipizide. Usually given twice a day, modified-release diabeton is now available and taken once a day.
Gliquidone (Glurenorm), tablets of 30 and 60 mg. The drug is completely metabolized by the liver to an inactive form, so it can be used in chronic renal failure. Practically does not cause severe hypoglycemia, therefore it is especially indicated for elderly patients.
Modern sulfonamides of the 3rd generation include glimepiride (Amaryl), tablets of 1, 2, 3, 4 mg. It has a powerful prolonged hypoglycemic effect, close to Maninil. It is used once a day, the maximum daily dose is 6 mg.
Side effects of sulfonamides
Severe hypoglycemia occurs infrequently with sulfonamides, mainly in patients receiving chlorpropamide or glibenclamide. The risk of developing hypoglycemia is especially high in elderly patients with chronic kidney failure or against the background of an acute intercurrent illness, when food intake is reduced. In the elderly, hypoglycemia is manifested mainly by mental or neurological symptoms making it difficult to recognize. In this regard, it is not recommended to prescribe long-acting sulfonamides to the elderly.
Very rarely, in the first weeks of treatment with sulfonamides, dyspepsia, skin hypersensitivity, or a reaction of the hematopoietic system develop.
Since alcohol inhibits gluconeogenesis in the liver, its intake can cause hypoglycemia in a patient receiving sulfonamides.
Reserpine, clonidine and non-selective β-blockers also contribute to the development of hypoglycemia by suppressing counter-insulin regulatory mechanisms in the body and, in addition, can mask early symptoms hypoglycemia.
Diuretics, glucocorticoids, sympathomimetics and nicotinic acid reduce the effect of sulfonamides.
Biguanides (metformin) for the treatment of type 2 diabetes
Biguanides, derivatives of guanidine, enhance glucose uptake by skeletal muscles. Biguanides stimulate lactate production in muscles and/or organs abdominal cavity and therefore, many patients receiving biguanides have elevated lactate levels. However, lactic acidosis develops only in patients with reduced biguanide and lactate elimination or with increased lactate production, in particular, in patients with reduced kidney function (they are contraindicated with elevated serum creatinine), with liver disease, alcoholism and cardiopulmonary insufficiency. Lactic acidosis has been particularly common with phenformin and buformin, which is why they have been discontinued.
For today only metformin (Glucophage, Siofor, Diformin, Dianormet) used in clinical practice for the treatment of type 2 diabetes mellitus. Since metformin reduces appetite and does not stimulate hyperinsulinemia, its use is most justified in obese diabetes mellitus, making it easier for such patients to maintain a diet and promote weight loss. Metformin also improves lipid metabolism, reducing the level of low density lipoproteins.
Interest in metformin has now increased dramatically. This is due to the peculiarities of the mechanism of action of this drug. We can say that basically Metformin increases the sensitivity of tissues to insulin, suppresses the production of glucose by the liver and, of course, reduces fasting glycemia, slows down the absorption of glucose in the gastrointestinal tract. There are additional effects of this drug that have a positive effect on fat metabolism, blood clotting and blood pressure.
The half-life of metformin, which is completely absorbed in the intestine and metabolized in the liver, is 1.5-3 hours, and therefore it is prescribed 2-3 times a day during or after meals. Treatment is started with minimal doses (0.25–0.5 g in the morning) to prevent adverse reactions in the form of dyspeptic phenomena, which occur in 10% of patients, but in most patients they pass quickly. In the future, if necessary, the dose can be increased to 0.5–0.75 g per dose, prescribing the drug 3 times a day. Maintenance dose - 0.25-0.5 g 3 times a day.
Treatment with biguanides should be immediately discontinued when the patient develops acute kidney disease, liver disease, or manifests cardiopulmonary insufficiency.
Since sulfonamides mainly stimulate insulin secretion, and metformin mainly improves its action, they can complement each other's hypoglycemic effect. The combination of these drugs does not increase the risk of side effects, is not accompanied by their adverse interactions, and therefore they are successfully combined in the treatment of type 2 diabetes mellitus.
Combinations of drugs in the treatment of type 2 diabetes
The expediency of using sulfonylurea drugs is beyond doubt, because the most important link in the pathogenesis of type 2 diabetes is a secretory defect in the β-cell. On the other hand, insulin resistance is an almost constant feature of type 2 diabetes mellitus, which necessitates the use of metformin.
Metformin in combination with sulfonylurea drugs- a component of effective treatment, has been intensively used for many years and allows to achieve a reduction in the dose of sulfonylurea drugs. According to the researchers, combination therapy with metformin and sulfonylurea drugs is as effective as combination therapy with insulin and sulfonylurea drugs.
Confirmation of observations that combination therapy with sulfonylurea and metformin has significant advantages over monotherapy contributed to the creation of the official form of the drug containing both components (Glibomet).
To achieve the main goals of the treatment of diabetes mellitus, it is necessary to change the previously established stereotype of treatment of patients and switch to more aggressive therapy tactics: the early start of combined treatment with oral hypoglycemic drugs, in some patients almost from the moment of diagnosis.
Simplicity, efficiency and relative cheapness explain the fact that secretogens successfully complement metformin. Combined drug Glucovans, containing metformin and a micronized form of glibenclamide in one tablet, is the most promising representative new form antidiabetic drugs. It turned out that the creation of Glucovans clearly improves not only patient compliance, but also reduces total number and intensity of side effects with the same or better efficacy.
Advantages of Glucovans over Glibomet (metformin 400 mg + glibenclamide 2.5 mg): Metformin forms a soluble matrix in which micronized glibenclamide particles are evenly distributed. This allows glibenclamide to act faster than the non-micronized form. The rapid achievement of the peak concentration of glibenclamide allows you to take Glucovans with meals, which, in turn, reduces the frequency of gastrointestinal effects that occur when taking Glibomet. The undoubted advantage of Glucovans is the presence of 2 dosages (metformin 500 + glibenclamide 2.5, metformin 500 + glibenclamide 5), which allows you to quickly select an effective treatment.
Addition of basal insulin (Monotard HM type) at an average dose of 0.2 U per 1 kg of body weight to ongoing combination therapy, it is recommended to start as a single injection at night (22.00), usually the dose is increased by 2 U every 3 days until target glycemic values of 3.9–7.2 mmol are reached / l. In the case of a high initial level of glycemia, it is possible to increase the dose by 4 IU every 3 days.
Secondary resistance to sulfa drugs.
Despite the fact that tissue insulin resistance is the leading mechanism for the development of type 2 diabetes mellitus, insulin secretion in these patients also decreases over the years, and therefore the effectiveness of sulfonamide treatment decreases over time: in 5–10% of patients annually and in most patients after 12 -15 years of therapy. This loss of sensitivity is called secondary resistance to sulfonamides, as opposed to primary, when they are ineffective from the very beginning of treatment.
