Increasing pain in the perineum, high fever and problematic sitting on a chair - although delicate problems, they interfere with the usual pace of life so much that they make even the most shy people apply for medical care.
In a quarter of cases of pathology of the rectum, a proctologist diagnoses paraproctitis and prescribes an operation.
In search of an opportunity to avoid surgical intervention, the patient must clearly understand the danger of complications of paraproctitis in case of untimely or incomplete treatment.
Paraproctitis: what is it?
Paraproctitis is an acute, in the absence or ineffectiveness of treatment, turning into a chronic form. purulent inflammation tissue of the pararectal zone. In other words, in the perirectal space filled with adipose tissue, an abscess is formed - an abscess.
The purulent process that has begun cannot be stopped: in any case, necrosis of infected tissues occurs. In addition, acute paraproctitis has a high chance of becoming chronic.
Spontaneous opening of the abscess gives only temporary relief, and repeated suppuration is fraught with the formation of a fistula that goes either into the lumen of the rectum or through the skin of the anal zone.
Most often, paraproctitis is diagnosed in men. Very rarely, the disease develops in children after surgical removal. birth defects development of the anus and narrowing of the rectum.
The severity of the symptoms of paraproctitis, the lack of chances for self-healing and the effectiveness of non-surgical therapy, as well as serious complications require immediate medical attention when the first symptoms of the disease appear and qualified surgical care.
Forms of pathology
- downstream - acute (formed for the first time) and chronic (formed fistulas);
- according to the depth of the location of the pathology - superficial, deep;
- according to the localization of purulent foci - subcutaneous, submucosal, intrasphincteral (located between the fibers of the external and internal sphincter), ischiorectal (abscess located in the perineum, outside the anal sphincter), pelviorectal (high location, high threat of a total purulent process);
- by the presence of a fistulous exit - incomplete (there is only an entrance through the anal crypt) and complete (the abscess has found an exit through the skin, into the abdominal space or into the lumen of the rectum);
- in relation to the fistula to the anal sphincter - intra-, extra- and transsphincteral;
- according to the complexity of the structure of fistulous passages - simple and complex (the presence of several passages, streaks and purulent pockets).

The main culprits of paraproctitis are anaerobic bacteria: E. coli, often in common with staphylococci and streptococci.
The infection enters the tissue surrounding the rectum through the ducts of the glands (morgagian crypts) that open into the anal canal or through microdamages of the rectal mucosa.
The hematogenous / lymphogenous route of infection is not excluded. Pathogen from chronic foci of infection (caries, sinusitis, chronic tonsillitis) with the flow of blood or lymph reaches the anal zone and multiplies in the perirectal tissue.
Factors provoking the development of paraproctitis:
- haemorrhoids,
- nonspecific ulcerative colitis,
- anal and rectal fissures,
- Crohn's disease,
- constipation,
- reduced immunity,
- atherosclerosis of the rectal vessels,
- gynecological diseases in women and prostatitis in men,
- diabetes,
- surgery on the rectum.
Symptoms and signs of paraproctitis, photo
Acute paraproctitis always begins suddenly.
General symptoms:
- temperature increase,
- weakness,
- muscle pain, lack of appetite.
Specific signs of paraproctitis:
- sharp pains of a pulsating / jerking nature in the rectal area, spreading during defecation to the entire pelvic area;
- painful urination;
- stool disorder and painful urge to empty the bowels;
- with a superficial location of a purulent focus - swelling and redness of the skin with a possible opening and outflow of pus.

Self-opening of an abscess can occur through the skin (the most favorable option), into the lumen of the vagina in women, into the rectum, into the abdominal space with the formation.
The walls of the purulent cavity and the fistulous passage are gradually lined with epithelium, chronic paraproctitis is formed with periodic exacerbation and the release of purulent contents.
During remission, it is characterized by an imaginary recovery: the patient's state of health normalizes, working capacity is restored, the wound is covered with scar tissue. However, recurring exacerbations can lead to insomnia, neurasthenia, and impotence in men.
Diagnosis of paraproctitis
Diagnostic examination is designed to accurately determine the location of the fistula and the degree of damage to the sphincter muscle fibers for selection. effective treatment paraproctitis.
A patient with suspected paraproctitis undergoes:
- digital examination of the rectum (identification of the internal mouth of the fistula);
- examination with a probe;
- transrectal ultrasound;
- fistulography.
Paraproctitis treatment and surgery

For many patients, the question arises: is surgery necessary for paraproctitis? In this case, the answer is categorical - the treatment of paraproctitis without surgery is impossible, and delay will only aggravate the purulent process.
Radical treatment is carried out in two stages:
- Opening of the formed abscess and removal of pus, often with drainage. In acute paraproctitis, a fistula is almost always formed after an operation to open a purulent cavity.
- Removal of the fistulous tract and closure of the connection between the rectum and the purulent cavity.
Often, with the surgical removal of the fistula, surgery hemorrhoids.
Surgical intervention is tolerated quite easily, the postoperative period is not very painful.
At the same time, antibiotic therapy and immunostimulation are carried out.
Only such treatment of paraproctitis, which involves two operations under general anesthesia and drug therapy complete cure sick.
 When the first signs of paraproctitis appear, emergency surgical care is needed. The prognosis of the disease depends on the timing of its provision.
When the first signs of paraproctitis appear, emergency surgical care is needed. The prognosis of the disease depends on the timing of its provision.
