A lung abscess is considered a bomb that causes damage to the body.
An abscess is a purulent-destructive formation, the development of which can be rapid or gradual.
Find the answer
Are you having any problem? Enter “Symptom” or “Name of the disease” into the form, press Enter and you will find out all the treatment for this problem or disease.Symptoms
Symptoms of an abscess appear in 2 stages.
Before purulent exudate enters the bronchus, this period will be accompanied by:
- Increasing temperature indicators;
- Feeling of chills;
- Increased level sweating;
- Dry cough, which will be accompanied by painful sensations from the location of the outbreak;
- Heavy breathing and even shortness of breath;
- In severe cases it may develop respiratory failure.
By percussion, a shortening of the sound will be observed over the area where the lesion is localized, and by auscultation, harsh breathing will be heard.
The formation of an abscess in the lung will indicate general form patient and will be observed:
- Change in skin color, it will become pale;
- The appearance of a cyanotic blush on the face, especially on the affected side;
- Forced position of the patient, more often he will lie on his side on the affected side;
- Decline blood pressure, tachycardia and arrhythmia.
After perforation into the bronchus, a cough will be observed, which is accompanied by the release of a large amount of purulent and unpleasant-smelling sputum (up to 500 ml.).
If the abscess cavity is well drained, the patient's general condition will improve. After 1.5-2 months, the pathological manifestations of the abscess will disappear.
If drainage is insufficient, the following will be present:
- Body temperature indicators are at the same high level,
- Feeling chilly;
- Sweating;
- Nonproductive cough;
- Dyspnea;
- Manifestations of intoxication of the whole body;
- Lack of appetite;
- Fingers in the shape of " drumsticks” and nails reminiscent of a “watch glass”.
If a positive variant of the course of the disease is observed, which is accompanied by perforation of the abscess into the bronchus, one should expect a speedy recovery. 
If the course of the disease is unfavorable, it will be accompanied by the formation of various complications:
- Pyopneumothorax;
- Empyema of the pleura;
- Bacteremic shock;
- Sepsis;
- Pulmonary hemorrhage.
Of all these complications, bleeding occurs most often. It occurs as a result of injury to the bronchial arteries.
We can talk about bleeding if there is a cough with the release of blood, the amount of which exceeds 50 ml.
Pulmonary hemorrhage is accompanied by expectoration of sputum containing admixtures of red foamy blood. There may be cases when blood is released from the oral cavity without preliminary coughing impulses.
If the bleeding is intense enough, it will be accompanied by a decrease in blood pressure, pale skin, and a frequent pulse with weak filling. This pathological condition is considered quite dangerous, because it leads to the death of the patient.
How does lung gangrene differ from an abscess?
A lung abscess should be understood as a disease characterized by purulent melting of lung tissue, in most cases with a tendency to delineate. Lung gangrene is expressed, like an abscess, by putrefactive decay of lung tissue, but without the presence of a tendency to delineation.
But both pathological conditions are often accompanied by similar characteristics. This is confirmed by the fact that there are cases when an abscess is accompanied by putrefactive changes without signs of delineation.
With gangrene of the lung, especially with mild form flow, the process of putrefactive decay may stop and form a delimited cavity.
It is quite difficult to separate these diseases from each other from the point of view of etiology and pathogenesis. Certain differences can be observed in the clinical symptoms of these pathological conditions, because with gangrene the sputum has bad smell(smelly).
Treatment of these diseases is carried out according to almost the same scheme, so it is often considered the best option to describe these pathological conditions together.
Classification and reasons
In medical practice, it is customary to classify diseases according to:
- Reasons for formation. An abscess is considered primary if the cause of its appearance is trauma. chest. We can talk about a secondary abscess in the presence of severe respiratory diseases.
- Localization in the body. There is a central abscess, when the lesion is localized in the center of the lung, and a peripheral abscess, which is located closer to the periphery of the lung.
- Duration of the flow. Basically, the acute course of the disease is distinguished, the duration of which is 1.5 months; after this period, recovery is observed. Chronic, it lasts more than six weeks and is characterized by alternating periods of exacerbation and remission.
- The nature of the disease. There is a mild course, which will be accompanied by the appearance of cough and shortness of breath, moderate severity- pathological manifestations will be moderate and severe, which is accompanied by clinical manifestations of high intensity disease, and there is a risk of life-threatening complications.
An abscess is considered a process; it is infectious in nature and is caused by bacteria or fungi. Microorganisms penetrate into the lung cavities along with the blood flow from foci of infections present in the body. 
In most cases, the causes of abscess formation are considered to be:
- Pneumonia;
- Blocking of the lumen of the bronchus by a tumor or foreign body, which leads to impaired patency through it and the development of stagnation of mucus in the lower sections with the addition of an infectious process;
- Entry of gastric contents into the respiratory tract;
- Sepsis.
Factors that help develop the disease include:
- Smoking;
- Drinking alcoholic beverages;
- General hypothermia;
- Decreased body resistance;
- Chronic respiratory diseases;
- Flu.
Pathogenesis and stages of development
Most often, the occurrence of an abscess in the body is preceded by clinical picture focal inflammation of the lungs, accompanied by fatigue, stress, and disorders of the nervous system.
As a result of the collapse of the lung parenchyma, a decrease in local immunity is observed, and this makes it easier for pathogens to enter the lung tissue.
An abscess is necrotic lung tissue that is separated from healthy tissue. If there is a high level of body resistance, the affected tissues are isolated from healthy ones by forming a capsule.
More often there is only one abscess in the lung, but sometimes there are situations in which there are many purulent cavities. The tissues located around are also involved in inflammation; it occurs with a lower level of intensity.
If the appearance of an abscess in the lung tissue was preceded by its infarction, then circulatory disorders will play a major role. Over time, the infectious process will join; it will descend along the bronchial tree.
As a result, we can conclude that various factors play a large role in the pathogenesis of the disease, to which others are added over time.
The following main stages of the disease are distinguished:
- Infiltration.
- Decay.
- Breakthrough.
- Healing.
But it is taken into account that the presented dynamics can change and become more complex, and this will lead to a chronic process.
Video
Acute and chronic type of disease
Medical workers:
- Gangrenous course of the disease, which is formed as a result of contact with the affected area pathogenic flora, bacteria and fungi.
- Acute abscess, accompanied by a feeling of severe pain in the chest, hemoptysis, shortness of breath and cough with purulent sputum. In case of perforation of the abscess cavity into the lumen of the bronchus, an improvement in the general condition of the patient will be observed. The process will be characterized by a cough with the release of a large amount of sputum, which will have a rotten odor.
- Chronic abscess is characterized by alternating exacerbations and remissions. An exacerbation of the disease will be characterized by all manifestations of an acute abscess. If remission is observed, then the chest pain will weaken, but a barking cough will appear, with an increase in the amount of sputum produced and increased sweating, especially at night. A characteristic symptom of remission is the rapid fatigue of a sick person.