Resistance to sulfonamides is manifested by progressive weight loss, the development of fasting hyperglycemia, postalimentary hyperglycemia, an increase in glycosuria, and an increase in HbA1c levels.
With secondary resistance to sulfonamides, a combination of insulin (IPD) and sulfonamides is first prescribed. The likelihood of a positive effect of combination therapy is high when it is prescribed at the earliest stages of the development of secondary resistance, i.e. at a fasting glycemia level between 7.5–9 mmol/l.
It is possible to use pioglitazone (Aktos) - a drug that reduces insulin resistance, which makes it possible to reduce the dose of IPD and, in some cases, cancel it. Take actos 30 mg 1 time per day. It can be combined with both metformin and sulfonylurea preparations.
But the most common combination treatment regimen is that the previously prescribed sulfonamide treatment is supplemented with small doses (8-10 IU) of medium-acting drugs (for example, NPH or ready-made "mixes" - mixtures of short-acting and prolonged-acting drugs) 1-2 times a day. day (8.00, 21.00). The dose is increased in steps of 2-4 units every 2-4 days. In this case, the dose of sulfanilamide should be maximum.
Such treatment can be combined with a low-calorie diet (1000-1200 kcal / day) for diabetes in obese people.
If the regimen of a single injection of insulin is ineffective, it is administered 2 times a day, with glycemic control at critical points: on an empty stomach and at 17.00.
The usual dose of IPD is 10–20 IU/day. When the need for insulin is higher, this indicates complete resistance to sulfonamides, and then insulin monotherapy is prescribed, i.e. sulfonamide preparations are completely canceled.
The arsenal of hypoglycemic drugs used in the treatment of type 2 diabetes mellitus is quite large and continues to grow. In addition to sulfonylurea derivatives and biguanides, this includes secretogens, amino acid derivatives, insulin sensitizers (thiazolidinediones), α-glucosidase inhibitors (glucobay), and insulins.
Glycemic regulators for the treatment of type 2 diabetes
Based on the important role of amino acids in the process of insulin secretion by β-cells directly in the process of eating, scientists studied the hypoglycemic activity of phenylalanine analogs, benzoic acid, synthesized nateglinide and repaglinide (NovoNorm).
Novonorm is an oral fast-acting hypoglycemic drug. Rapidly lowers blood glucose levels by stimulating the release of insulin from functioning pancreatic β-cells. The mechanism of action is associated with the ability of the drug to close ATP-dependent channels in the membranes of β-cells by acting on specific receptors, which leads to cell depolarization and the opening of calcium channels. As a result, increased calcium influx induces insulin secretion by β-cells.
After taking the drug, an insulinotropic response to food intake is observed within 30 minutes, which leads to a decrease in blood glucose levels. In the periods between meals, there is no increase in insulin concentration. In patients with non-insulin dependent type 2 diabetes mellitus, when taking the drug in doses of 0.5 to 4 mg, a dose-dependent decrease in blood glucose levels is noted.
Insulin secretion stimulated by nateglinide and repaglinide is close to the physiological early phase of hormone secretion in healthy individuals after a meal, resulting in effective reduction peaks of glucose concentration in the postprandial period. They have a quick and short-term effect on insulin secretion, thereby preventing a sharp increase in glycemia after a meal. When skipping meals, these drugs are not used.
Nateglinide (Starlix) is a derivative of phenylalanine. The drug restores early insulin secretion, which leads to a decrease in postprandial blood glucose concentration and the level of glycosylated hemoglobin (HbA1c).
Under the influence of nateglinide taken before meals, the early (or first) phase of insulin secretion is restored. The mechanism of this phenomenon lies in the rapid and reversible interaction of the drug with K + ATP-dependent channels of pancreatic β-cells.
The selectivity of nateglinide for K + ATP-dependent channels of pancreatic β-cells is 300 times higher than that for the channels of the heart and blood vessels.
Nateglinide, unlike other oral hypoglycemic agents, causes a pronounced secretion of insulin within the first 15 minutes after a meal, thereby smoothing out postprandial fluctuations (“peaks”) in blood glucose concentration. In the next 3–4 hours, the insulin level returns to its original values. Thus, postprandial hyperinsulinemia, which can lead to delayed hypoglycemia, is avoided.
Starlix should be taken before meals. The time interval between taking the drug and eating should not exceed 30 minutes. When using Starlix as monotherapy, the recommended dose is 120 mg 3 times / day (before breakfast, lunch and dinner). If with this dosing regimen it is not possible to achieve the desired effect, a single dose can be increased to 180 mg.
Another prandial regulator of glycemia is acarbose (glucobay). Its action takes place in the upper part of the small intestine, where it reversibly blocks α-glucosidases (glucoamylase, sucrase, maltase) and prevents the enzymatic breakdown of poly- and oligosaccharides. This prevents the absorption of monosaccharides (glucose) and reduces the sharp rise in blood sugar after eating.
Inhibition of α-glucosidase by acarbose occurs according to the principle of competition for the active site of the enzyme located on the surface of the microvilli of the small intestine. Preventing the rise in glycemia after a meal, acarbose significantly reduces the level of insulin in the blood, which improves the quality of metabolic compensation. This is confirmed by a decrease in the level of glycated hemoglobin (HbA1c).
The use of acarbose as the sole oral antidiabetic agent is sufficient to significantly reduce metabolic disturbances in patients with type 2 diabetes mellitus that are not compensated by diet alone. In cases where such tactics do not lead to the desired results, the appointment of acarbose with sulfonylurea drugs (Glurenorm) leads to a significant improvement in metabolic parameters. This is especially important for elderly patients who are not always ready to switch to insulin therapy.
In patients with type 2 diabetes mellitus who received insulin therapy and acarbose, the daily insulin dose decreased by an average of 10 units, while in patients who received placebo, the insulin dose increased by 0.7 units.
The use of acarbose significantly reduces the dose of sulfonylureas. The advantage of acarbose is that it does not cause hypoglycemia when used alone.
Modern conditions dictate the need to create new drugs that allow not only to eliminate metabolic disorders, but also to maintain the functional activity of pancreatic cells, stimulating and activating the physiological mechanisms of regulation of insulin secretion and blood glucose. In recent years, it has been shown that the regulation of glucose levels in the body, in addition to insulin and glucagon, also involves the hormones incretins produced in the intestine in response to food intake. Up to 70% of postprandial insulin secretion in healthy individuals is due precisely to the effect of incretins.
Incretins in the treatment of type 2 diabetes mellitus
The main representatives of incretins are glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (G PP-1).
The intake of food in digestive tract quickly stimulates the release of GIP and GLP-1. Incretins can also lower glycemic levels through non-insulin mechanisms by slowing gastric emptying and reducing food intake. In type 2 diabetes, the content of incretins and their effect are reduced, and the level of glucose in the blood is increased.