Chronic paraproctitis is characterized by a high risk of complications:
- Spontaneous opening of an abscess.
- Purulent fusion and necrosis of the walls of the vagina, urethra.
- Exit stool into the perirectal tissue through the necrotic wall of the rectum, lightning spread of the purulent process.
- Breakthrough of an abscess into the abdominal space and the development of peritonitis, which is fatal.
- Insufficiency of the anal sphincter due to severe damage to its fibers, leakage of feces.
- The growth of scar tissue and a decrease in the elasticity of the walls of the anal canal.
- Cancer degeneration in the presence of a fistula for more than 5 years.
Prevention of the formation of paraproctitis
- Timely and complete treatment of rectal pathology.
- Fight against constipation.
- Proper hygiene anal area to avoid crack formation anus.
- Maintaining immunity, eliminating chronic foci of infection in the body.
Paraproctitis according to mcb 10
In the international classifier of diseases, pathology is:
Class XI. Diseases of the digestive system (K00-K93)
K55-K63 - Other bowel diseases
K61 - Abscess of the anus and rectum (Including: abscess or phlegmon of the anus and rectum, with or without a fistula)
- K61.0 Anal abscess
K62 - Other diseases of the anus and rectum
- K62.8 Other specified diseases of anus and rectum/perforation (non-traumatic) of rectum/proctitis NOS
paraproctitis(pararectal abscess) - acute or chronic inflammation of pararectal tissue. It accounts for about 30% of all diseases, the process affects about 0.5% of the population. Men suffer 2 times more often than women, get sick at the age of 30-50 years.
Etiology and pathogenesis. Paraproctitis occurs as a result of microflora (staphylococcus, gram-negative and gram-positive rods) entering the pararectal tissue. With ordinary paraproctitis, polymicrobial flora is most often detected. Inflammation involving anaerobes is accompanied by particularly severe manifestations of the disease - gas cellulitis of the pelvic tissue, putrefactive paraproctitis, anaerobic sepsis. Specific pathogens of tuberculosis, syphilis, actinomycosis are very rarely the cause of paraproctitis.
Ways of infection are very diverse. Microbes enter the pararectal tissue from the anal glands that open into the anal sinuses. In the inflammatory process in the anal gland, its duct is blocked, an abscess is formed in the intersphincteric space, which breaks into the perianal or pararectal space. The transition of the process from the inflamed gland to pararectal tissue is also possible by the lymphogenous route.
In the development of paraproctitis, injuries of the rectal mucosa by foreign bodies contained in the feces, hemorrhoids, anal fissures, ulcerative colitis, Crohn's disease, and immunodeficiency states can play a certain role.
Paraproctitis can be secondary - with the spread of the inflammatory process to pararectal tissue from the prostate, urethra, female genital organs. Injuries to the rectum are a rare cause of paraproctitis (traumatic).
Classification of paraproctitis
Acute paraproctitis.
According to the etiological principle: ordinary, anaerobic, specific, traumatic.
According to the localization of abscesses (infiltrates, streaks): subcutaneous, ischiorectal, submucosal, pelviorectal, retrorectal.
Chronic paraproctitis (fistulas of the rectum).
According to the anatomical feature: complete, incomplete, external, internal.
According to the location of the internal opening of the fistula: anterior, posterior, lateral.
In relation to the fistulous tract to the fibers of the sphincter: intrasphincteric, transsphincteric, extrasphincteric.
Difficulty level: simple, difficult.
Acute paraproctitis characterized by rapid development of the process.
Clinically, paraproctitis is manifested by rather intense pain in the rectum or perineum, fever, accompanied by chills, malaise, weakness, headaches, insomnia, loss of appetite. Extensive phlegmon of pararectal tissue leads to severe intoxication, the development of a syndrome of dysfunction of vital organs, threatening the transition to multiple organ failure and sepsis. Often there is a delay in stool, tenesmus, dysuric phenomena. As the pus accumulates, the pains intensify, become jerking, throbbing. If the abscess is not opened in a timely manner, then it breaks into the adjacent cellular spaces, the rectum, out through the skin of the perineum.
The breakthrough of the abscess into the rectum is a consequence of the melting of its wall with pus in pelviorectal paraproctitis. A message is formed between the cavity of the abscess and the lumen of the rectum (incomplete internal fistula).
When pus breaks out (on the skin of the perineum), an external fistula is formed. The pain subsides, the body temperature decreases, the general condition of the patient improves.
A breakthrough of the abscess into the lumen of the rectum or outside very rarely leads to a complete recovery of the patient. More often a fistula of the rectum (chronic paraproctitis) is formed.
Subcutaneous paraproctitis is the most common form of the disease (up to 50% of all patients with paraproctitis). Characterized by sharp, jerking pains, aggravated by movement, straining, defecation; dysuria is observed. The body temperature reaches 39 "C, chills often occur. On examination, hyperemia, swelling and swelling of the skin in a limited area near the anus, deformation of the anal canal are revealed. Palpation of this zone causes sharp pain, sometimes fluctuation is determined. Finger examination of the rectum causes increased pain. However, it is advisable to carry it out under anesthesia, since this makes it possible to determine the size of the infiltrate on one of the walls of the rectum near the anal canal and decide on the method of treatment.