Necessary diagnostic measures
Most informative method X-ray examination is considered diagnostic.
It can be carried out both in direct and lateral projection.
Will be observed characteristic symptoms:
- Round shadow syndrome;
- Blurred contours;
- The nature of the abscess content will be uniform;
- Enlargement of lymph nodes at the root of the localization of the lesion process;
- Thick walls that separate the affected area.
But it must be remembered that each stage of the disease has differences on the x-ray. If the photo is taken on initial stages disease, then the abscess cavity will be small in size, up to 4 cm. Perifocal foci of inflammatory nature and deformation of the pulmonary pattern will be present.
There will also be an increase in the fluid level; this symptom will be noticeable if the examination is carried out over time. Over time, the inner wall of the ring-shaped shadow becomes denser and smoother. 
An abscess in the drainage stage will look like this: thinning of the wall is observed, clearing is visible in the center, sequesters will be located above the fluid level. The outer part of the capsule becomes blurred due to a purulent inflammatory process.
An abscess that has cleared is indicated by the thinned walls of the capsule; the cavity does not contain fluid. Over time, these walls are overgrown with connective tissue, so the size of the cyst will not change for a certain time, and a scar is formed.
In the case of a favorable course of the disease, the purulent cavity passes quite easily.
With a favorable course of the disease, the cyst goes through 3 stages:
- Acute, will last 3 months;
- Chronic, which will be present for a month and a half;
- False cyst.
Effective treatment of the disease
The sooner the disease is identified and its treatment is started, the more successful the prognosis will be.
Persons with an abscess of lung tissue require immediate hospitalization and inpatient treatment. Oxygen inhalation and a balanced diet are prescribed.
Treatment should consist of:
- Carrying out drainage to eliminate pus in the lesion;
- Drugs that will have a detrimental effect on pathogenic microflora;
- Means to combat the manifestations of intoxication in the body;
- Means that provide improved immunity;
- Symptomatic drugs.
In case of ineffectiveness conservative treatment or if indications are present, surgical intervention is performed.
Antibacterial drugs are used in maximum doses. For example, penicillin is administered intravenously up to eight times a day (up to 8-10 units).
Before prescribing an antibacterial drug, the sensitivity of the microflora is determined. For treatment, a combination of several antibacterial drugs and routes of their introduction into the body can be used.
Washing abscesses through a bronchoscope is considered quite common and effective. For this purpose they use saline, furagin. After such washings, proteolytic enzymes, bronchodilators and antibiotics are introduced into the bronchial tree.
To eliminate purulent exudate in the lesion, transthoracic punctures are also performed. For the same purpose, postural drainage is used, the essence of which is to provide a position for the patient that would promote and facilitate the discharge of sputum.
Aerosol therapy and therapeutic exercises are carried out.
Possible complications of the disease
Complications that can develop as a result of the presence of a lung abscess include:
- Lack of therapeutic effect from the prescription of antibacterial drugs and the transition of the disease to chronic stage or to the other side;
- Entry of purulent contents into the pleural cavity with the formation of pleural empyema;
- Thrombosis of the veins and arteries leading to and from the lungs;
- Formation of bronchopulmonary fistulas;
- Hemoptysis;
- Pulmonary hemorrhage;
- Clinical recovery, which will be accompanied by clearance of the abscess through the bronchus and the formation of an air cyst;
- Bacteremia, which leads to toxic shock;
- Diffuse pneumonia, which occurs as a result of pus entering the Airways(as a result of abscess perforation);
- Brain abscess, inflammation of the meninges;
- Death.
To prevent the formation of a lung abscess, it is necessary to try to avoid respiratory diseases, and if they are present, carry out timely and adequate treatment.
Doctors advise:
- Do not overcool;
- Eat a balanced diet;
- Get rid of bad habits (smoking, alcohol abuse);
- In the presence of colds seek medical help in a timely manner;
- If pneumonia is suspected, a mandatory x-ray examination is necessary.
Under the influence of pathogenic microorganisms on the lung tissue, it is destroyed. This is how a lung abscess and a more severe form of infectious destruction—its gangrene—occurs. These diseases are accompanied by necrosis of the pulmonary area and its collapse.
A lung abscess is a formation in the form of a cavity, usually round in shape, filled with purulent contents. It is surrounded by a shell consisting of fibers connective tissue and a section of the lungs saturated with immune cells and blood proteins.
Lung abscesses
A much more serious condition is lung gangrene. It is accompanied by rapidly spreading tissue necrosis and is not delimited from healthy areas.
Gangrenous abscess is an intermediate variant between these two conditions, tending to be separated from normal tissue.
These diseases occur predominantly in males aged 20 to 55 years. The frequency of the disease has decreased significantly over the past decades, but the mortality rate remains quite high - up to 10%. If gangrene is caused by Pseudomonas aeruginosa, Klebsiella or Staphylococcus aureus, the incidence of adverse outcomes increases to 20%.
Classification

Smoking is a risk factor for lung abscess
Conditions that increase the risk of lung abscess or gangrene:
- smoking experience;
- diabetes;
- flu illness;
- alcohol abuse;
- immunodeficiency states;
Infectious destruction of lung tissue occurs in severe neurological diseases(consequences of stroke, myasthenia gravis, amyotrophic sclerosis), with prolonged vomiting, epileptic seizures, foreign object in the bronchi. Risk factor is any operation under general anesthesia, as well as the use of narcotic substances. Finally, the penetration of microbes into the lungs is facilitated by stomach diseases, accompanied by the reflux of its contents into the esophagus, or, for example,.
Development of the disease
Germs usually enter the lungs through the upper respiratory tract. Often their source is in the nasopharynx, for example, with tonsillitis. Very often, microbes are inhaled along with microscopic particles of stomach contents after vomiting or gastroesophageal reflux. The disease often occurs when there is a bruise or wound to the chest.
Microorganisms that enter the alveoli cause an inflammatory reaction, which is accompanied by increased penetration into this area immune cells blood. Leukocytes actively destroy pathogens, forming enzymes that destroy proteins and pus. The resulting cavity is surrounded by a dense cell wall.
After 15–20 days, the abscess opens into the nearest bronchus and empties. The cavity collapses, leaving behind a focus of compacted (sclerosed) lung.
Gangrene develops faster. As a result of circulatory disorders, the active action of pathogens causes inflammation to not be limited, and a large area of necrosis of the lungs occurs. Here, many disintegrating foci are identified, some of which are emptied through the bronchi. During gangrene, a large amount of toxic metabolic products enter the blood, causing severe intoxication (poisoning) of the body.
Clinical signs
The disease is usually preceded by. An abscess forms within 14 days.