The ability of GLP-1 to improve glycemic control is of interest in the treatment of type 2 diabetes mellitus (the emergence of a class of incretin mimetics). GLP-1 has multiple effects on the endocrine part of the pancreas, but its principal action is to potentiate glucose-dependent insulin secretion.
Increased levels of intracellular cAMP stimulate GLP-1 receptors (rGLP-1), resulting in exocytosis of insulin granules from β-cells. An increase in cAMP levels thus serves as the primary mediator of GLP-1 induced insulin secretion. GLP-1 enhances insulin gene transcription, insulin biosynthesis, and promotes β-cell proliferation through rGLP-1 activation. GLP-1 also potentiates glucose-dependent insulin secretion via intracellular pathways. In the study by C. Orskov et al. GLP-1 has been shown in vivo to cause a decrease in glucagon secretion when acting on α-cells.
Improvement in glycemic indices after administration of GLP-1 may be the result of the restoration of normal β-cell function. An in vitro study indicates that glucose-resistant β-cells become glucose-competent after administration of GLP-1.
The term "glucose competence" is used to describe the functional state of β-cells that are sensitive to glucose and secrete insulin. GLP-1 has an additional hypoglycemic effect that is not associated with an effect on the pancreas and stomach. In the liver, GLP-1 inhibits glucose production and promotes glucose uptake by adipose and muscle tissue, but these effects are secondary to regulation of insulin and glucagon secretion.
An increase in the mass of β-cells and a decrease in their apoptosis is a valuable quality of GLP-1 and is of particular interest for the treatment of type 2 diabetes mellitus, since the main pathophysiological mechanism of this disease is precisely the progressive β-cell dysfunction. Incretinomimetics used in the treatment of type 2 diabetes include 2 classes of drugs: GLP-1 agonists (exenatide, liraglutide) and inhibitors of dipeptidyl peptidase-4 (DPP-4), which destroys GLP-1 (sitagliptin, vildagliptin).
Exenatide (Byetta) isolated from the saliva of the giant lizard Gila monster. The amino acid sequence of exenatide is 50% identical to human GLP-1. When exenatide is administered subcutaneously, its peak plasma concentration occurs after 2-3 hours, and the half-life is 2-6 hours. This allows exenatide therapy in the form of 2 subcutaneous injections per day before breakfast and dinner. Created, but not yet registered in Russia, long-acting exenatide - Exenatide LAR, administered once a week.
Liraglutide is a new drug, an analogue of the human GLP-1, which is 97% similar in structure to the human one. Liraglutide maintains a stable concentration of GLP-1 for 24 hours when administered once a day.
DPP-4 inhibitors for the treatment of type 2 diabetes
GLP-1 preparations developed to date do not have oral forms and require mandatory subcutaneous injection. This drawback is deprived of drugs from the group of DPP-4 inhibitors. By suppressing the action of this enzyme, DPP-4 inhibitors increase the level and lifespan of endogenous GIP and GLP-1, enhancing their physiological insulinotropic action. The drugs are available in tablet form and are prescribed, as a rule, once a day, which significantly increases the adherence of patients to the therapy. DPP-4 is a membrane-binding serine protease from the group of prolyl oligopeptidases, the main substrate for which are short peptides such as GIP and GLP-1. The enzymatic activity of DPP-4 on incretins, especially GLP-1, suggests the possibility of using DPP-4 inhibitors in the treatment of patients with type 2 diabetes mellitus.
The peculiarity of this approach to treatment is to increase the duration of action of endogenous incretins (GLP-1), i.e., the mobilization of the body's own reserves to combat hyperglycemia.
DPP-4 inhibitors include sitagliptin (Januvia) and vildagliptin (Galvus) recommended by the FDA (USA) and the European Union for the treatment of type 2 diabetes mellitus, both as monotherapy and in combination with metformin or thiazolidinediones.
The combination of DPP-4 inhibitors and metformin seems to be the most promising, which makes it possible to influence all the main pathogenetic mechanisms of type 2 diabetes mellitus - insulin resistance, secretory response of β-cells and hyperproduction of glucose by the liver.
The drug GalvusMet was created (50 mg vildagliptin + metformin 500, 850 or 100 mg), which was registered in 2009.
Insulin therapy in type 2 diabetes mellitus.
Despite the definition of type 2 diabetes mellitus as "non-insulin dependent", a large number of patients with this type of diabetes eventually develop absolute insulin deficiency, requiring the administration of insulin (insulin-requiring diabetes mellitus).
Treatment with insulin as monotherapy is indicated primarily for primary resistance to sulfonamides, when treatment with a diet and sulfonamides does not lead to optimal glycemia for 4 weeks, as well as for secondary resistance to sulfonamides against the background of depletion of endogenous insulin reserves, when it is necessary to compensate the exchange dose of insulin prescribed in combination with sulfonamides is high (more than 20 IU / day). The principles of insulin treatment for insulin-requiring diabetes mellitus and type 1 diabetes mellitus are almost the same.
According to the American Diabetes Association, after 15 years, most type 2 diabetics require insulin. However, a direct indication for monoinsulin therapy in type 2 diabetes mellitus is a progressive decrease in insulin secretion by pancreatic β-cells. Experience shows that approximately 40% of patients with type 2 diabetes require insulin therapy, but in fact this percentage is much lower, often due to patient opposition. In the remaining 60% of patients who are not indicated for monoinsulin therapy, unfortunately, treatment with sulfonylurea drugs also does not lead to compensation for diabetes mellitus.
Even if during daylight hours it is possible to reduce glycemia, then almost everyone has morning hyperglycemia, which is caused by nighttime production of glucose by the liver. The use of insulin in this group of patients leads to an increase in body weight, which exacerbates insulin resistance and increases the need for exogenous insulin, in addition, the inconvenience caused to the patient by frequent dosing of insulin and several injections per day should be taken into account. An excess of insulin in the body also causes concern for endocrinologists, because it is associated with the development and progression of atherosclerosis, arterial hypertension.
According to WHO experts, insulin therapy for type 2 diabetes should be started neither too early nor too late. There are at least 2 ways to limit insulin doses in patients not compensated by sulfonylurea drugs: the combination of a sulfonylurea drug with long-acting insulin (especially at night) and the combination of a sulfonylurea drug with metformin.
Combination treatment with sulfonylurea and insulin has significant advantages and is based on complementary mechanisms of action. High blood glucose has a toxic effect on β-cells, in connection with which the secretion of insulin is reduced, and the administration of insulin by lowering glycemia can restore the response of the pancreas to sulfonylurea. Insulin suppresses the formation of glucose in the liver at night, which leads to a decrease in fasting glycemia, and sulfonylurea causes an increase in insulin secretion after meals, controlling the level of glycemia during the day.