Ischiorectal paraproctitis occurs in 35-40% of patients. Initially, general signs of a purulent process appear, characteristic of the syndrome of a systemic reaction to inflammation with a sharp increase in body temperature, chills, tachycardia and tachypnea, and a high content of leukocytes in the blood. Along with this, weakness, sleep disturbance, signs of intoxication are noted. Dull pains in the depths of the perineum become sharp, throbbing. They are aggravated by coughing, physical activity, defecation. With the localization of the abscess in front of the rectum, dysuria occurs. Only after 5-7 days from the onset of the disease, moderate hyperemia and swelling of the skin of the perineum in the area of the abscess is noted. Attention is drawn to the asymmetry of the gluteal regions, the smoothness of the semilunar fold on the side of the lesion. Soreness on palpation medially from the ischial tuberosity is moderate. Very valuable in the diagnosis of ischiorectal ulcers is a digital examination of the rectum. Already at the beginning of the disease, it is possible to determine the soreness and compaction of the intestinal wall above the rectal-anal line, the smoothness of the folds of the mucous membrane of the rectum on the side of the lesion.
Submucosal paraproctitis observed in 2-6% of patients with acute paraproctitis. Pain in this form of the disease is very moderate, somewhat aggravated by defecation. Body temperature subfebrile. Palpation determines the bulging in the lumen of the intestine, in the area of the abscess, sharply painful. After a spontaneous breakthrough of the abscess into the intestinal lumen, recovery occurs.
Pelviorectal paraproctitis- the most severe form of the disease, occurs in 2-7% of patients with acute paraproctitis. Initially, general weakness, malaise, fever to subfebrile, chills, headache, loss of appetite, aching pain in the joints, dull pain in the lower abdomen.
With abscessing of the pelviorectal fiber infiltrate (after 7-20 days from the onset of the disease), the body temperature becomes hectic, symptoms of purulent intoxication are expressed. The pains become more intense, localized, tenesmus, constipation, dysuria are noted. There is no pain on palpation of the perineum. The diagnosis can be confirmed by ultrasound, computed tomography or magnetic resonance imaging. Without instrumental studies, it is difficult to make a diagnosis until the purulent fusion of the pelvic floor muscles leads to the spread of the inflammatory process to the ischiorectal and subcutaneous fatty tissue with the appearance of edema and hyperemia of the skin of the perineum, pain when pressed in this area. During a digital examination of the rectum, infiltration of the intestinal wall, infiltration in the tissues surrounding the intestine and its bulging into the intestinal lumen can be detected. The upper edge of the bulge is not reached with the finger.
Retrorectal paraproctitis observed in 1.5-2.5% of all patients with paraproctitis. Characterized by intense pain in the rectum and sacrum, aggravated by defecation, in a sitting position, with pressure on the coccyx. Pain radiates to the thighs, perineum. With a digital examination of the rectum, a sharply painful bulging of its posterior wall is determined. Of the special research methods, sigmoidoscopy is used, which is informative for pelviorectal paraproctitis. Pay attention to hyperemia and slight bleeding of the mucous membrane in the area of the ampoule, smoothing of the folds and infiltration of the wall, the internal opening of the fistulous passage when the abscess ruptures into the intestinal lumen. In other forms, endoscopy is not needed.
Treatment. In acute paraproctitis, surgical treatment is performed. The operation consists in opening and draining the abscess, eliminating the entrance gate of the infection. The operation is performed under general anesthesia. After anesthesia (narcosis), the localization of the affected sinus is established (examination of the intestinal wall with the help of a rectal mirror after the introduction of methylene blue solution and hydrogen peroxide solution into the abscess cavity). If the breakthrough of the abscess has occurred outward through the skin, then good drainage, as a rule, does not occur.
With subcutaneous paraproctitis, it is opened with a semilunar incision, the purulent cavity is well inspected with a finger, the bridges are separated and purulent streaks are eliminated. A bellied probe is passed through the cavity into the affected sinus and an area of skin and mucous membrane is excised, forming the wall of the cavity together with the sinus (Gabriel's operation). With subcutaneous-submucosal paraproctitis, the incision can be made in the radial direction - from the comb line through the affected anal crypt (the entrance gate of infection) to the perianal skin. Then the edges of the incision are excised, the affected crypt together with the internal opening of the fistula. A bandage with ointment is applied to the wound, a gas outlet tube is inserted into the lumen of the rectum.
With ischiorectal and pelviorectal paraproctitis, such surgical intervention is impossible, since this will cut most of external sphincter. In such cases, the abscess is opened with a semilunar incision, its cavity is carefully examined and all purulent streaks are opened, the wound is washed with a solution of hydrogen peroxide and loosely packed with a gauze swab with dioxidine ointment.
With retrorectal (presacral) acute paraproctitis, a skin incision 5-6 cm long is made in the middle between the projection of the tip of the coccyx with the posterior edge of the anus. At a distance of 1 cm from the coccyx, the anal-coccygeal ligament is crossed. The pus is evacuated, the abscess cavity is examined with a finger, separating the jumpers. The posterior wall of the anal canal, surrounded by the sphincter muscles, is exposed with the help of hooks, where the site of the fistulous passage leading to the intestinal lumen is found. The second stage of the operation - conducting a ligature - is performed in the same way as described above.