Signs of the disease before the abscess empties:
- high fever with chills and sweat;
- cough without phlegm;
- increased breathing rate;
- slight cyanosis of lips, hands, feet.
After the abscess empties, which occurs on days 4–12 of illness, the following appears:
- cough attack with a single release of purulent sputum in a volume of up to 0.5 l;
- decrease in temperature and improvement of condition.
If the abscess cavity is poorly cleaned, the following symptoms develop:
- repeated increase in temperature, chills, sweating;
- difficult separation of sputum with a foul odor when coughing;
- rapid breathing;
- lack of appetite, weight loss;
- lethargy, headache, nausea;
- thickening of the nail phalanges; nails become round and convex.
Lung gangrene is accompanied by similar, but more pronounced symptoms:
- fever up to 40°C and above;
- tremendous chills, severe sweating;
- lack of appetite and weight loss;
- when coughing and breathing - chest pain;
- attacks of coughing with a large amount of purulent sputum.
Diagnostics
The disease is diagnosed by a therapist or pulmonologist, taking into account the conditions preceding the disease, the duration and severity of symptoms. Since destruction of lung tissue is often found in pneumonia, the doctor must regularly and carefully perform percussion and auscultation in order to suspect the disease in time and refer the patient for additional diagnostics.
Laboratory signs
Blood analysis:
- increased number of leukocytes;
- the appearance of rod forms;
- increase in ESR;
- anemia is possible.

Large lung abscess with fluid level
Lung abscess must be distinguished from the following diseases:
- respiratory cancer;
- cyst;
- actinomycosis;
- Wegener's granulomatosis;
- empyema of the pleura.
Therapeutic measures
Therapy is carried out only in a hospital.
High calorie food with high content squirrel. Fat should be limited slightly. Very useful for patients:
- decoction of rose hips;
- boiled liver;
- fruits, vegetables, juices.
Salt and liquid intake should be slightly reduced.
Medicines
The basis of treatment is . The duration of their use reaches 2 months. At first antibacterial drugs prescribed empirically. These are modern inhibitor-protected penicillins, such as amoxicillin and clavulanic acid.
Second line agents:
- lincomycin + aminoglycosides or cephalosporins;
- fluoroquinolones + metronidazole;
- carbapenems.
Once sensitivity results are obtained, the regimen can be adjusted. First, the drugs are administered intravenously, then in tablets.
Detoxification is prescribed using intravenous solutions, symptomatic remedies(antipyretics, vitamins, restoratives).
The abscess can be drained during bronchoscopy, and it can also be punctured through the surface of the chest, using ultrasound or radiography for control.
Vibration massage and postural drainage are prescribed.
Operation
Surgical intervention is performed in 10% of patients. Indications:
- ineffectiveness of antibiotics;
- likelihood of lung cancer;
- abscess diameter more than 60 mm;
- chronic form of abscess or gangrene;
- breakthrough into the pleural cavity.
Depending on the size of the pathological focus, the appropriate part of the lung or the entire organ.
Rehabilitation and prognosis
After discharge, the patient is observed by a pulmonologist. Control X-ray prescribed 3 months after recovery.

Simple breathing exercises
At home it is necessary to carry out breathing exercises. Among folk remedies, one can note the effectiveness of honey and beekeeping products. Inhalations with garlic juice, essential oils of eucalyptus and pine are also useful. It is recommended to use infusions of chamomile, linden blossom, raspberry, and rose hips.
After a lung abscess, recovery occurs in 60–90% of cases. In 15–20% of patients, a chronic abscess develops. Mortality does not exceed 10%. With severe gangrene of the lung, unfavorable outcomes are recorded in more than 40% of cases.
To avoid such a serious disease, prevention is necessary to eliminate risk factors. They are listed in the corresponding section of our article.
The most common complications of acute abscess and gangrene of the lungs are:
Pulmonary hemorrhage;
Pyopneumothorax (pleural empyema);
Sepsis (septicopyemia);
Damage to the contralateral lung (due to bronchogenic spread of purulent sputum).
Chapter 8. Forecast
The prognosis of the disease is determined by:
The mechanism of disease development (aspiration, post-pneumonic, embolic abscess, etc.);
The nature of the microflora and associated pathological changes in lung tissue;
The state of the macroorganism (chronic suppurative lung diseases, severe general somatic diseases, bad habits, presence of immunodeficiency, etc.);
Features of therapeutic and diagnostic measures (timeliness of hospitalization in a specialized department, early diagnosis and scope of treatment measures, etc.);
Presence of complications.
Depending on the above factors, acute lung abscess occurs:
With a tendency to recover when under the influence complex treatment clinical manifestations of the disease are quickly eliminated, the abscess cavity decreases and either a focus of looped fibrosis (complete recovery) or a dry cavity (recovery with a “defect”) forms at the site of the abscess;
The healing of the abscess occurs slowly, the cavity is emptied of pus
not enough, subsides poorly, regeneration processes are slow - acute abscess becomes chronic;
In patients with concomitant pathology, with a particularly virulent infection and poor drainage of the abscess through the bronchus, the disease progresses with the development of complications, the formation of new abscesses in the contralateral lung (reflux of purulent sputum) or internal organs (metastatic abscesses), impaired cardiac function, renal function, and liver and can lead to the death of the patient.
A favorable course of pulmonary gangrene is rare and only with complex intensive therapy (antibiotics, detoxification, sanitation of the bronchial tree, immune correction, etc.), which subsequently does not exclude the need for surgical intervention.
Chapter 9. Differential diagnosis I
The differential diagnosis of acute lung abscesses is carried out mainly with malignant neoplasms, tuberculosis, suppurating cysts and pulmonary echinococcus.
Abscess formation in lung cancer is not uncommon. In case of central cancer and complete obstruction of the bronchus by a tumor, suppuration develops in the area of atelectasis or obstructive pneumonitis, in case of peripheral lung cancer - in the center of the tumor against the background of necrosis and decay of tumor tissue.
In differential diagnosis, it is necessary to take into account the patient’s age, medical history, differences in the severity of individual clinical symptoms, and the dynamics of the disease during conservative treatment.
A methodologically competent (at least 5 tests) cytological examination of sputum is of great importance: with abscesses and gangrene of the lungs, a large number of neutrophilic leukocytes, elastic fibers, bronchial epithelial cells with pronounced dystrophic changes, and nonspecific microflora are detected; For lung cancer, the detection of tumor cells is typical.