A number of studies have compared between 2 groups of type 2 diabetics, of which 1 group received only insulin therapy, and the other - combination therapy with insulin at night with a sulfonylurea. It turned out that after 3 and 6 months, the indicators of glycemia, glycated hemoglobin significantly decreased in both groups, but the average daily dose of insulin in the group of patients receiving combined treatment was 14 IU, and in the group of monoinsulin therapy - 57 IU per day.
Average daily dose extended insulin at bedtime to suppress nocturnal glucose production by the liver is usually 0.16 U / kg / day. With this combination, there was an improvement in glycemia, a significant decrease in the daily dose of insulin and, accordingly, a decrease in insulinemia. Patients noted the convenience of such treatment and expressed a desire to more accurately comply with the prescribed regimen.
Monotherapy with insulin in type 2 diabetes mellitus, i.e., not combined with sulfonamides, is necessarily prescribed for severe metabolic decompensation that has developed during treatment with sulfonamides, as well as for the pain form of peripheral neuropathy, amyotrophy or diabetic foot, gangrene (ICD therapy only or "bolus-basal").
Each patient should strive to achieve a good compensation for diabetes from the first days of the disease, which is facilitated by their training in the “schools for the patient with diabetes”. And where such schools are not organized, patients should be provided with at least special educational materials and diabetic diaries. Self-management and effective treatment also involves providing all diabetic patients with portable means for rapid testing of glycemia, glucosuria and ketonuria at home, as well as glucagon ampoules to eliminate severe hypoglycemia (hypokit kit).
M.I.Balabolkin, V.M.Kreminskaya, E.M.Klebanova
Department of Endocrinology and Diabetology, FPPO MMA named after I.M. Sechenov, Moscow
Diabetes mellitus (DM) type 2 is a heterogeneous disease, the development of which is due to the presence of insulin resistance and impaired insulin secretion by pancreatic islet β-cells. It becomes clear that type 2 diabetes therapy cannot be as unified as it is in type 1 diabetes.
The goal of treatment for type 2 diabetes is to achieve compensation for diabetes over a long period of time, i.e. indicators of glucose in blood plasma, which are almost identical to those observed in a healthy person throughout the day. However, the qualitative and quantitative indicators of DM compensation have been repeatedly revised based on ongoing studies that establish the dependence of the development of late vascular complications diabetes from the state of carbohydrate metabolism. The dynamics of quantitative indicators of DM compensation is presented in Table. one.
At present, no one doubts that strict and long-term compensation of carbohydrate metabolism reduces the frequency of complications of DM. This is convincingly shown by the results of the DCCT (1993) and UKPDS (1998) studies. Maintaining glycemia close to normal over the follow-up period (about 10 years) made it possible to carry out primary prevention of retinopathy in patients with type 1 diabetes by 76%; secondary prevention of retinopathy - by 54%; prevention of neuropathy - by 60%; to achieve the disappearance of microalbuminuria - by 39% and albuminuria - by 54%. The same effects can be achieved in type 2 diabetes, since the mechanisms underlying the development of complications are probably the same. Thus, it was found that intensive hypoglycemic therapy reduces the risk of myocardial infarction by 16%. Therefore, as before, the main task of treating DM is to achieve its compensation for a long time, which is associated with great difficulties. This is mainly due to the fact that diabetes treatment is usually prescribed not from the moment of carbohydrate metabolism disorder, which is detected only by various exercise tests (glucose tolerance test, etc.), but only when pronounced clinical signs of diabetes appear, indicating in turn the development vascular and other changes in tissues and organs.
Table 2.
Compensation criteria for type 2 diabetes
|
Indicators |
low risk |
Risk of arterial damage |
Risk of microangiopathy |
|
Plasma of venous blood on an empty stomach / before meals |
|||
|
Glucose of capillary blood (self-monitoring) |
|||
|
On an empty stomach / before meals |
|||
|
Postprandial glucose (peak) |
|||
Table 3
Criteria for the state of lipid metabolism in patients with type 2 diabetes mellitus
Thus, an analysis of the clinical manifestations of DM, detected during its manifestation in adults, shows a high incidence of late vascular complications in them, the development of which occurs with a duration of carbohydrate metabolism disorders of 5-7 years. Our study of the frequency of vascular complications in type 2 diabetes shows that 44% of patients with newly diagnosed diabetes have one or two (retinopathy, nephropathy, macroangiopathy, etc.) vascular complications of diabetes.
The main role in the pathogenesis of vascular complications of DM belongs to hyperglycemia, and in type 2 DM, to impaired lipid metabolism. European Office of the International Federation of Diabetes and WHO European Office in 1998. proposed criteria for metabolic compensation in patients with type 2 diabetes, which are presented in Table. 2.
In type 2 diabetes, carbohydrate metabolism disorders are combined with pronounced changes lipid metabolism. In this regard, when considering the compensation of metabolic processes, one should also take into account indicators of the state of lipid metabolism, which to some extent correlate with the risk of developing vascular complications of diabetes (Table 3).
The adequacy of DM therapy remains the most pressing issue, since it has been established that hyperglycemia is the starting point of many pathogenetic mechanisms that contribute to the development of vascular complications.
Strict compensation for diabetes, i.e. maintaining a normal (or close to normal) concentration of glucose in the blood for a long time, it is possible to delay or delay the onset of late complications of diabetes.
Treatment of type 2 diabetes
Treatment of type 2 diabetes is complex, and its components are: diet; dosed exercise stress; patient education and self-management of diabetes; drug therapy (oral hypoglycemic drugs as monotherapy, combination therapy with oral drugs - drugs with different mechanisms of action, combination therapy of oral hypoglycemic drugs with insulin or the use of insulin alone); prevention and treatment of late complications of DM.
Diet with type 2 diabetes, it must meet the following requirements: a) be physiological in terms of the composition of products (about 60% of the total calorie content of food should be carbohydrates, 24% fats and 16% proteins); b) the energy value food should be subcaloric (daily calorie content is about 1600-1800 kcal); c) 4-5 meals a day; d) exclude easily digestible carbohydrates from the diet and replace them with sweeteners or sweeteners; e) food should contain a sufficient amount of fiber or fiber (at least 25-30 g per day); f) of the total amount of fats, about 40-50% should be fats of vegetable origin (1/3 of the total amount of fat should be saturated fats; 1/3 - semi-unsaturated and 1/3 - unsaturated fats).
Multiple (4-5-fold) food intake during the day allows you to more adequately modulate the relationship between the level of insulin and blood glucose, approaching those indicators that occur in a healthy person throughout the day.