Chronic paraproctitis (fistulas of the rectum) occurs in 30-40% of all proctological patients. The disease develops as a result of acute paraproctitis and is manifested by fistulas of the rectum. This happens if there is an internal opening leading from the rectum to the cavity of the abscess. With the formation of chronic paraproctitis, the inner opening of the fistula opens into the lumen of the rectum, the outer one - on the skin of the perineum. Gases and feces enter the fistula from the rectum, which constantly supports the inflammatory process.
Reasons for the transition acute paraproctitis in chronic are: late appeal of patients for medical care after spontaneous opening of the abscess; erroneous surgical tactics in the acute period (opening the abscess without sanitation of the entrance gate of infection).
The fistula may be complete or incomplete. A complete fistula has two or more openings: internal - on the wall of the rectum and external - on the skin of the perineum. An incomplete fistula has one opening on the wall of the rectum, blindly ending in the pararectal tissue (internal fistula).
The fistula of the rectum, depending on its location in relation to the sphincter fibers, can be intrasphincteric, transsphincteric and extrasphincteric.
With an intrasphincteric fistula, the fistulous canal is completely inside the rectal sphincter. Usually such a fistula is straight and short.
With a transsphincteric fistula, part of the fistulous canal passes through the sphincter, part is located in the fiber.
With an extrasphincteric fistula, the fistulous canal passes through the cellular spaces of the pelvis and opens on the skin of the perineum, bypassing the sphincter.
Clinical picture and diagnosis. The amount of purulent discharge from the fistula is different and depends on the volume of the cavity that it drains, as well as on the degree of the inflammatory process in it. With a wide fistulous passage, gases and feces can exit through it, with a narrow one, a meager serous-purulent discharge. Episodic closure of the fistula leads to impaired drainage of the purulent cavity, accumulation of pus, exacerbation of paraproctitis. Such an alternation of exacerbations and remissions is often observed in chronic paraproctitis, the duration of remissions can reach several years.
Pain occurs only with an exacerbation of the disease, disappearing during the functioning of the fistula. On examination, pay attention to the number of fistulas, scars, the nature and amount of discharge from them, the presence of maceration skin. Already with palpation of the perianal zone, it is often possible to determine the fistulous course. A digital examination of the rectum allows you to determine the tone of the sphincter of the rectum, sometimes - to identify the internal opening of the fistula, its size, to establish the complexity of the fistula, its course and features.
Additional information about the localization of the internal opening of the fistula, its course and features, which is necessary for choosing the method of operation, is obtained by introducing methylene blue into the fistula, careful probing of the fistula, fistulography, anoscopy, sigmoidoscopy, endorectal ultrasound.
Treatment. With conservative treatment, sitz baths are prescribed after defecation, washing the fistula with antiseptic solutions, introducing antibiotics into the fistula, using microclysters with sea buckthorn oil, collargol. Conservative treatment rarely leads to a complete recovery of patients, so it is usually used only as a preparatory stage before surgery.
Surgery is a radical treatment for rectal fistulas. The timing of surgical intervention depends on the nature of the course of the disease: in case of exacerbation of chronic paraproctitis, urgent surgical intervention is indicated; in the subacute course of paraproctitis (the presence of infiltrates), anti-inflammatory treatment is carried out for 1-3 weeks, then surgical intervention; in chronic course - a planned operation; in the case of persistent remission, the operation is postponed until the exacerbation of paraproctitis.
Surgical intervention for fistulas of the rectum is carried out depending on the type of fistula (its relationship to the sphincter), the presence inflammatory processes in the pararectal tissue, purulent streaks, the state of tissues in the area of the internal opening of the fistula.
With intrasphincteric fistulas, they are excised into the lumen of the rectum. Excision of the fistula is best done wedge-shaped, together with skin and tissue. The bottom of the wound is scraped out with a Volkmann spoon. In the presence of a purulent cavity in the subcutaneous adipose tissue, it is opened along the probe, the walls are scraped off with a Volkmann spoon and gauze turunda with ointment is injected (levosin, levomekol, etc.), a gas outlet tube is installed.
Transsphincteric fistulas are eliminated by excision of the fistula into the lumen of the rectum with or without suturing the deep layers of the wound (sphincter muscles) and draining the purulent cavity.
With extrasphincteric fistulas, which are the most difficult, they resort to various operations, the essence of which is the complete excision of the fistulous tract and the elimination (suturing) of the internal opening of the fistula. For complex fistulas, the ligature method is used. Incomplete fistulas are excised into the lumen of the rectum using a probe bent at a right angle.
- an inflammatory process in the fiber of the rectum. It is manifested by sharp pain in the anus and perineum, high temperature, chills, defecation and urination disorders. Locally revealed swelling and redness of the anal area, the formation of infiltration and abscess. Complications include the development of chronic paraproctitis, fistulas, involvement of organs in the inflammatory process. genitourinary system, sepsis. Treatment is always surgical acute inflammation perform an autopsy, drainage, in chronic cases, the fistula is excised.
General information
- a disease characterized by inflammation and suppuration of the tissues surrounding the rectum as a result of penetration bacterial infection from the lumen of the rectum through anal glands the bottom of the morganian crypts into the deep layers of the pararectal region. In modern proctology, paraproctitis is divided into acute (first detected) and chronic (long-term, recurrent). Chronic paraproctitis is the result of insufficient or incorrect treatment of acute paraproctitis.
Chronic paraproctitis usually involves the morganian crypt, the space between the internal and external sphincters, and the pararectal tissue. The result of a long-term chronic paraproctitis of this magnitude may be pararectal fistulas of the rectum (pathological channels connecting the rectum to the skin or nearby hollow organs). Identification of pararectal fistula speaks about the acute paraproctitis that took place.