On X-ray examination, lung cancer is clearly characterized
defined area of the lesion and the absence of perifocal inflammatory
changes, the presence of atelectasis (subsegment, segment, lobe of the lung); in later stages of lung cancer, a path of cancerous lymphangitis appears, connecting the tumor i. with the root, an increase in the hilar lymph nodes is determined;
for an abscess easily i is characterized by pronounced infiltration of lung tissue without clear boundaries, art. The structure of the lung root is usually preserved. There are also differences in outline; ; external and internal walls of the cavity in case of lung cancer and abscess: in case of peripheric cancer, the outer contours of the shadow are lumpy, indistinct in places, with the presence of delicate strands going into the lung tissue (cancerous lymphangitis, corona inaligna); in case of a lung abscess, the outer contours of the shadow are indistinct (blurred) ; the internal walls of the cavity in peripheral cancer are uneven, undermined; in abscesses, as a rule, the destruction cavity is located in the center of the infiltrate, its internal walls are smooth and clear; in the case of an abscess, on targeted tomograms you can see the lumen of the bronchus draining the abscess; in case of lung cancer, the draining bronchus is not visible.
Computed tomography or magnetic resonance imaging is crucial in some cases, because more clearly reveals both the tumor itself (along the tissue density gradient) and the invasive nature of its growth, as well as the presence of signs of intrathoracic lymphadenopathy.
Endoscopic examination in combination with biopsy data (detection of tumor cells in the biopsy specimen) plays a decisive role in central lung cancer;
for peripheral cancer, definitive information can be obtained by transthoracic i-sectional biopsy - cell detection malignant tumor in puncture confirms the diagnosis of cancer.
In recent years, the number of patients with blocked lung abscesses has increased. Under block! This lung abscess should be understood as the presence in the lung of a limited zone of nonspecific suppuration with complete or partial disruption of the patency of the draining bronchus. In two thirds of patients, blocked lung abscesses occur without pronounced clinical manifestations and are detected radiographically as round or oval shading with clear, bumpy contours, often on an intact pulmonary background, with localization mainly in the upper parts of the lung (Fig. 4).
In the diagnosis of blocked lung abscesses, a carefully collected anamnesis with a targeted search for clinical manifestations of the onset and
course of the disease, taking into account the dynamics of laboratory and radiological data,
“endoscopic picture in comparison with the effectiveness of the treatment.
With blocked abscesses, the presence of destruction can be detected on tomograms. Selective bronchography helps in clarifying the diagnosis; filling the abscess cavity with contrast through a partially closed bronchus or through adjacent bronchi is pathognomonic for a lung abscess. If the result of selective bronchography is negative, it is necessary to perform a transbronchial or transthoracic biopsy of the formation - the presence of a cytological picture of nonspecific purulent inflammation (neutrophilic leukocytes in the lysis stage, purulent detritus, macrophages, histiocytes, pyogenic microflora) and the absence of tumor cells allows us to exclude the diagnosis of peripheral lung cancer in the vast majority of patients .
Differential diagnosis of acute lung abscess and infiltrative
pneumonic tuberculosis in the decay phase is helped by anamnesis data (occupation, contact with tuberculosis patients), examination of sputum, bronchial lavage water, culture of sputum on special media to identify mycobacterium tuberculosis, bronchoscopy with a biopsy of the bronchial mucosa, intensity of response to tuberculin (Mantoux test) , enzyme-linked immunosorbent assay (determination of antibodies to mycobacteria), as well as x-ray examination, especially tomograms of the lungs, which often reveal fresh tuberculosis foci (foci of screening) near the destruction cavity.
Suppurating lung cysts occur with a less pronounced clinical picture than lung abscesses: moderate cough, mucopurulent sputum, odorless, fever lasts 2-3 days and quickly disappears under the influence of antibiotics. Radiologically, suppurating lung cysts have a characteristic appearance - these are single thin-walled cavities of a round or oval shape, with thin walls without perifocal inflammatory infiltration.
It should be remembered that the detection of cavity or spherical formation syndrome in the lungs in patients over 45-50 years of age requires, first of all, the exclusion of lung cancer and wait-and-see tactics are unacceptable here. If there is a suspicion of cancer and it is impossible to prove this diagnosis using the above methods, a diagnostic thoracotomy with urgent histological examination of the surgical material (lung tissue, lymph nodes, pleura) is indicated, which finally resolves the issue of diagnosis and determines further treatment tactics for the patient.
Abscess and gangrene of the lung as separate nosological forms were identified by Rene Théophile Hyacinthe Laennec in 1819. Ferdinand Sauerbruch (1920) proposed to group these diseases under common name"pulmonary suppuration".
G.I. Sokolsky (1838) in “The Doctrine of chest diseases, taught in 1837 in the Department of Medical Sciences of the Imperial Moscow University to students of the 3rd, 4th and 5th courses,” gave a detailed clinical description of acute abscess and gangrene of the lung. The first report on surgical treatment of gangrene dates back to 1889, when N.G. Freiberg described pneumotomy performed by K.K. Reier.
The treatment of acute pulmonary suppuration received a solid scientific basis in the 20th century. In 1924 I.I. Grekov reported 20 years of experience surgical treatment gangrene of the lung using pneumotomy. Supporters of this operation were S.I. Spasokukotsky and A.N. Bakulev. In the second half of the last century, in the clinics of A.P. Kolesova, P.A. Kupriyanova, A.N. Bakuleva, V.I. Struchkova, A.A. Vishnevsky, F.G. Uglova, I.S. Kolesnikova, M.I. Perelman, E.A. Wagner is actively developing radical anatomical resections and pneumonectomy for acute abscess and gangrene of the lung.
Over the past 10-15 years, the problem of suppurative lung diseases has rarely been discussed in foreign literature, but remains still relevant for our country. With widespread destruction of the lungs caused by an association of highly virulent, multi-resistant microorganisms, treatment results still remain unsatisfactory and high mortality remains: for acute abscess it is 2.5-4%, limited gangrene (gangrenous abscess) - 8-10%, widespread - 45 -50%.
Main features of pathology
Lung abscess is an intrapulmonary cavity limited by the granulation shaft and the zone of perifocal infiltration, formed as a result of the disintegration of necrotic areas of lung tissue and containing pus.
Lung gangrene is necrosis of a significant area of lung tissue, usually a lobe, two lobes or the entire lung, without demarcation, with a tendency to further spread. Destruction cavities in lung gangrene always contain necrotic sequestration.
Etiology and pathogenesis
When any etiological factor of suppurative lung diseases occurs, acute pneumonia with known clinical manifestations first develops. In most cases, as a result of timely rational therapy, acute inflammatory process reversible - the infection is suppressed, the alveolar exudate is resorbed, the inflammatory infiltrate resolves. Otherwise, under certain conditions and unfavorable circumstances, necrosis of the lung tissue develops, followed by the formation of destruction cavities.
The first information about the pathogenesis of acute abscess and gangrene of the lung was given in 1871 by L. Traube. They concerned primarily the state of the bronchial tree during the development of an intrapulmonary suppurative process without taking into account the role of the infectious factor.