Physical activity and physiotherapy exercises are an obligatory component of therapy for patients with type 2 diabetes. The amount of physical activity should be determined taking into account the age of the patient, the state of the cardiovascular system and the compensation of carbohydrate metabolism. They have a positive effect on the course of diabetes and contribute to the maintenance of stable compensation of carbohydrate metabolism with a noticeable decrease in excess body weight. Regular exercise, regardless of its volume, contributes to the normalization of lipid metabolism, improves microcirculation, activates fibrinolysis, normalizes the increased secretion of catecholamines in response to a stressful situation, which ultimately prevents the development of vascular complications (angiopathy). Stabilization and even regression of vascular complications of DM were noted in diabetic patients who regularly exercise.
task patient education Type 2 diabetes is their motivation to change the lifestyle and habits that accompanied the patient throughout life before the development of diabetes. This applies primarily to the diet (almost 50% of the daily calorie content of food falls on the afternoon or dinner), sleep and rest, to reduce physical inactivity due to regular physical activity, to quit smoking and taking excessive doses of alcohol, and to fulfill all those activities that are components of a healthy lifestyle. Self-control of diabetes and the achievement of its compensation will help delay the development of vascular complications of diabetes.
Medical therapy
Drug therapy for patients with type 2 diabetes includes: a) the use of various drugs that affect the reduction of carbohydrate absorption in the gastrointestinal tract (acarbose, etc.); b) biguanides (metformin); c) glitazones or insulin sensitizers (pioglitazone); d) the use of drugs that stimulate insulin secretion: sulfonylurea drugs of the second generation: glibenclamide, glipizide, gliclazide, gliquidone and sulfonylurea drugs of the third generation (glimepiride), as well as drugs derived from amino acids, repaglinide and nateglinide, which are regulators of postprandial hyperglycemia or secretion stimulants short acting insulin. In cases where it is not possible to achieve compensation for diabetes with the help of oral hypoglycemic drugs (in patients with type 2 diabetes with a pronounced defect in pancreatic islet b-cells), it is recommended to use combination therapy (oral hypoglycemic therapy + insulin therapy, more often with drugs of an average duration of action on night or 2 times a day).
Sulfonylureas represent the main group of drugs used to treat type 2 diabetes. These drugs are insulin secretogens, and their main hypoglycemic effect is associated with stimulation of the formation and release of insulin from the pancreatic islets. In recent years, the mechanism of action of sulfonylurea drugs on the stimulation of insulin secretion by pancreatic b-cells has been completely deciphered. These drugs bind to the corresponding receptors localized on the membranes of b-cells, change the activity of K-ATPase, promote the closure of potassium channels (KATP-dependent channels) and increase the ratio of ATP/ADP levels in the cytoplasm, which leads to membrane depolarization. This, in turn, promotes the opening of voltage-dependent Ca2+ channels, an increase in the level of cytosolic calcium, and stimulation of Ca2+-dependent exocytosis of secretory granules, which results in the release of the contents of the secretory granule into the intercellular fluid and blood. The last step in insulin secretion is under the control of calcium/calmodulin-dependent protein kinase II. Thus, the target of sulfonylurea drugs are ATP-sensitive potassium channels, which consist of a sulfonylurea receptor [protein with a molecular weight of 140-kDa (SUR)] and a specific protein - (KIR6.2).
However, all sulfonylurea derivatives of the 2nd generation have certain disadvantages of greater or lesser severity, which do not allow in all cases to achieve stable compensation for diabetes and normalization of carbohydrate metabolism both for a long time and throughout the day. The latter is due to the fact that the peak of action of any sulfonylurea drug and the increase in post-absorption hyperglycemia do not coincide in time. This leads, on the one hand, to an insufficient decrease in the level of glucose in the blood for a long time, and on the other hand, to the development of hypoglycemia of varying severity in the hours following a meal, especially in the case of its insufficient amount or skipping a meal. Episodes of hypoglycemia are more common in elderly patients as a result of a violation of the regimen for the use of hypoglycemic drugs due to memory impairment. For example, when taking glibenclamide 2-3 times, patients often forget if they took the drug in the morning. To compensate for the possible absence of the drug before breakfast, the patient takes a double dose before dinner, which leads to the development of hypoglycemia at night.
The study of the molecular mechanisms of action of sulfonylurea drugs made it possible to obtain data that shed light on the processes of interaction between various stimulators of insulin secretion and showed that insulin secretogens, despite the identical final effect, which is manifested in increased secretion and release of insulin from b-cells, carry out this action through involvement in corresponding process of various protein and signal molecules.
ATP-sensitive potassium channels are the primary structures interacting with various insulin secretogens. ATP-sensitive potassium channels are a complex that includes sulfonylurea receptor 1 [protein with a molecular weight of 140,000 (SUR1) and a specific protein, the so-called internal potassium channel cleaner or rectifying subunit KIR6.2. The gene encoding the SUR1 receptor is localized on chromosome 11p15.1 and belongs to the family of ATP-binding cassette proteins (ABC proteins), which has 17 transmembrane domains (TMD), in which there are two nucleotide-binding sites - NBF-1 and NBF-2, specifically complexed with Mg2+ ADP/ATP. ATP-sensitive channels are, as it were, two proteins, SUR1 and KIR6.2, which are co-expressed together. The KIR6.2 locus is located within the SUR1 gene; on the same 11p15.1 chromosome.
Thus, ATP-sensitive potassium channels are "assembled-constructed" from two different subunits: the sulfonylurea receptor, which belongs to the family of ATP-binding cassettes, and potassium channel subunits (KIR6x), forming a pore and a regulatory subunit. Three isoforms of the sulfonylurea receptor have been cloned: SUR1, a high-affinity receptor, and SUR2, SUR2B, low-affinity receptors. Structurally, potassium channels in different tissues are not the same in terms of their constituent subunits. Thus, in b-cells of pancreatic islets and glucose-sensitive neurons of the hypothalamus, they consist of SUR1/KIR6.2; in the heart muscle, from SUR2A/KIR6.2; and in vascular smooth muscle cells, from SUR2B/KIR6.1 (or KIR6.2). It was shown that the ability of various drugs (glibenclamide, glipizide, tolbutamide and meglitinide) to inhibit potassium channels (SUR1/KIR6.2 and SUR2B/KIR6.2) was 3-6 times higher than their affinity for complexing with these receptors. Closure of the potassium channel requires binding of one of the four sulfonylurea binding sites on the "channel complex", which is represented by the octometric structure (SUR/KIR6x)4.
The key to understanding the mechanism of action of various sulfonylurea drugs were studies in which it was shown that the latter are complexed with certain areas of TMD. Thus, glibenclamide is complexed with the site 1-5 TMD, and tolbutamide - with 12-17 TMD, which indicates a modular structural and functional organization of ATP-sensitive potassium channels. Glibenclamide, as a result of conformational changes, disrupts the interaction between NBF 1 and 2 SUR1 in the regions of TMD 12-17 and especially TMD 1-5. This in turn causes the TMD2KIR6.2 complex, which is in direct contact with TMD 1-5 SUR1, to move to induce a "potassium channel closed" state. This mechanism requires the aminoterminal end of KIR6.2 to be intact. Thus, the binding of a sulfonylurea to SUR1 definitely causes an implicit decrease in the required bond strength between SUR1 and KIR6.2, which is required to keep KIR6.2 at least partially open.