Causes of paraproctitis
The causative agent of infection is most often a mixed flora: staphylococci and streptococci, Escherichia coli. In some cases, there may be specific infection Key words: clostridia, actinomycosis, tuberculosis. Specific paraproctitis occurs no more often than in 1-2% of patients. The development of paraproctitis is facilitated by a decrease in the body's immune properties, general exhaustion, chronic diseases organs and systems, acute or chronic infection digestive tract, specific infectious diseases, stool disorders (constipation or diarrhea), proctological pathologies (proctitis, hemorrhoids, anal fissure, cryptitis, papillitis).
Classification
Paraproctitis, depending on the localization and prevalence of the process, is divided into subcutaneous paraproctitis (pararectal abscess), intrasphincteric, ischiorectal and pelviorectal paraproctitis. Subcutaneous paraproctitis is characterized by purulent fusion of subcutaneous tissue in the perianal region. This type of paraproctitis is the most easily curable and has the most favorable prognosis.
With intrasphincteric paraproctitis, inflammation affects the tissues of the anal sphincter, with ischiorectal paraproctitis, the purulent process is localized in the ileo-rectal fossa. Inflammation in pelviorectal paraproctitis develops inside the small pelvis.
Paraproctitis symptoms
Acute paraproctitis is manifested by symptoms characteristic of local purulent inflammation, pain, hyperemia, hyperthermia and tissue edema, suppuration. Unlike nonspecific aerobic flora, anaerobic microorganisms do not contribute to purulent fusion, but to necrotic destruction of tissues. The predominance of putrefactive anaerobic flora contributes to the development of putrefactive paraproctitis, which is characterized by a massive lesion, a high rate of tissue destruction, and severe intoxication. With non-clostridial anaerobic paraproctitis, muscles and fascial structures are often involved in the pathological purulent process.
Chronic paraproctitis is the result of undertreated acute paraproctitis, so its symptoms most often repeat those of acute paraproctitis, but their severity is usually less. In chronic paraproctitis, an adrectal fistula often develops, which is manifested by secretions in the perineal region of the ichor or pus. Constant discharge contributes to perineal skin irritation and itching.
A well-drained (with a free outlet for pus) pararectal fistula usually does not bother the patient with pain or discomfort. pain symptom characteristic of an incomplete internal fistula. In this case, the pain intensifies during defecation and subsides after it (this is due to improved drainage of the fistula at the time of stretching of the anal valve).
Clinical signs of pararectal fistula appear in waves, subsiding and again aggravating. This is due to periodic blockage of the fistulous lumen, the formation of a purulent abscess, after opening which relief comes. The fistula does not heal on its own, purulent processes in it continue. If blood impurities appear in the purulent discharge, it is necessary to conduct studies on the subject of malignant formation.
Complications
Most dangerous complication acute paraproctitis is the penetration of a purulent process in the pelvic space filled with fiber, as well as purulent fusion of all layers of the intestinal wall above the anorectal line. In this case, stool masses enter the pararectal tissue, affecting nearby organs and threatening the infection to enter the bloodstream (development of sepsis).
The anatomical proximity of the pelvic peritoneum makes possible the spread of infection with the development of peritonitis. The proximity of the pelvic tissue to the retroperitoneal allows pus to break through into the retroperitoneal space. Such a spread of the purulent process is typical for the elderly and debilitated persons with a late visit to the doctor.
Among other things, paraproctitis can be complicated by an abscess breakthrough into the rectum, vagina, and perineal skin. Usually, after a spontaneous opening of the abscess without the implementation of drainage measures, a fistulous tract is formed. If the fistula has not formed, but the focus of infection has survived, then over time a relapse occurs - the formation of a new abscess.
 The continued existence of a fistula of the rectum, especially having a complex structure of the canal (areas of infiltration, purulent cavities), contributes to a significant deterioration general condition sick. chronic course purulent process leads to cicatricial changes, deformation of the anal canal, rectum.
The continued existence of a fistula of the rectum, especially having a complex structure of the canal (areas of infiltration, purulent cavities), contributes to a significant deterioration general condition sick. chronic course purulent process leads to cicatricial changes, deformation of the anal canal, rectum.
Deformation leads to tonic insufficiency of the anal sphincter, incomplete closure anal passage, leakage of intestinal contents. Another common complication of chronic paraproctitis is pathological scarring (pectenosis) of the walls of the anal canal and a decrease in their elasticity, which leads to impaired bowel movements. A long-term fistula (more than 5 years) may become malignant.
Diagnostics
For a preliminary diagnosis of paraproctitis, a proctologist has enough data from a survey, examination and physical examination. characteristic Clinical signs: fever, local pain, symptoms of purulent inflammation. Due to the extreme pain of the procedures, digital examination of the anus and methods instrumental diagnostics proctological diseases (anoscopy, sigmoidoscopy) are not performed. When examining blood, there are signs of purulent inflammation: leukocytosis with neutrophilia, increased ESR.
Acute paraproctitis basically has to be differentiated from festering teratoma of the perirectal tissue, tumors of the rectum and surrounding tissues, Douglas space abscess. The need for additional research to differentiate paraproctitis from other diseases usually occurs in the case of a high location of the abscess (in the pelvis or ileo-rectal fossa).