The respiratory tract has effective local and systemic mechanisms that maintain the sterility of terminal bronchioles and lung parenchyma. The pathogen contaminates the respiratory tract as a result of inhalation of an aerosol of small particles, aspiration of oropharyngeal secretions, or by hematogenous route.
Aspiration of oropharyngeal contents is prevented by cough and supraglottic reflexes. Mechanical retention at the level of the upper parts of the tracheobronchial tree in combination with mucociliary transport prevents contamination of the peripheral parts of the respiratory tract. If the infectious agent reaches the alveolar level, cellular and humoral mechanisms designed to eliminate pathogenic microorganisms.
Under certain conditions, the protective mechanisms of bronchopulmonary structures are damaged and an inflammatory process develops. Predisposing factors for this are alcoholism, drug addiction, epilepsy, traumatic brain injury, overdose sedatives, general anesthesia, coma of any origin and other conditions causing disturbances of consciousness. It is with them that the respiratory tract is easily contaminated by the aggressive microflora of the oropharynx.
In the etiopathogenesis of acute pulmonary suppuration, non-spore-forming anaerobic microorganisms play a leading role. More than 300 types of pathogens of this group are known that can cause lung destruction. Of the purulent foci, Bacteroides, Fusobacterium, Peptostreptococcus, Peptococcus and others are most often isolated, that is, the flora that usually colonizes the nasopharyngeal area.
In acute abscess and gangrene of the lung, non-spore-forming anaerobes are always found in association with aerobic hospital strains. Most often these are Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, etc.
In the pathogenesis of bacterial destruction of the lung great importance is attributed to impaired patency of bronchial branches with the formation of atelectasis, as well as impaired blood circulation in the bronchial and pulmonary vessels with the development of ischemia of bronchopulmonary structures.
Classification
Taking into account the experience of our clinic and on the basis of previously known classifications, we have proposed a classification scheme, and we do not insist on its indisputability, but we believe that in practical terms it is quite convenient.
- Etiology
- Postpneumonic
- Post-traumatic
- Aspiration
- Obstructive
- Hematogenous
- Clinical characteristics
- Acute abscess
– Single
– Multiple (unilateral or bilateral)
- Lung gangrene
– Limited (gangrenous abscess)
– Common
- Morphological characteristics
- Liquation necrosis - “wet” gangrene
- Coagulative necrosis - “dry” gangrene
- Collision-coagulation necrosis – mixed type
- Complications
- Empyema of the pleura
– With bronchopleural communication
– Without bronchopleural communication
- Pulmonary hemorrhage
- Aspiration inflammation of the opposite lung
- Phlegmon chest wall
- Pulmonary sepsis
Epidemiology
Statistical data on the prevalence of this pathology are not systematized, inaccurate and contradictory. Acute abscess and gangrene of the lung develop more often in men (67%) of working age - 45-55 years. Most patients are socially disadvantaged and abuse alcohol and tobacco.
Hematogenous (always bilateral) lung abscesses occur with angiogenic sepsis. 2/3 of these patients suffer from drug addiction. Quite often, their lung destruction is combined with bacterial endocarditis and HIV.
Diagnostics
In general, the clinical picture of acute abscess and gangrene of the lung is identical, but there are differences, primarily in the severity of the patients’ condition, the severity of endogenous intoxication and multiple organ failure.
Clinical manifestations of acute abscess depend on the stage and period of the disease. Lung destruction does not develop suddenly. This is always preceded by acute, usually protracted, pneumonia of various etiologies.
Abscessation of the lung significantly worsens the patient's condition. Weakness and malaise increase, and febrile temperature appears. Later, chest pain develops, worsening with inspiration, and a nonproductive cough.
As the infectious process progresses and the volume of destruction increases, body temperature becomes hectic, its rises are accompanied by heavy sweats. The nonproductive cough intensifies, which has the character of a painful paroxysmal cough. Intoxication and respiratory failure are increasing.
Listed Clinical signs characteristic of a lung abscess that does not communicate with the tracheobronchial tree. If qualified treatment is not started at this stage of the disease, then the next stage of the disease is a spontaneous breakthrough of the abscess into the regional (usually segmental) bronchus.
Against the background of a persistent cough, the patient suddenly coughs up foul-smelling purulent sputum with a mouth full. Within a day after this, the patient’s condition improves somewhat - signs of intoxication, chest pain, shortness of breath decrease, and the temperature decreases.
When examining a patient with an acute lung abscess, pale skin with a grayish tint, cyanotic lips and nail beds are detected. Shallow breathing due to pain in the chest. With percussion, a shortening of the sound can be detected if the abscess is located in the lung cloak; with auscultation, a weakening of breathing, dry and moist rales can be detected.
As a result of intoxication, respiratory failure, chest pain, the patient has tachycardia and hypotension is possible. A general blood test reveals pronounced leukocytosis, a neutrophil shift, and an increase in ESR.
Even more manifest manifestations of pulmonary destruction are found in patients with lung gangrene. The condition is severe or extremely serious. Severe weakness, frequent shallow breathing, febrile or hectic temperature, anorexia.
The patient is exhausted, the skin is pale with a bluish-gray tint. The skin feels dry to the touch. The position is forced - sitting, leaning on outstretched arms. The ribs are contoured in relief under soft tissues. The chest wall on the affected side does not participate in breathing, the intercostal spaces are narrowed.
The main feature is that the intolerantly fetid purulent sputum with fibrin and small sequestration of lung tissue is continuously coughed up with a full mouth in a daily volume of 500.0 to 1500.0(!) ml or more (due to multiple bronchial fistulas through which purulent fluid is drained into the respiratory tract). content pleural cavity- pleural empyema).
With percussion - shortening of the sound over the damaged lung. Auscultation determines a sharp weakening of breathing or its absence on the side of the pathology. Scattered dry and moist rales are heard over the contralateral lung due to aspiration of purulent sputum from the bronchi of the diseased lung.
A clinical blood test determines severe anemia hyperleukocytosis, shift of the formula to juvenile forms, toxic granularity of neutrophils, increased ESR.
As before, the basic method for confirming the clinical diagnosis of bacterial destruction of the lung remains polypositional fluoroscopy and chest radiography, which allows confirming the diagnosis and determining the localization of the process. In case of acute lung abscess, before it communicates with the bronchial tree, a regular round homogeneously darkened cavity with perifocal infiltration is determined. After the abscess has emptied into the respiratory tract, there is a cavity with a fluid level.
The X-ray picture of a gangrenous abscess is characterized by a cavity within the lung lobe with a bay-shaped irregular outline of the internal contour due to necrotic sequestration of the lung tissue.
Common gangrene of the lung is characterized by total darkening of the hemithorax on the side of the disease with small irregular air cavities, hydropneumothorax (pleural empyema).