The opening and closing of ATP-sensitive potassium channels, and hence the initiation of insulin secretion and its inhibition, is provided by ATP complexing with various subunits of potassium channels. ATP binding to the carboxyterminal domain of KIR6.2 stabilizes the dissociation of SUR1 and KIR6.2 induced by glibenclamide and promotes the closure of potassium channels. Complexation of ATP with NBF-1 and Mg2+ ADP with NBF-2 on SUR1 causes the opening of potassium channels.
Despite the fact that glibenclamide and glimepiride have a stimulating effect on insulin secretion by closing ATP-sensitive potassium channels, the mechanism of this effect has certain differences. It has been found that glimepiride has 2.2-3 times higher association rate constants and 8-10 times higher dissociation rates than glibenclamide. These data indicate that the affinity of glimepiride for the sulfonylurea receptor is 2-3 times lower than that of glibenclamide. In addition, glibenclamide complexed with the 140 kDa receptor polypeptide, while glimepiride complexed with the same receptor polypeptide, but with a molecular weight of 65 kDa, designated SURX. Additional studies have shown that glibenclamide, in addition to the main complexing with the 140 kDa polypeptide, also specifically complexes with proteins with a molecular weight of 40 and 65 kDa, which made it possible to suggest that glibenclamide can also complex with the SURX protein, although the affinity for such complexing it is significantly lower than that of glimepiride. All of the above suggests that the target proteins of the sulfonylurea receptor for glibenclamide and glimepiride are different: for glibenclamide - SUR1, for glimepiride - SURX. Both proteins interact with each other and control, through KIR6.2, the opening and closing of potassium channels, and, consequently, the processes of insulin synthesis and release in the pancreatic b-cell.
Since the use of sulfonylurea drugs for the treatment of type 2 diabetes, discussions about the extra-pancreatic (peripheral) effect of sulfonylurea drugs have not stopped. In the laboratory led by G. Muller, research in this direction has been carried out for many years. Studying in vitro and in vivo the effect of glimepiride, glipizide, glibenclamide and gliclazide on the maximum decrease in blood glucose levels and the minimum increase in insulin secretion within 36 hours after taking these drugs, it was found that glimepiride at a dose of 90 μg / kg caused the maximum decrease in glucose in the blood with minimal secretion of insulin; glipizide at a dose of 180 μg/kg had the lowest hypoglycemic activity and caused the maximum increase in insulin secretion; glibenclamide at a dose of 90 μg/kg and gliclazide at a dose of 1.8 mg/kg occupied an intermediate position between the two extremes. The curves of the dynamics of the concentration of insulin and glucose in the blood when using these sulfonylurea drugs were almost identical. However, when determining the coefficient (average increase in plasma insulin to average decrease in blood glucose), these indicators were not the same (glimepiride - 0.03; gliclazide - 0.07; glipizide - 0.11 and glibenclamide - 0.16). This difference was a consequence of lower insulin secretion: in glimepiride, the average plasma insulin level was 0.6 μU/ml, in gliclazide, 1.3; in glipizide - 1.6 and glibenclamide - 3.3 μU / ml (G. Muller, 2000). The least stimulating effect of glimepiride on insulin secretion provides a lower risk of hypoglycemia.
The results of these studies show that sulfonylureas have some degree of peripheral effect, but this effect is more pronounced with glimepiride. The peripheral effect of glimepiride is due to the activation of GLUT-4 translocation (to a lesser extent GLUT-2) and an increase in the synthesis of fat and glycogen in fat and muscle tissue respectively. In the plasma membrane of adipocytes under the influence of glimepiride, the amount of GLUT-4 is 3-3.5 times higher, and that of insulin is 7-8 times higher. In addition, glimepiride causes dephosphorylation of GLUT-4, which is an obligate condition for stimulating key enzymes of lipogenesis (glycerol-3-phosphate acyltransferase) and glycogenesis (glycogen synthetase). Glimepiride, like glibenclamide, increases the activity coefficient of glycogen synthetase to 45-50% of the maximum effect of insulin. At the same time, the activity of glycerol-3-phosphate acyltransferase increases to 35-40% of the maximum effect of insulin. Glimepiride inhibits the activity of protein kinase A and lipolysis through the activation of cAMP-specific phosphodiesterase.
The most effective drug from the group of sulfonylurea drugs is glibenclamide, which was introduced into clinical practice in 1969. The biological half-life is 5 hours, and the duration of the hypoglycemic effect is up to 24 hours. The metabolism of the drug occurs mainly in the liver by turning into two inactive metabolites, one of which is excreted in the urine, and the second is excreted through the gastrointestinal tract. The daily dose is 1.25-20 mg (the maximum daily dose is 20-25 mg), which is prescribed in 2, less often in 3 doses 30-60 minutes before meals. Glibenclamide has the most pronounced hypoglycemic effect among the entire group of sulfonylurea drugs, and in this regard, it is rightfully considered the "gold standard". On the domestic market, glibenclamide is presented in tablets of 5; 3.5; and 1.75 mg. And the last two dosage forms are a micronized form, which allows maintaining its therapeutic concentration in the blood at a lower dose of the drug, i.e. with a lower dose of the drug, it is possible to achieve a higher efficiency of its action. If the bioavailability of glibenclamide in tablets of 5 mg is 29-69%, then its micronized forms are 100%. Glibenclamide (5 mg) is recommended to be taken 30-40 minutes before a meal, and its micronized forms - 7-8 minutes. The maximum action of micronized glibenclamide almost completely coincides with post-absorption hyperglycemia, therefore, in patients receiving micronized forms of the drug, hypoglycemic conditions are much less common, and if they develop, they proceed in a mild form.
Glipizide has been used to treat type 2 diabetes since 1971 and is almost equivalent to glibenclamide in terms of hypoglycemic effect. It is rapidly and completely absorbed from the gastrointestinal tract. The biological half-life in plasma is 2-4 hours, the hypoglycemic effect lasts 6-12 hours, and its retard form has a duration of action of 24 hours.
Along with this, dosage forms of known drugs (gliclazide and glipizide) with a prolonged action have been obtained. The prolongation of the action of these drugs is due to the use of technologies that allow slowing down the absorption of the drug from the intestine.