The formed pararectal fistula must be differentiated from a cyst of the perirectal tissue, osteomyelitis of the terminal spine, tuberculous fistula, epithelial coccygeal tract and fistulas in patients with Crohn's disease. For differential diagnosis significant history data laboratory research, radiography of the small pelvis .
Treatment of paraproctitis
The disease requires surgical treatment. Immediately after establishing the diagnosis of acute paraproctitis, it is necessary to perform an operation to open and drain the purulent focus. Since muscle relaxation and high-quality anesthesia are important factors, complete anesthesia of the operating area is necessary. The operation is currently performed under epidural or sacral anesthesia, in some cases (with lesions abdominal cavity) are given general anesthesia. local anesthesia when opening pararectal abscesses do not produce.
During the operation, an accumulation of pus is found and opened, the contents are pumped out, after which the crypt, which is the source of infection, is found and it is excised along with the purulent passage. After complete removal the focus of infection and high-quality drainage of the abscess cavity can be expected to recover. Most challenging task is the opening of an abscess located in the cavity of the small pelvis.
In chronic paraproctitis, the formed fistula must be excised. However, surgery for the removal of the fistula during the period of active purulent inflammation is impossible. First, the existing abscesses are opened, thorough drainage is performed, only after that the fistula can be removed. In the case of infiltrated areas in the canal, a course of anti-inflammatory and antibiotic therapy, often combined with methods of physiotherapy. Surgery to remove the fistulous passage is desirable to be carried out as soon as possible, since the recurrence of inflammation and suppuration can occur quite quickly.
In some cases (old age, weakened body, severe decompensated diseases of organs and systems), the operation becomes impossible. However, in such cases it is desirable conservative methods to treat pathologies, improve the patient's condition and then perform an operation. In some cases, when the closure of the fistulous passages occurs during long-term remission, the operation is postponed, since it becomes problematic to clearly define the canal to be excised. It is advisable to operate when there is a well-visualized landmark - an open fistulous tract.
Forecast and prevention
After timely complete surgical treatment of acute paraproctitis (with excision of the affected crypt and purulent passage into the rectum), recovery occurs. In the absence of treatment or insufficient drainage, the source of infection is not removed, chronic paraproctitis occurs and the formation of a fistulous tract occurs.
Excision of fistulas located in the lower parts of the peri-intestinal space, as a rule, also leads to complete recovery. More highly located fistulas can most often be removed without complications, but sometimes long-term fistulous passages contribute to the spread of sluggish purulent inflammation into hard-to-reach anatomical formations of the small pelvis, which leads to incomplete removal of the infection and subsequent relapses. An extensive long-term purulent process can provoke cicatricial changes in the walls of the anal canal, sphincters, as well as adhesive processes in the small pelvis.
Paraproctitis is a proctological disease, which is a purulent inflammation of fatty tissue located in the perianal region and around the rectum. According to proctologists, up to 40% of patients come to the doctor for this reason, and most of the patients are male.
The cause of the inflammatory process in the pararectal region is considered to be the entry of pathological flora from the rectum into the deep layers of the surrounding cellular tissue. The main causative agents of the disease - Escherichia coli, enterococci, staphylococci, anaerobic microbes - penetrate into the fatty tissue from the rectal cavity through the recesses in the wall of the anus (anal sinuses or Morganian crypts). Morgani's crypts are the main "entrance gates" for bacteria, and most often the infection is promoted by damage to the intestinal mucosa and anal fissures.
 Other, less common, routes of entry of pathogens are wounds and ulcers on the surface of the skin, inflamed prostate. Self-infection of the body is not excluded, when bloodstream Pathogenic microorganisms are transferred to the site of inflammation from extraintestinal foci of inflammation (fungi, clostridia, mycobacteria, etc.)
Other, less common, routes of entry of pathogens are wounds and ulcers on the surface of the skin, inflamed prostate. Self-infection of the body is not excluded, when bloodstream Pathogenic microorganisms are transferred to the site of inflammation from extraintestinal foci of inflammation (fungi, clostridia, mycobacteria, etc.)
Pathogens can affect any of the cellular spaces surrounding the intestine:
- pelvic-rectal region;
- ileo-rectal tissue;
- behind-rectal zone;
- submucosal layer of the rectum;
- subcutaneous fat layer.
In severe cases, inflammation can cover several areas at once.
There are a number of factors that increase the risk of paraproctitis:
- Availability diabetes;
- atherosclerotic vascular lesions;
- weak immunity, general and local;
- frequent constipation;
- haemorrhoids;
- cracks in the anus;
- anal sex.
Types and symptoms of paraproctitis
 There are two forms of pararectal inflammation:
There are two forms of pararectal inflammation:
- sharp
- chronic
Paraproctitis is considered acute, which appeared for the first time and is characterized by the formation of suppuration in fatty tissue. Purulent contents can find a way out, forming a pathological channel between the abscess and neighboring hollow organs or the surface of the skin (fistula).
Lack of treatment or illiterate therapy translates the course of the disease into a chronic form, which is manifested by periodic relapses and captures the entire rectal space between the external and internal sphincters, the blinking sinuses and the surrounding tissue. With a long course of inflammation, persistent pararectal and perianal fistulas are formed.