Computed tomography should be considered the gold standard for radiological diagnosis of lung diseases, which allows a detailed study of the structure of the cavity formation, its localization and differential diagnosis of suppurative and other diseases, in particular, cancer and pulmonary tuberculosis.
The list of mandatory instrumental studies of suppurative lung diseases includes fiber-optic bronchoscopy, which allows assessing the severity and prevalence of endobronchitis, diagnosing a foreign body, bronchodilitis or bronchial tumor, and collecting material for microbiological and cytological studies.
It is necessary to differentiate between acute abscess and gangrene of the lung, first of all, with destructive forms tuberculosis process.
Certain difficulties arise in the differential diagnosis of acute abscess and peripheral lung cancer with decay (cavitary tumor form). Often suppuration with the formation of intrapulmonary cavities develops in patients with central cancer of the segmental, lobar or main bronchi. This occurs as a result of infection of atelectatic areas of the lung tissue (obstructive pneumonitis), the natural evacuation of contents from which becomes impossible due to tumor obstruction.
The differential series should also include aspergilloma and echinococcus of the lung and other diseases with clinical and radiological syndrome of acute suppuration.
Anamnesis, clinical manifestations and the data of modern methods of radiodiagnosis form the basis of the differential diagnosis for lung diseases, but the final diagnosis is established based on the study of the results of microbiological, cytological and histological studies.
The material for research is taken from the tracheobronchial tree (fiber bronchoscopy), during transcutaneous puncture of pathological formations of the lung and pleura under the control of computed tomography or ultrasound.
Empyema of the pleura- the most typical complication of acute bacterial destruction of the lung. It develops as a result of a breakthrough of an intrapulmonary abscess into the pleural cavity. As a rule, the empyema cavity communicates through the focus of destruction with the tracheobronchial tree (bronchopleural fistulas), which causes the formation of pyopneumothorax with lung collapse.
Pleural empyema worsens the patient's condition due to increased resorption of toxins, deterioration of gas exchange in unaffected areas of the collapsed lung and displacement of the mediastinum to the healthy side.
With acute empyema, the patient feels a sharp pain in the chest. Shortness of breath increases, cyanosis appears. During auscultation on the affected side, breathing cannot be heard or is greatly weakened. Percussion reveals tympanitis over the upper parts of the hemithorax and shortening of the sound in the basal parts.
Plain radiographs (frontal and lateral projection) reveal a picture of hydropneumothorax with a horizontal fluid level and lung collapse.
Treatment
Treatment of acute bacterial destruction of the lung is the absolute prerogative of surgeons. top scores are achieved in specialized thoracic departments. The severity of the patient's condition requires a variety of intensive care, parasurgical procedures and emergency surgical interventions if complications occur.
Conservative and parasurgical treatment
Conservative treatment includes infusion media and medications, capable of correcting homeostasis disorders that develop as a result of prolonged intoxication, hypoxemia and anorexia. Methods of efferent therapy and gravitational surgery are used, provided that the abscesses are adequately drained.
When a patient with acute bacterial destruction of the lungs is admitted to a surgical hospital, he is immediately prescribed empirical antibiotic therapy, based on data on the polymicrobial etiology of pleuropulmonary infection. Subsequently, the prescriptions are adjusted taking into account the results of microbiological examination of the contents of the abscesses.
In the treatment of acute abscess and gangrene of the lung, combination (2 or more drugs) antibacterial therapy is often used. Examples of such combinations could be:
- 3rd generation cephalosporin + aminoglycoside (amikacin) + metronidazole;
- aminoglycoside (amikacin) + clindamycin;
- fluoroquinolone 3-4 generations + metronidazole;
- tigacil.
However, monotherapy using cefoperazone/sulbactam or carbopenems is possible. IN acute period For diseases, antibiotics are prescribed mainly intravenously. An indispensable condition for antibacterial therapy is the prevention of systemic mycosis with antifungal agents (Diflucan, Mycosist, flucosanol, etc.).
A leading role in the pathogenesis of bacterial destruction of the lung is played by impaired bronchial obstruction. To restore bronchial drainage, it is necessary to use a variety of methods sanitation of the tracheobronchial tree.
Simple and enough effective method emptying the purulent cavity is postural drainage. To implement it, the patient is given a position in which the abscess is above the draining bronchus. For example, when an abscess is localized in the 2nd or 6th segments of the lung (posterior segments), the patient is placed on his stomach with the head end of the bed slightly lowered, which creates conditions for the natural outflow of infected contents into the respiratory tract, followed by active coughing. It is advisable to combine positional drainage with vibration massage of the chest.
This method is not effective enough if thick purulent sputum and sequestration of lung tissue block the draining bronchus. In these situations, it is advisable to use selective sanitation of the pathological focus using a catheter, which is inserted transcutaneously into the trachea.
Under local anesthesia, completely painlessly, a puncture of the cricoid ligament (fossa canina) is performed, a radiopaque, specially modeled catheter is inserted through a needle into the trachea using a Seldinger-type technique, the tip of which, under the control of an electron-optical converter or fiberoptic bronchoscope, is installed into the draining bronchus or purulent cavity. Through the catheter, lavage (12-14 drops per minute) of the pathological area is carried out with solutions at room temperature with the addition of antiseptics, antibiotics and prolonged proteolytic enzymes.
In patients with large and giant subpleural ulcers containing detritus, fibrin, sequestration of pulmonary tissue, it is advisable to combine intrabronchial sanitation with percutaneous drainage of the infected cavity, which was proposed by A. Monaldi (1938) for the treatment of tuberculous cavities.
A breakthrough of the abscess into the pleural cavity requires additional parasurgical procedures.
Some methods of treating empyema have been known since the time of Hippocrates. Following his principle “ubi pus ibi evacua,” the great doctor pierced the patient’s chest with a hot iron rod or knife and inserted bronze tubes into the pleural cavity, removing pus.
They do the same thing nowadays, using modern devices and instruments. In case of total pleural empyema, two drains are installed: in the second intercostal space along the middle clavicular and in the seventh along the posterior axillary lines. The contents of the pleural cavity are evacuated by vacuum.
In case of pleural empyema with bronchopleural communications, active aspiration is not effective enough - the lung cannot be straightened. In addition, steal syndrome develops due to excessive evasion of air from the respiratory tract, and hypoxemia intensifies.
In this case, it is advisable to carry out selective occlusion of the fistula-bearing bronchus with polyurethane foam (foam rubber). The occluder is passed through the tube of a rigid bronchoscope and installed under visual control at the mouth of the segmental or lobar bronchus draining the abscess. The bronchopleural communication stops, and re-expansion of the lung occurs due to the straightening of the “healthy” segments.
A special place in the treatment of acute suppurative lung diseases is occupied by pulmonary hemorrhage- a complication that most often ends in the death of the patient. Patients with massive pulmonary hemorrhage die as a result of flooding of the respiratory tract with blood (the volume of the tracheobronchial tree is 80-120 cm3) and asphyxia.