Gliclazide proposed as a hypoglycemic drug in 1970. Gliclazide is also a second-generation drug, its daily dose is 30–120 mg (available in 30 mg tablets). Our studies have shown that in the treatment with gliclazide in patients there was a significant decrease in platelet aggregation, a significant increase in the relative disaggregation index, an increase in heparin and fibrinolytic activity, an increase in heparin tolerance, which made it possible to speak about the normalizing effect of gliclazide on the functional state of platelets. There was a significant trend towards improvement in the aggregation function of erythrocytes, as well as a decrease in blood viscosity at low shear stresses. Plasma coagulation factors of blood coagulation, fibrinolysis, indicators of protein and lipid metabolism also tended to normalize. It stabilizes the course of microangiopathy and even causes regression in some cases.
Gliquidone is also a derivative of sulfonylurea, and it is also referred to as second-generation drugs. However, like gliclazide, in terms of its characteristics, it does not fully possess all the characteristics that apply to this group. The drug is available in tablets of 30 mg, and the daily dose is 30-120 mg. The difference between gliquidone and this group of drugs is that 95% of the drug taken orally is excreted through the gastrointestinal tract and only 5% through the kidneys, while almost 100% of chlorpropamide and 50% of glibenclamide are excreted in the urine. The hypoglycemic effect of gliquidone is weaker compared to the listed drugs.
In addition, to the great satisfaction of endocrinologists, glimepiride was proposed in the second half of the 1990s for the treatment of type 2 diabetes. This is the first sulfonylurea drug with a prolonged action and a low therapeutic dose (1-4 mg per day) compared to other sulfonylurea drugs. These differences made it possible to attribute glimepiride to the III generation of sulfonylurea drugs.
Glimepiride - the first sulfonylurea drug with a prolonged action and a low therapeutic dose (1-4 mg per day) compared to other sulfonylurea drugs. These differences made it possible to attribute it to the third generation (generation) of sulfonylurea drugs. The half-life of glimepiride is longer (more than 5 hours) than that of other drugs in this group, which ensures its therapeutic efficacy during the day. The drug is prescribed once a day at a dose of 1-4 mg, the maximum recommended dose is 6 mg. Glimepiride is completely metabolized in the liver to metabolically inactive products.
For many years, various pharmaceutical companies have been conducting research to find new oral hypoglycemic drugs. One of these developments is the synthesis of a new oral hypoglycemic substance - repaglinide , which is a derivative of benzoic acid. Repaglinide is structurally related to meglitinide, which has a non-sulfonylurea moiety of glibenclamide and, like sulfonylureas, stimulates insulin secretion by the mechanism described for sulfonylureas.
Biguanides. The second group of oral hypoglycemic drugs includes biguanides, which are represented by phenethylbiguanide (phenformin), N,N-dimethylbiguanide (metformin) and L-butylbiguanide (buformin).
The difference in the chemical structure of these drugs has little effect on their pharmacodynamic effect, causing only a slight difference in the manifestation of the hypoglycemic activity of each of them. but metformin is not metabolized in the body and is excreted unchanged by the kidneys, while phenformin is only 50% excreted unchanged, and the rest is metabolized in the liver. These drugs do not change insulin secretion and have no effect in its absence. Biguanides increase peripheral glucose utilization in the presence of insulin, reduce gluconeogenesis, increase glucose utilization by the intestine, which is manifested by a decrease in the level of glucose in the blood flowing from the intestine; and also reduce the increased content of insulin in the blood serum in patients suffering from obesity and type 2 diabetes. Their long-term use has a positive effect on lipid metabolism (reducing cholesterol, triglycerides). Biguanides increase the amount of GLUT-4, which is manifested in the improvement of glucose transport through the cell membrane. It is this effect that explains their potentiating effect on the action of insulin. The site of action of the biguanides is also probably the mitochondrial membrane. By inhibiting gluconeogenesis, biguanides contribute to an increase in the content of lactate, pyruvate, alanine, i.e. substances that are precursors of glucose in the process of gluconeogenesis. Due to the fact that under the action of biguanides the amount of increasing lactate exceeds the formation of pyruvate, this may be the basis for the development of lactic acidosis (lactate acidosis).
In Russia, as in all countries of the world, only metformin is used from the biguanide group. The half-life of metformin is 1.5-3 hours. The drug is available in tablets of 0.5 and 0.85 g. Therapeutic doses are 1-2 g per day (up to a maximum of 2.55-3 g per day).
The hypoglycemic effect of metformin is due to several mechanisms. Decrease in glucose in the blood flowing from the liver indicates a decrease in both the rate and the total amount of glucose produced by the liver, which is a consequence of the inhibition of gluconeogenesis through inhibition of lipid oxidation. Under the influence of metformin, the utilization of glucose in the periphery increases due to the activation of the post-receptor mechanisms of action of insulin and, in particular, tyrosine kinase and phosphotyrosine phosphatase. In addition, the peripheral effects of metformin are also mediated by its specific effect on the synthesis and pool of glucose transporters in the cell. . Increased utilization of glucose in the intestinal mucosa. The number of glucose transporters (GLUT-1, GLUT-3 and GLUT-4) is increased by metformin in the plasma membrane of both adipocytes and monocytes. Increased transport of glucose in the endothelium and vascular smooth muscle, as well as in the heart muscle. It is this effect that explains the decrease in insulin resistance in patients with type 2 diabetes under the influence of metformin. An increase in insulin sensitivity is not accompanied by an increase in its secretion by the pancreas. At the same time, against the background of a decrease in insulin resistance, the basal level of insulin in the blood serum decreases. In patients treated with metformin, there is a decrease in body weight, in contrast to what can occur with an overdose of sulfonylurea drugs and insulin. Moreover, the decrease in body weight occurs mainly due to a decrease in adipose tissue. In addition, metformin contributes to the reduction of lipids in the blood serum. At the same time, the concentration of total cholesterol, triglycerides, low and very low density lipoproteins decreases and, possibly, the level of high density lipoproteins increases, which has a positive effect on the course of macroangiopathy.
In recent years, it has been established that under the influence of metformin, fibrinolysis increases, which is reduced in patients with type 2 diabetes and is an additional factor in thrombosis and vascular complications of diabetes. The main mechanism of action of metformin on the increase in fibrinolysis is a decrease in the level of plasminogen activator inhibitor-1, which occurs in patients with type 2 diabetes, regardless of its dose. In addition to reducing the activity of the plasminogen activator-1 inhibitor, metformin also reduces the proliferation of smooth muscle cells in the vascular wall in vitro and the rate of atherogenesis in animals.
Metformin does not reduce blood glucose below its normal level, which is why there are no hypoglycemic conditions in the treatment of diabetic patients with this drug.
It was noted above that sulfonylurea drugs stimulate insulin secretion, and metformin promotes glucose utilization by peripheral tissues, i.e. drugs, acting on various mechanisms, contribute to better compensation for diabetes. Combination therapy with sulfonylurea drugs and metformin has been used for a long time and with good effect. Therefore, some firms have already mastered the production of combined drugs.