 The development of the disease is accompanied by typical symptoms of the inflammatory process:
The development of the disease is accompanied by typical symptoms of the inflammatory process:
- temperature, which can reach 39 degrees;
- signs of intoxication of the body - weakness, chills, headaches, lack of appetite;
- violations of urination and defecation (pain, delay);
- pain in the area of inflammation (lower abdomen, small pelvis).
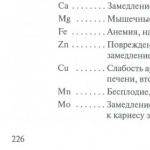
The specific clinical picture of acute paraproctitis depends on its type, that is, on the location of inflammation:

Symptoms of chronic paraproctitis
Chronic paraproctitis, as a rule, exists almost painlessly. The main manifestations of this form of paraproctitis are the formation of purulent fistulas. The outlets of fistulas can be located near the anus and on the buttocks, pus flows out of them with an admixture of feces. When the mouth of the canal is closed, pus accumulates, new abscesses develop, which break into the intestine or out, thus forming fresh fistulas. In the advanced form of the disease, purulent "moves" can form whole clusters with a branched structure, numerous holes and a common cavity - the focus of infection.
Such paraproctitis is not capable of self-healing. With every relapse the scale pathological process only increases, more and more destroying the patient's body. Gradually arise severe complications in the form of necrosis malignant degeneration paraproctitis.
Since the symptoms of acute paraproctitis are quite specific, when they are detected, it is important to contact a proctologist as soon as possible in order to avoid life-threatening consequences and to prevent the disease from becoming chronic.
Examination for illness
 Diagnosis of the disease is carried out by proctological and surgical specialists. By clinical picture and the patient's complaints, the doctor can already make a preliminary diagnosis. It is necessary to differentiate paraproctitis from festering benign tumor- "wen", tumors of the intestine, and subcutaneous form- from furunculosis.
Diagnosis of the disease is carried out by proctological and surgical specialists. By clinical picture and the patient's complaints, the doctor can already make a preliminary diagnosis. It is necessary to differentiate paraproctitis from festering benign tumor- "wen", tumors of the intestine, and subcutaneous form- from furunculosis.
Manual and instrumental examination, sigmoidoscopy and other procedures are usually not performed because they are very painful. If necessary, these manipulations are done under anesthesia already directly on the operating table.
In case of difficulties with the diagnosis, an ultrasound of the perineum with a rectal sensor is additionally prescribed, computed tomography, x-ray to detect tumors and fistulas (fistulography).
 Paraproctitis is a surgical disease, that is, its treatment is carried out mainly by surgery. "Acute" patients are sent to the operating room on an emergency basis, immediately after the diagnosis. The task of the surgeon with paraproctitis is to open the abscess, clean the cavity from the contents, and install drainage. The procedure is carried out under general anesthesia or epidural anesthesia. Carried out exfoliation of the abscess does not guarantee that the recurrence of the disease will not occur, since such an operation does not eliminate the root cause of paraproctitis. Therefore, most often, after 5-7 days, a second intervention is carried out, already in order to remove the affected glands and sinuses. Such an operation is called multi-stage.
Paraproctitis is a surgical disease, that is, its treatment is carried out mainly by surgery. "Acute" patients are sent to the operating room on an emergency basis, immediately after the diagnosis. The task of the surgeon with paraproctitis is to open the abscess, clean the cavity from the contents, and install drainage. The procedure is carried out under general anesthesia or epidural anesthesia. Carried out exfoliation of the abscess does not guarantee that the recurrence of the disease will not occur, since such an operation does not eliminate the root cause of paraproctitis. Therefore, most often, after 5-7 days, a second intervention is carried out, already in order to remove the affected glands and sinuses. Such an operation is called multi-stage.
If the location of the abscess is precisely known, the surrounding tissues are not involved in the inflammatory process and the patient's condition allows, all of the above manipulations are performed at a time. During a one-stage operation, it is necessary not only to open the abscess, but also to find the source of infection, remove the affected crypt, and cut out fistula passages. Deep-seated abscesses often require cutting the sphincter (sphincterotomy), which poses a certain risk of damage to the anus's locking mechanism. As a result, the patient may develop fecal incontinence.
If the process is already chronic stage, a planned radical operation is necessary, during which all affected tissues, fistulas will be eliminated and conditions will be created for the normal healing of the postoperative wound. For the treatment of chronic paraproctitis, the following types of surgical interventions are used:

The type and extent of the operation is determined by the surgeon-proctologist based on information about the location and severity of the inflammatory process.
IN postoperative period prescribe antibiotic therapy (Gentamicin, Tsufotaxime) and make dressings with antiseptics (Levomekol). Recovery takes place within 2-5 weeks, all this time the patient must comply strict diet, do sitz baths with potassium permanganate 3-4 times a day and follow other recommendations of the surgeon.
Prevention of acute and chronic paraproctitis
 The main task after recovery is to prevent the recurrence of paraproctitis. Prevention consists of the following measures:
The main task after recovery is to prevent the recurrence of paraproctitis. Prevention consists of the following measures:
- a diet that ensures the establishment of regular light stools;
- maintaining optimal weight;
- getting rid of hemorrhoids and;
- meticulous hygiene, washing with cool water after each bowel movement;
- destruction of chronic foci of infection in the body;
- treatment of major diseases (diabetes mellitus, atherosclerosis, diseases gastrointestinal tract etc.)
When unpleasant, and often pain in the region of the rectum. However, by the time the decision to visit a doctor is made, the disease often takes launched form. Such a critical form of proctological diseases is purulent paraproctitis.