The first task in case of massive pulmonary hemorrhage is to stop the flow of blood into the “healthy” parts of the tracheobronchial tree. To do this, rigid tracheobronchoscopy is urgently performed, the side of the bleeding is determined and, if possible, the lobar or segmental localization of the source. After obturation of the main or lobar bronchus with a foam rubber occluder, the airways are freed from spilled blood.
The second task is to detect the bleeding vessel and perform endovascular occlusion. As a rule, this can be done in patients with acute lung abscess, where selective angiography reveals hyperplasia of the bronchial artery with pronounced hypervascularization of the pathological area and extravasation of contrasted blood.
If X-ray endovascular occlusion of the bronchial arteries is successful, then a repeat bronchoscopy is performed, the occluder is removed, a thorough sanitation of the tracheobronchial tree is performed, and conservative treatment of the underlying disease continues. Otherwise, emergency surgery is prescribed.
The situation is more complicated in patients with pulmonary gangrene, since the source of massive, usually pulmonary-pleural, bleeding is the branches of the pulmonary artery and the tributaries of the pulmonary veins. The possibility of endovascular surgery in these cases is limited. In rare cases, it is possible to stop bleeding by implanting Gianturko coils into the branches of the pulmonary artery.
Surgery
Targeted conservative and parasurgical treatment in the majority of patients with acute lung abscess (95-97%) allows one to avoid emergency surgery. The indication for surgical intervention for the pathology in question is ongoing bleeding.
In approximately 3-5% of cases, acute lung abscess does not end with recovery and the disease becomes chronic with typical remissions and exacerbations. It is difficult to judge definitively the timing of transformation of an acute abscess into a chronic one, however, it is generally accepted that an acute abscess that is not cured within 2 months should be classified as a group of chronic pulmonary suppurations that require active surgical treatment.
On the contrary, with widespread gangrene of the lung there is no alternative to emergency surgery, since conservative and parasurgical treatment ends in death for the vast majority of patients. In patients with limited gangrene (gangrenous abscess), it is possible to use a gentle, organ-preserving operation such as pneumotomy or thoracopleuroabscessostomy.
The operation consists of a projection limited thoracotomy through the bed of resected 1-3 ribs in the area closest to the pathological process. Pus and sequestration of lung tissue are removed. The edges of the parietal pleura and skin are sutured, forming a pleuroabscessostomy for subsequent long-term open sanitation of the purulent cavity.
The disadvantage of this operation is considered to be a high probability of developing phlegmon of the chest wall, osteomyelitis of the ribs, and arrosive bleeding. In addition, limited gangrene of the lung occurs infrequently, in contrast to the common process, when surgical intervention through limited access is impossible.
Therefore, despite the very serious condition of the patients, radical surgery has to be performed, usually in the form of anatomical pneumonectomy. These operations are accompanied by severe complications and high mortality, but there is no other way to solve the problem.
To prevent the flow of purulent sputum into the opposite lung (the patient is on the operating table in the position on the healthy side), endoscopic occlusion of the main bronchus on the affected side is performed on the eve of the operation. Along with this, separate intubation of the bronchi is performed, for example, with a Carlens tube.
Access: anterolateral thoracotomy in the fifth intercostal space. Pus, fibrin and sequestration of lung tissue are removed from the pleural cavity. Processed sequentially pulmonary artery, superior and inferior pulmonary veins. As carefully as possible, without extensive skeletonization, the main bronchus is isolated, stitched with a device, and cut off. The lung is removed. The bronchial stump is additionally sutured with 3/0 monofilament atraumatic sutures and, if possible, pleurized.
The pleural cavity is thoroughly sanitized, drains are installed, and layer-by-layer sutures are applied to the wound. The removed lung consists of non-structural necrotic parenchyma and exposed segmental bronchi, arteries and veins (which is why gangrene of the lung is often complicated by profuse pulmonary-pleural bleeding).
The most common complication postoperative period with anatomical resection of the lung, the bronchial stump is found to be incompetent (50-70%). The main causes of its occurrence are a pronounced inflammatory process in the wall of the bronchus (panbronchitis), widespread aerobic-anaerobic pleural empyema. It is also important that reparative processes in patients with lung gangrene are suppressed as a result of gross disturbances of homeostasis and secondary immunodeficiency.
The failure of the bronchial stump is diagnosed on the basis of a significant intake of air through the pleural drainage during coughing and forced breathing, and an increase in respiratory failure. Confirmed by fiberoptic bronchoscopy.
To treat the complication that has arisen, rethoracotomy is performed, resection of the bronchial stump with repeated suturing. Relapse of insolvency occurs in 92-95% of cases. If it is possible to stabilize the patient’s condition and suppress the acute infectious process in the pleural cavity, then a bronchopleural fistula, chronic pleural empyema, is formed.
Analysis of the pathogenesis of pulmonary destruction suggests that this is not only and not so much a medical problem, but rather a socio-medical one. Therefore, an important stage in the prevention of the occurrence of suppurative lung diseases is the improvement of living conditions, health education and medical examination of the population, timely diagnosis and treatment for early stages community-acquired pneumonia, immediate referral of the patient to a specialized department if a pulmonary-pleural complication occurs.
Lung abscess is a disease characterized by the formation of a cavity with pus in the lung tissue, delimited from undamaged parts by a pyogenic capsule that forms during the development of inflammation. Lung gangrene characterized by necrosis of a large mass of pulmonary tissue. In the absence of delimitation of the destructive process from the unaffected parts of the lung by an inflammatory-granulation shaft and the progression of necrosis with its spread to the entire lung, the disease is designated as widespread gangrene. If the process is delimited by an inflammatory-granulation shaft, then this limited gangrene (gangrenous abscess). Abscess and gangrene of the lung are the most common acute suppurative diseases of the lungs. They belong to the group of nonspecific destructions of the lung and are characterized by necrosis of the pulmonary parenchyma with its disintegration, melting of dead lung tissue with the formation of cavities in this area.
Classification infectious destruction of the lung
· the nature pathological process :
1. Acute purulent abscess;
2. Acute gangrenous abscess;
3. Widespread gangrene of the lung;
4. Chronic abscess.
· according to the severity of the clinical course:
light, medium, heavy.
· by the nature of the flow:
1. Uncomplicated;
2. Complicated (pleural empyema, pulmonary hemorrhage, sepsis, pneumonia of the opposite lung, etc.).
In addition, lung abscesses can be single or multiple, unilateral or bilateral.
Etiology and pathogenesis.