Alpha-glucosidase inhibitors (acarbose)- this is the third group of oral hypoglycemic drugs that have been widely used to treat diabetes in the last 8-10 years in order to reduce the absorption of carbohydrates from the intestines and the main effect of which is associated with inhibition of the activity of enzymes involved in the digestion of carbohydrates. It is known that food carbohydrates, more than 60% of which are starch, are first hydrolyzed in the gastrointestinal tract by specific enzymes (glycosidases: beta-glucuronidase, beta-glucosaminidase, alpha-glucosidase, etc.) and then decompose to monosaccharides. The latter are absorbed through the intestinal mucosa and enter the central circulation. Recently, in addition to the main action - inhibition of glucosidases, alpha-glucosidase inhibitors have been shown to improve peripheral glucose utilization by increasing the expression of the GLUT-4 gene. The drug is well tolerated by patients and can be used to treat patients with type 2 diabetes in the case when it is not possible to achieve compensation for carbohydrate metabolism only on a diet and adequate physical activity.
The usual doses of acarbose are from 50 mg per day, gradually increasing to 50 mg 3 times a day, and then up to 100 mg 3 times a day. In this case, it is possible to avoid such undesirable phenomena as discomfort in the gastrointestinal tract, flatulence, loose stools. The drug must be taken with the first sip of food (i.e. during meals). With monotherapy with acarbose, there is no hypoglycemia.
Potentiators (or sensitizers) of insulin action increase the sensitivity of peripheral tissues to insulin. The drugs in this group include glitazones or thiazolidinediones - pioglitazone and rosigditazone.
Algorithm for the treatment of type 2 diabetes
Thus, the modern algorithm for the treatment of type 2 diabetes includes: diet therapy, lifestyle changes (regular physical activity, smoking cessation, patient education), and in the absence of an effect, the additional use of acarbose. In the presence of obesity, anorectics may be recommended. In case of insufficient effect from taking acarbose with excess body weight (ideal body weight 30 kg / m 2 or more), combined treatment with metformin or sulfonylurea drugs (with ideal body weight up to 30 kg / m 2). In these cases, a combination of metformin with sulfa drugs (in case of overweight) is possible. Insulin sensitizers (pioglitazone, usually 30 mg once daily) can be used alone or in combination with sulfonylurea drugs and metformin. All listed oral hypoglycemic drugs can be used as monotherapy or in combination.
With an unsatisfactory effect of the ongoing treatment, further insulin therapy is indicated. The criteria for prescribing insulin therapy in type 2 diabetes are: lack of compensation for diabetes when using diet therapy in combination with glucosidase inhibitors, biguanides, insulin sensitizers or insulin secretogens (sulfonylureas and drugs derived from amino acids) and the so-called secondary insulin resistance to oral drugs.
According to various authors, secondary resistance to sulfonylurea drugs occurs in 5-20% of patients with diabetes and is associated with a decrease in residual secretion of insulin. Secondary resistance to oral drugs after 1 year from the onset of the disease is detected in 4.1% of patients, and after 3 years - in 11.4%.
The study of the pathogenesis of secondary resistance to oral drugs made it possible to establish its various mechanisms. In some patients, secondary resistance to hypoglycemic oral drugs occurs with reduced residual secretion of insulin and C-peptide, while antibodies to cell antigens of the pancreatic islets are absent. Based on the features clinical course diseases, these patients can be divided into 2 groups: 1) patients with type 2 diabetes with temporary insulin demand; 2) patients with a constant need for insulin or even with insulin dependence (LADA subtype).
The first group consists of patients with diabetes lasting 10 years or more and overweight. To compensate for carbohydrate metabolism, it is recommended in these cases two treatment tactics. The first is the complete transfer of patients to insulin therapy for a short time (2.5-4 months). This time is enough to remove glucose toxicity and lipotoxicity with the restoration of the sensitivity of beta cells to sulfonylurea drugs and the restoration of the reserve capacity of the pancreatic islets. A prerequisite for the removal of glucose toxicity is the achievement of full compensation for diabetes during the period of insulin therapy. In the future, patients are again transferred to oral therapy with good or satisfactory compensation results.
The second tactic is to conduct a combination therapy with insulin and oral hypoglycemic drugs. For the treatment of patients with type 2 diabetes with secondary resistance to oral drugs, we have been using both treatment tactics for 10-12 years. We used combination therapy with insulin in a daily dose, as a rule, not more than 30 IU. per day (usually intermediate-acting insulin). It is more expedient to prescribe insulin at night, i. at 22 or 23 o'clock. The onset of action of such an insulin preparation occurs in the morning hours or during the period when there is an excess production of glucose by the liver. The result of this is a significant reduction in fasting glycemia. In some cases, it is necessary to administer these insulin preparations twice (in the morning and at 22-23 h). During the day, to maintain the hypoglycemic effect, it is recommended to take sulfonylureas (glimepiride at a dose of 2-3 mg per day, glibenclamide at a dose of 10-15 mg per day or gliclazide at a dose of 60-180 mg per day). Insulin therapy is recommended to start with 10-12 IU. and increase by 2-4. every 3-4 days until fasting glycemia drops to 5-6.8 mmol / l. Determination of glycemia during the day is necessary at least once a week during the period of selection of doses of hypoglycemic drugs (insulin and oral drugs). It is extremely necessary, in addition to determining fasting glycemia, to have data on the content of glucose in the blood before lunch and dinner, as well as 1 hour after a meal.
In cases where patients require insulin therapy, the latter can be carried out in a multiple injection regimen or more often in a double injection regimen. In the latter case, good results were obtained by us with the use of combined insulin preparations. Combined insulin preparations are administered before breakfast and before dinner.
In addition, the double-dose regimen can be used when using short-acting and intermediate-acting insulin preparations. In this case, before breakfast, it is necessary to use short-acting and medium-acting insulin, before dinner - a short-acting insulin preparation and before bedtime (at 22 or 23 hours) - medium-acting insulin. The ratio of short-acting insulin preparation to intermediate-acting insulin in the morning is 1:3 (25% and 75%), and in the evening - 1:2 or even 1:1. The regimen of multiple insulin injections, which is necessary for the control of type 1 diabetes, was also used to treat patients with type 2 diabetes. In these cases, both intermediate-acting and long-acting insulin preparations can be used as basal-acting insulin. However, there is little to no advantage of the multiple injection regimen over the double injection regimen.
As for the dose of insulin, to compensate for type 2 diabetes, a daily dose of 0.6-0.8 units per 1 kg of body weight is required. In some cases, the dose of the drug has to be increased to 0.9-1.0 units per 1 kg and even more. This is due to insulin resistance, which is so characteristic of type 2 diabetes. When diabetes compensation is achieved in such cases, insulin demand decreases and, accordingly, the doses of insulin necessary to maintain diabetes compensation are reduced.
Achieving compensation for diabetes mellitus 2 is a prerequisite for the prevention of vascular complications, early disability and increased mortality in this disease.