Folk remedies can treat various diseases
In order to save the patient from inflammatory processes, the abscess must be opened, washed and rid of the accumulated pus. Also, in the event that the paraproctitis was severely neglected, in addition to washing and drainage (removal of pus), it is necessary to perform a procedure for cleaning the fistula - a purulent passage that occurs when there are especially neglected abscesses. This procedure is extremely delicate, requiring the execution of an experienced specialist.
It should be remembered that an untimely visit to a doctor with an advanced case of paraproctitis threatens the patient with destruction of the wall of the rectum or urethra.
Symptoms of paraproctitis and its forms

Surgical treatment of paraproctitis
Fast developing disease requires immediate contact with a specialist doctor if you find yourself experiencing symptoms such as:
- (its manifestations can be fever, general weakness, headaches, body aches and loss of appetite)
- Constipation and when trying to go to the toilet
- Pain is also accompanied by the urination process.
- Causeless occurrence of foci of pain and swelling in the anus.
In addition to the listed main symptoms, there are private signs that accompany the following forms of paraproctitis:
- Spicy. It is characterized by pronounced manifestations of the main symptoms listed above, however, it requires an individual selection of treatment
- Chronic. Characterized by the occurrence of a fistula that destroys the walls small intestine and requires immediate surgery followed by regular drainage
- Purulent. Not just an abscess is formed, but a whole cavity filled with pus. To prevent the occurrence of a fistula, immediate action is required
- Ischiorectal. The abscess itself is located in a deep layer of pararectal tissue (located under the skin), which makes this form of paraproctitis difficult to diagnose. Many symptoms of ischiorectal paraproctitis are often mistaken for a respiratory infection.
Thus, almost every form of paraproctitis can be taken as an ordinary one. viral infection or one of the manifestations of hemorrhoids, not only by the patients themselves, but also by doctors. A thorough examination by a qualified specialist using a rectal speculum, as well as an ultrasound procedure, will help to avoid the serious consequences of such an error.
Paraproctitis: treatment

Folk remedies should be used with caution!
A disease such as paraproctitis, in most cases, requires surgical intervention. The doctor is obliged to send the patient to the operating room immediately after confirming the diagnosis. There, the patient will be opened abscess and drained.
In addition to draining the purulent focus, during the operation, the crypt, which is the source of infection, is excised, and in especially advanced, acute cases of paraproctitis, the fistula is also excised, after which the procedure will be considered finally completed.
In the event that there were infiltrated areas in the canal, it would be appropriate to prescribe a course of anti-inflammatory and antibacterial therapy in the preoperative period, but even in this case, surgical intervention should by no means be postponed for a long time. However, in some cases, the operation is not possible. These are cases like:
- Fairly old age
- Severe weakness of the body
- Decompensated diseases of internal organs.
Treatment of the disease with folk remedies

Folk remedies are more effective on early dates diseases
Often in the event that it is undesirable to operate on paraproctitis for one reason or another, patients resort to means traditional medicine. And in the event that the disease has not yet acquired sharp shape, similar treatment may have a positive effect.
Treatment of paraproctitis tested by many generations folk remedies in the early stages of the disease, it often helps to avoid opening the abscess by a doctor, allowing it to open spontaneously. However, even in this case, you need to see a doctor in order to treat the bursting abscess, remove the pus and excise the fistula.
There are several ways to treat paraproctitis at home: using therapeutic baths, and using special medicinal teas. Among the most effective bath solutions are:
- Bath with brine to relieve inflammation and reduce pain. To prepare it, you need to take 1 tbsp. l. salt and 1 tbsp. l. soda, mix and dilute in 5 liters. distilled water.
- The course of treatment is 15 procedures, after each of which it is recommended to use the ointment prescribed by the doctor.
- Mummy solution. To prepare this composition, you will need 200 ml boiled water and 10 tablets of mummy. The expressed solution must be dissolved in five liters of boiled warm water.
- The procedure is also effective, in which a mixture of 2 liters of warmed milk, 2 onions and 5-6 cloves of garlic is used as a bath. The mixture must be boiled for 3-4 minutes, then cool thoroughly. When taking this bath, you need to ensure that the patient's body is warm.

Treatment of paraproctitis with folk remedies should be carried out under the supervision of a doctor!
Microclysters and tampons impregnated with special compounds have a positive effect both on their own and in combination with treatment with baths:
- A solution of 100 ml of water and 1 tbsp. l. mix honey with separately prepared infusion of sage, chamomile and yarrow. Inject 40 ml immediately after the cleaning procedure.
- Squeeze the juice of a small, well-peeled potato and inject with an enema, 1 tbsp. l. in 10 days. The procedure is preferably performed before going to bed.
Strengthen the body and relieve discomfort healing infusions and teas help:
- You can brew a collection of plantain leaves, yarrow and marshmallow root and apply 4 times a day, 150 ml each.
- Pour 3 liters. boiling water 3 grams stone oil and insist for 3 days. Take 200 grams after each meal, if the body perceives such an infusion well.
Paraproctitis is a disease that is extremely dangerous and brings a lot of inconvenience. And, as you know, it is easier to avoid it than to cure it completely. In order not to encounter paraproctitis, it is necessary to drink enough fluids, and lead a healthy, mobile lifestyle.
How to behave with an "uncomfortable" illness, the video will tell:
Tell your friends! Tell your friends about this article in your favorite social network using social buttons. Thank you!