In the pathogenesis of acute suppuration of the lungs, 3 factors play a leading role:
1. Impaired bronchial obstruction;
2. Acute infectious process in the pulmonary parenchyma;
3. Impaired blood supply to a section of lung tissue, causing its necrosis.
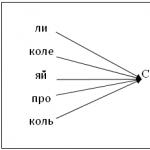
Processes in lung tissue develop schematically as follows:
· Trigger mechanism – violation of bronchial obstruction;
· Atelectasis of a section of lung tissue drained by an obstructed bronchus (the alveoli and bronchioles of this section are filled with fluid);
· In conditions of airless lung tissue, the activity of pathogenic microbial flora can lead to circulatory disorders, tissue necrosis and pulmonary suppuration.
Origin of acute suppurative lung diseases:
1. Post-pneumonic lung abscesses (form within 3-4 weeks);
2. Aspiration lung abscesses (form within 1-2 weeks);
3. Traumatic;
4. Hematogenous-embolic;
5. Lymphogenic.
Complaints.
Clinical course acute abscess the lung is usually clearly divided into two periods: 1) the period of formation of a purulent cavity before its breakthrough into the bronchus, and 2) the period after the abscess breaks through into the draining bronchus. First period Acute purulent abscess is characterized by an acute onset with an increase in body temperature to 38 degrees or more, chest pain and a cough - dry or with a small amount of sputum. Phenomena of severe general intoxication are observed, and complaints are associated with it - general weakness, malaise, sweating, fatigue, loss of appetite, headaches.
Second period characterized by a breakthrough of the abscess into the lumen of the bronchus, which is accompanied by the appearance of bad breath and a large amount of purulent sputum (200 ml or more per day), a decrease in temperature to subfebrile, a decrease in the manifestations of general intoxication and an improvement in the general condition of the patient.
For gangrene or gangrenous abscess lung, the clinical picture of the disease is characterized by a more severe condition of the patient. Severe intoxication comes first, up to the development of septic shock, and respiratory failure develops. There are complaints of severe weakness, lack of appetite, thirst, painful cough with foul-smelling sputum of a brown, gray-brown color, which, after settling, is divided into three layers: the lower one is a crumbly sediment, the middle one is liquid, the upper one is mucopurulent, foamy. Sometimes the foul odor during breathing is so pronounced that it becomes impossible for others to stay near the patient. The course of lung gangrene is often complicated by hemoptysis, pulmonary hemorrhage, pleural empyema, pyopneumothorax, which significantly aggravates the patient’s condition.
Examination of the patient. Physical examination data in the first period are scarce: against the background of fever, weakened breathing in the affected area, various dry and moist rales are detected. The first period usually lasts 7-10 days, and the listed symptoms are mistakenly interpreted as manifestations acute pneumonia. The ineffectiveness of the therapy should lead one to suspect the presence of a lung abscess. After the abscess breaks through into the draining bronchus, a decrease in temperature is noted, and multiple moist rales of various sizes are heard over the affected lung. Gangrene and gangrenous lung abscess are characterized by lethargy and adynamism of the patient. Skin dry, grayish in color. Lips and nail beds are cyanotic. The affected side of the chest lags behind in the act of breathing. Physical data depend on the volume of necrosis of the lung tissue and the severity of its disintegration - dullness of percussion sound, its boxy hue above the destruction cavity located superficially. On auscultation, there is a significant weakening or absence of respiratory sounds, an amphoric hue over the cavity draining through the bronchus, and various moist rales.
Diagnostics.
1. General analysis blood reveals an increase in the number of leukocytes with a shift in the leukocyte formula to the left. With gangrene of the lung, there is a sharp leukocytosis (more than 30,000), an acceleration of ESR of more than 70 mm/h, changes in the leukocyte blood count with a predominance of young forms, pronounced toxic granularity of neutrophils, and significant anemia.
2. Biochemical research blood. Characterized by severe hypoproteinemia, dysproteinemia, water-electrolyte imbalance, and severe metabolic acidosis.
3. Bacteriological research sputum and pus with determination of microflora and its sensitivity to antibiotics, as well as examination of sputum for the presence of tubercle bacilli and fungal flora.
Instrumental studies:
1. X-ray examinations of the chest (fluoroscopy, radiography, tomography, CT scan) in the first clinical period, massive infiltration of lung tissue is detected, mainly within 1-2 segments or lobes of the lung. In the second period X-ray examination makes it possible to detect a destruction cavity with a horizontal fluid level against the background of decreasing infiltration of lung tissue, which confirms the diagnosis of a lung abscess. With gangrene of the lung in the initial phases, massive confluent infiltration of the lung tissue within a lobe or the entire lung is radiologically determined. As decay progresses against the background of infiltration of the lung tissue, multiple destruction cavities of various sizes and degrees of filling with contents are determined. Lung tomography reveals tissue sequestration irregular shape, located freely or near the wall in the largest cavities of destruction.
2. Bronchoscopy allows you to exclude the tumor nature of the process and collect material for bacteriological and cytological examination.
Treatment.
Treatment of acute lung abscess follows 3 main directions:
1. The most complete and constant drainage of purulent foci of the lung;
2. Therapeutic effect on the microbial flora of foci of suppuration;
3. Stimulation of the body's defenses.
For adequate drainage of purulent foci in the lung, use:
· Postural drainage (giving the patient’s body an optimal position for the free discharge of pus into the draining bronchus “by gravity”);
· Chest massage, vibration massage, breathing exercises;
· Inhalations with soda, bronchodilators;
· Expectorants orally;
· Bronchoscopic sanitation of the bronchi;
· Intratracheal infusions of drugs;
· Catheterization of the segmental bronchus draining the abscess by percutaneous puncture of the anterior wall of the trachea.
Antibacterial therapy should be carried out taking into account the nature of the microflora and its sensitivity to antibiotics. In the absence of this data, use a combination antibacterial agents:
3rd generation cephalosporins +
Aminoglycosides (amikacin or gentamicin) +
· Metronidazole.
Monotherapy with imipenem (thienam) or meronem is also possible.
To stimulate the body's defenses, use:
· High-calorie, protein- and vitamin-rich nutrition;
· Antistaphylococcal gamma globulin;
· Transfusion of hyperimmune plasma;
· Infusions of albumin, protein, amino acids;
· Detoxification therapy (fluid infusions, forced diuresis);
Surgical treatment of acute lung abscess is performed when conservative treatment is ineffective and consists of the following:
Drainage of the abscess cavity using a trocar or a thick needle with a tube (preferably double-lumen);
Lung resection(most often – 1 lobe, lobectomy). Indications: massive pulmonary hemorrhage, failure of conservative treatment, abscess > 6 cm in diameter, pyopneumothorax.
The only treatment for lung gangrene is surgery. After stabilizing the patient's condition with the help of conservative therapy for 7–10 days (if there is no pulmonary hemorrhage or rapid progression of the disease), extensive resection of the dead part of the lung or the entire lung is performed.